Grażyna Piotrowicz1, Artur Antolak2, Daria Gąsiorowska1*, Łukasz Dorosz1, Adam Piotrowicz1
1 Department of Gastroenterology, Hospital of Ministry of the Interior and Administration, Gdańsk, Poland
2 Laboratory of pathomorphology, ALAB PLUS Sp. zo.o., Gdańsk
*Corresponding Author: Daria Gąsiorowska, Department of Gastroenterology, Hospital of Ministry of the Interior and Administration, Gdańsk, Poland
Abstract
We report a case of a 64-year-old man with COVID -19 and severe bleeding from gastrointestinal tract. The only changes visible at that time were the erosions in the rectum due to intestine inflammation. It is estimated that gastrointestinal symptoms are reported in approximately 17.6% of COVID- 19 patients. Gastrointestinal bleeding as a consequence of colitis is a rare symptom but very significant for the final outcome due to its potential mortality. Moreover, the occurrence of symptoms from the gastrointestinal tract is also the cause of the delay in admission to hospital compared with people with respiratory symptoms only (9 vs7.3 day). To correctly diagnose patients healthcare professionals should be aware of gastrointestinal complications associated with SARS-COV-2 infection and that is the aim of this case presentation.
Keywords: bleeding, COVID-19, inflammation
Introduction
At the end of December 12, 2019 pneumonia induced by coronarovirus began spreading in Wuhan, China and the disease has been named by WHO as COVID-19. The coronarovirus itself has been identified as Severe Acute Respiratory Distress Coronarovirus Syndrome 2 (SARS-COV-2). SARS-COV-2 is transmitted by direct contact, by air, through aerosols and during medical procedures. The presence of the virus is found in the respiratory tract, saliva, faeces and urine and possibly in tears as well. Virus transmission depends on the receptor binding domain and the ACE 2 receptor which is represented not only in respiratory tract but also on the surface of epithelial cells of the stomach, small intestine and large intestine. Gastrointestinal symptoms unlike infections with other coronaroviruses, may appear earlier and may worsen the course of the disease or they may be isolated and thus delay diagnosis. The most common gastrointestinal symptoms are anorexia (39.9-59.2 %) and diarrhea (2-49.5 %). Gastrointestinal bleeding as a consequence of colitis is a rare symptom estimated at 4-13.7 %. [1,2,3].
There are various mechanism that lead to the intestinal inflammation. In intestinal epithelial cells ACE 2 is needed to maintain amino acid homeostasis and production of antimicrobial peptide influencing the ecology of the intestinal microbiota, therefore reduction of this receptor increases the risk of inflammation. Inflammation in the digestive tract may be caused also by direct damaging action of the virus and/or immune response causing intestinal symptoms. The inflammatory response to the damaging effect of the virus leads to the recruitment of helper T cells, cytokine storm and organ damage. Histopathology shows lymphocyte, monocytes and plasma cells infiltrates, Finally the inflammatory process may lead to the erosins of the mucosa and bleeding from the gastrointestinal tract. [4]
Case presentation
A 64-year-old man with COVID -19 with prior history of persistent insulin-dependent diabetes, atrial fibrillation (treated with Xarelto), hypertension was admitted to the hospital in severe general condition with impaired consciousness, nausea, vomiting, additionally with distended abdomen with preserved peristaltics upon admission.
Mucosal dryness and tachycardia were noticeable, 120 bpm, tachypnea about 30 bpm, SpO2 saturation 95 %. In laboratory tests there were found: hyperglycemia 800 mg %, blood acidosis pH 7.014, increased CRP value up to 12 mg/l, rised level of leukocytes in the peripheral blood 23.78 G/L with neutrocytosis 78.5 % and lymphocytosis,13.7 %, INR 2.66, prerenal failure with GFR 33 ml/min. Slight increase of aminotransferase was observed throughout the hospitalization.
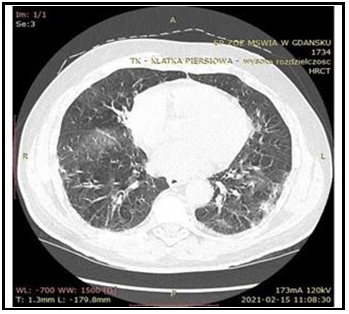
In the chest CT typical changes for COVID-19 were found covering about 25 % of the lung parenchyma (Figure 1).
Figure 1: The chest CT with typical changes for COVID-19 covering about 25 % of the lung parenchyma
Due to orientation disorders CT of the head was performed, showing numerous ischemic stroke foci in central nervous system with accompanying cerebral edema (Figure 2).
Figure 2: The CT of the head showing numerous ischemic stroke foci in the central nervous system with accompanying cerebral edema
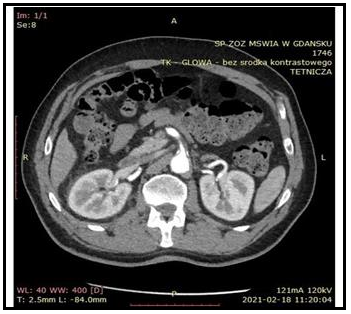
The abdominal CT scan showed a fluid lesion in the spleen, 36mm in size with a septum and a clot in the superior mesenteric artery (Figure 3).
Figure 3: The abdominal CT scan with a clot in the superior mesenteric artery
The treatment included fluid therapy, insulin infusion, steroid therapy, low molecular weight heparin, antibiotics and additionaly also oxygen therapy due to periodic desaturation up to 88 %.
During the entire hospitalization attention was drawn to leukocytosis which increased up to 30,000, neutrocytosