Mohamed Hany, Abdelrahman Helmy, Ziyu Liu*, Bruna Menezes Gomes, Morgan Lacken, Sahir Ijaz, Raul Mederos
Hialeah Hospital, General Surgery, 651 East 25th St., Hialeah, FL 33013, United States
*Corresponding Author: Ziyu Liu, Hialeah Hospital, General Surgery, 651 East 25th St., Hialeah, FL 33013, United States.
Abstract
Introduction
Trocar-site hernias (TSH) after a robotic procedure could potentially lead to severe complications involving bleeding, severe pain, and incarceration giving rise to bowel obstruction that requires immediate intervention. In this report, we present a case of incarcerated TSH following a robotic hysterectomy, which was reduced robotically 6 days after the initial surgery.
Case Summary
A 47-year-old female who had a robotic hysterectomy 6 days prior presented to the Emergency Department with worsening symptoms of indigestion, heartburn, projectile vomiting, and persistent abdominal pressure. The previous surgery implemented a 12-mm trocar but left the fascia unclosed upon finishing. CT showed proximal bowel obstruction. An incarcerated ventral TSH in the left lower quadrant abdomen was diagnosed. The patient underwent a robotic repair at the herniated trocar site and was discharged without complications.
Discussion
We suspect that the major risk factors leading to TSH in this patient are longer operation hours, excessive manipulation of the trocar during the procedure, not closing the fascial defect upon finishing, large trocar, and anemia. The bowel obstruction induced by TSH could soon progress into a strangulated or incarcerated hernia, which drastically increases the patient’s mortality and morbidity and, therefore, needs emergent reoperation.
Conclusion
Surgeons should be aware of the potential for reoperation and readmission. Key risk factors include using large trocars (10mm or larger), excessive intraoperative manipulation, and failing to inspect and close fascial incisions. Adhering to these practices can reduce TSH incidence and improve patient outcomes.
Keywords: Case report, Incarcerated hernia, Incisional hernia, Trocar-site hernia, Abdominal wall, Robotic-assisted incisional hernia repair
Introduction
Incisional hernia, a form of ventral hernia, is defined as abdominal wall hernias at the site of a previous surgical incision [1]. With an estimated prevalence of 0-35%, incisional hernias are the most frequent complication related to surgical procedures [2]. The incorporation of minimally invasive procedures in routine surgical practice has resulted in some specific complications, including incisional hernia at trocar sites.
Trocar-site hernia (TSH) can be asymptomatic, but it occasionally presents with bowel obstruction requiring emergency surgery [4]. The onset of the symptoms, such as nausea, vomiting, abdominal pain, and mass, can start in a few days or only several months after surgery [13]. Most research on trocar-site hernias has come from laparoscopic experience; the incidence has been reported to range from 0.0 to 5.2% for all procedures [5].
Present research indicates that repairing an incisional hernia can be achieved through either an open or laparoscopic approach, with both methods demonstrating comparable results [19]. With advancing surgical technology, minimally invasive approaches to abdominal surgeries have been preferred over the open technique due to the lower incidence of incisional hernias, decreased blood loss, early recovery, decreased postoperative pain, and shorter hospital stays associated with minimally invasive surgeries [3].
Here, we discuss a case of trocar-site incarcerated ventral hernia 6 days following a robotic hysterectomy that was robotically repaired.
Presentation of Case
A 47-year-old female (G3P3), with a past medical history significant for menorrhagia, adenomyosis and leiomyoma was indicated to have a total robotic hysterectomy.
Robotic hysterectomy involved the introduction of four trocars; two 8 mm trocars were placed on the left and right lower quadrants 10 cm from the umbilicus and 2 cm above the anterior superior iliac spine. Another 8 mm trocar is placed 3 cm above the umbilicus serving as the camera port and a fourth 12 mm trocar was placed between the camera port and the left lower quadrant port. Uterus was delivered vaginally with approximately 100 cc blood loss and no complications. Abdominal incisions were closed with 3-0 Monocryl and larger ports with subcutaneous Vicryl. The patient was discharged the following day in good condition. However, none of the trochar-site fasciae was closed.
On postoperative day 5, the patient called to report persistent abdominal pressure, indigestion, and heartburn. Later that afternoon, the symptoms progressed to include vomiting. She described the excretions as a thin yellow liquid, and the sensation felt different than previous GI illnesses she experienced. The on-called doctor suspected it to be related to gastritis or gastroenteritis and was discharged on analgesics and ondansetron.
On postoperative day 6, the patient called again to report that her symptoms were getting worse, and she was instructed to report to the emergency room for evaluation, given concern for a possible bowel obstruction.
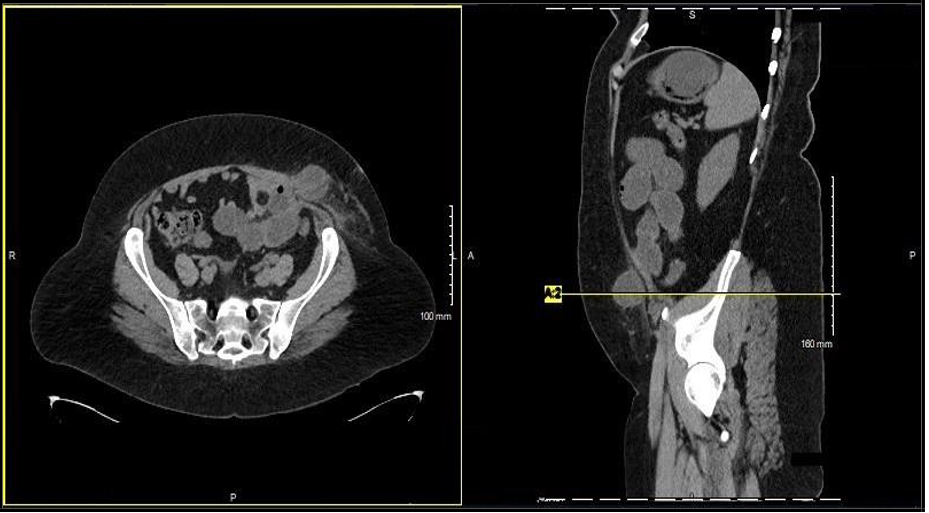
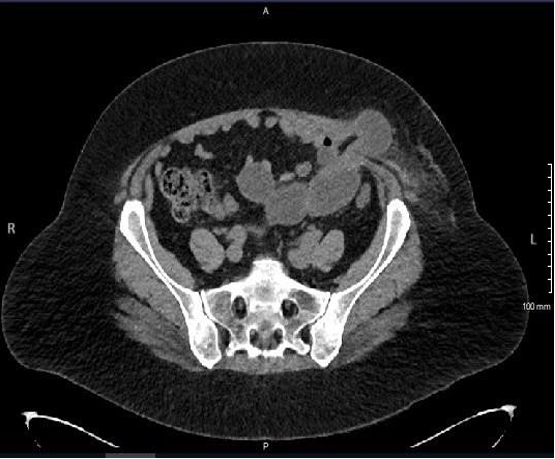
Physical exam in the emergency department noted an obese female patient with a mildly distended abdomen, tenderness and induration in the left lower quadrant, however the hernia was not detected on physical examination and surgical incision sites were clear of any drainage or signs of infection. Following a thorough evaluation of the patient's clinical manifestation marked by abdominal pain, nausea, and vomiting, given her recent history of robotic-assisted hysterectomy 6 days ago, TSH was highly suspected. An erect A/P X-ray was ordered, showing multiple air-fluid levels in the bowel, and the definitive diagnosis was ascertained by the abdominopelvic CT scan shown in (Figure 2 A & B and Figure 3). The imaging unveiled the herniation of bowel loops through the abdominal wall, specifically localized to the left lower quadrant, notably at the 12 mm trocar insertion site. Additionally, the findings indicated stomach distension and proximal small bowel dilation proximal to the site of hernia and decompression of the distal bowel, confirming incarceration, bowel obstruction, and the necessity for reoperation. The patient was emergently taken to the operating room, where a 5 mm Visiport camera was introduced into the right upper abdominal quadrant, followed by the insertion of three 8 mm trocars: two of them at the level of the umbilicus on contralateral midclavicular lines, with the final just inferior to the umbilicus. The da Vinci robotic system was docked, and inspection of the abdominal cavity revealed proximal small bowel dilation with herniated small bowel in the left lower quadrant (Figure 1). Herniated contents were carefully reduced using gentle traction, and the intestine was viable. The defect was noted to be approximately 2 cm. Primary repair followed by reflecting the surrounding peritoneum inferiorly and approximating the fascia with a #1 Stratafix suture. The same peritoneum was then reflected superiorly and sutured together to provide complete coverage of the defect. Trocar site wounds were approximated using 4-0 Vicryl with Steri Strips on top.
The patient's postoperative recovery was uneventful. She was educated in postoperative care, medication/diet, and the follow-up schedule and discharged home on postoperative day two.
Figure 1: The da Vinci robotic system was docked, and inspection of the abdominal cavity revealed proximal small bowel dilation with herniated small bowel in the left lower quadrant
Figure 2 A & B: X-ray showing multiple air-fluid levels in the bowel
Figure 3: The abdominopelvic CT scan
Discussion
Trocar site hernia (TSH) following gynecological laparoscopy was first reported in 1968 [6]. The true incidence of trocar site hernias following laparoscopic procedures is not known and is stated by some studies that it is even underestimated. However, a systematic review and meta-analysis showed that the incidence of incisional hernias following laparoscopic surgeries compared to open abdominal surgeries was 4.3 % vs 10.1 % (p =0.002) and is attributed mainly to smaller fascial defects [7].
Other estimates for trocar site hernia following laparoscopic procedures ranging from 0.2% to 1.3% have been determined across all surgical subspecialties based on the largest available studies [8, 9, 10, 11, 4].
A retrospective review of gynecological robotic surgeries, including 500 patients stated that the incidence of trocar site hernias was 0.6%. This incidence is similar to reported trocar site herniation following laparoscopy despite the fact that robotic surgeries require larger ports (8mm vs 5 mm) [12]. Additionally, an incidence as low as 0.016% has been determined in another retrospective study evaluating the incidence of TSH in 55,244 patients over 20 years following gynecologic laparoscopic procedures [13]. It is also worth noting that a study in 2016 stated that surgeons believed the rate of trocar site hernia to be between 0.5% and 5%. However, the same study revealed that the documented incidence in the literature varied more widely, ranging from 0% to 39.3%. This wide variation suggests a notable underestimation by surgeons of the incidence of TSH and emphasizes the need for further studies to determine the true incidence of TSH [14].
Multiple risk factors have been identified for trocar site hernia. These include pyramidal trocars, a long duration of surgery, manipulation of the trocar, closure of the fascia at the time of surgery, and umbilical location. Patient-specific risk factors were also reported, including age, obesity, patient history of kidney failure, anemia, smoking, steroid treatment, diabetes, and COPD. The most cited risk factor was the trocar size. Many of the reported trocar site herniations involve a port size of at least 10 mm, and only a few cases are reported at trocar sites smaller than 10 mm in adult surgery, with only one at a 3-mm port site [2, 12, 15].
Another report of a similar case of TSH following robotic-assisted Sacro-colpopexy mentioned that there is no current evidence that has clearly shown that the risk for TSH is operation-specific. However, the length of the operation and excessive manipulation have been linked to an increased risk for TSH, mostly due to peritoneal and/or fascial extension. The study mentioned other important risk factors, including the technique associated with port placement and the associated risk of port tracking during insertion, which may lead to widening of the peritoneal and or fascial defects, especially with the use of valveless endoscopic dynamic pressure system [16].
Regarding our case, the patient had multiple of the aforementioned risk factors, including obesity, anemia, and the use of a 12 mm trocar placed 5 cm from the midline in the left lower quadrant. This is an unusual site for TSH as the most common site of TSH according to a systematic review that included 30,568 patients is in the umbilicus region representing 82% of cases [9]. Other risk factors that this patient had were the long duration of surgery and excessive manipulation of the trocar during dissection, which may have caused the extension of the fascial defect. Not closing the fascial defect was also potentially one of the contributing factors to the development of TSH, although it is routine for surgeons not to close the fascial defects after gynecological operations.
Three categories of trocar site herniations have been outlined: (1) separation of fascial and peritoneal layers (linked with early-onset), as observed in our case, (2) fascial separation with an intact peritoneum (linked with a delayed-onset), and (3) herniation of the entire abdominal wall (evident during trocar removal or shortly after surgery) [11]. Early onset is the most frequently documented and usually becomes evident within 2 to 12 days following surgery. Individuals experiencing early-onset hernias typically exhibit symptoms of small bowel obstruction, a condition that may require urgent surgical intervention, often leading to the necessity of a reoperation. [11]. There have been documented cases of bowel resection required as a result of an incarcerated hernia [15, 17]. Additionally, a review of 30 case reports on trocar site herniation revealed a 17% (5/30) occurrence of TSH requiring bowel resection when emergent reoperation was conducted [11]. This shows the significant risk associated with TSH on both patient morbidity and mortality.
When omentum, as opposed to the bowel, is the herniating tissue, patients usually present later and with minimal symptoms [11,18]. This might also be one of the factors leading to underdiagnosis and decreased incidence of TSH.
Conclusion
While uncommon, trocar site hernias (TSH) following robotic surgeries pose a significant risk and surgeons performing robotic surgery should be aware of the possibility of reoperation and readmission, despite the low prevalence of these conditions. This study emphasizes the importance of recognizing TSH as a major, often underdiagnosed, complication of minimally invasive procedures, including laparoscopic gynecological surgeries. The true incidence of TSH is not well-documented in the literature, contributing to its underdiagnosis. Key risk factors identified include the use of large trocars (10mm or larger), excessive manipulation during surgery, and failure to inspect and close fascial incisions. Surgeons should minimize these risks by choosing appropriate trocar sizes, reducing intraoperative manipulation, and ensuring all fascial defects are thoroughly closed at the procedure's end. Adhering to these practices can reduce TSH incidence and improve patient outcomes.
Conflict of Interest: There are no conflicts of interest or financial disclosures to report.
Funding: There are no sources of funding for this case report.
Consent: Verbal consent was obtained from the patient for publication of this case report and accompanying images.
References
- Hope WW, Tuma F (2023) Incisional Hernia. 2023 Jun 12. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
- Ciscar A, Badia JM, Novell F, Bolívar S, Mans E (2020) Incidence and risk factors for trocar-site incisional hernia detected by clinical and ultrasound examination: a prospective observational study. BMC Surg. 20(1): 330.
- Aarts JW, Nieboer TE, Johnson N, Tavender E, Garry R, et al. (2015) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2015(8): CD003677.
- Swank HA, Mulder IM, la Chapelle CF, Reitsma JB, Lange JF, et al. (2012) Systematic review of trocar-site hernia. Br J Surg. 99(3): 315-23.
- Damani T, James L, Fisher JC, Shah PC (2021) Incidence of acute postoperative robotic port-site hernias: results from a high- volume multispecialty center. J Robotic Surg. 15(3): 457–463.
- Fear RE (1968) Laparoscopy: a valuable aid in gynecologic diagnosis. Obstet Gynecol. 31(3): 297-309.
- Kössler-Ebs JB, Grummich K, Jensen K, Hüttner FJ, Müller-Stich B, et al. (2016) Incisional Hernia Rates After Laparoscopic or Open Abdominal Surgery—A Systematic Review and Meta- Analysis. World Journal of Surgery. 40(10): 2319-30.
- Nezhat C, Nezhat F, Seidman DS, Nezhat C (1997) Incisional hernias after operative laparoscopy. J Laparoendosc Adv Surg Tech A. 7(2): 111-5.
- Helgstrand F, Rosenberg J, Bisgaard T (2011) Trocar site hernia after laparoscopic surgery: a qualitative systematic review. Hernia. 15(2): 113-21.
- Kadar N, Reich H, Liu CY, Manko GF, Gimpelson R (1993) Incisional hernias after major laparoscopic gynecologic procedures. Am J Obstet Gynecol. 168(5): 1493-5.
- Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M (2004) Trocar site hernia. Arch Surg. 139(11): 1248-56.
- Clark LH, Soliman PT, Odetto D, Munsell MF, Schmeler KM, et al. (2013) Incidence of trocar site herniation following robotic gynecologic surgery. Gynecol Oncol. 131(2): 400-3.
- Zhu YP, Liang S, Zhu L, Sun ZJ, Lang JH (2019) Trocar-site hernia after gynecological laparoscopic surgery: a 20-year, single- center experience. Chin Med J (Engl). 132(22): 2677-2683.
- Holihan JL, Chen JS, Greenberg J, Hehir D, Johnston SM, et al. (2016) Incidence of Port-Site Hernias: A Survey and Literature Review. Surg Laparosc Endosc Percutan Tech. 26(6): 425-430.
- Moreaux G, Estrade-Huchon S, Bader G, Guyot B, Heitz D, et al. (2009) Five-millimeter trocar site small bowel eviscerations after gynecologic laparoscopic surgery. J Minim Invasive Gynecol. 16(5): 643-5.
- Badiner N, Sansone S, Fenster T, Segal S (2021) Incarcerated ventral wall hernia after robotic urogynecologic surgery: A case report. Case Rep Womens Health. 32: e00350.
- Spaliviero M, Samara EN, Oguejiofor IK, DaVault RJ, Albrecht RM, et al. (2009) Trocar site spigelian-type hernia after robot- assisted laparoscopic prostatectomy. Urology. 73(6): 1423.e3-5.
- Coda A, Bossotti M, Ferri F, Mattio R, Ramellini G, et al. (2000) Incisional hernia and fascial defect following laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 10(1): 34-8.
- Al Chalabi H, Larkin J, Mehigan B, McCormick P (2015) A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg. 20: 65-74.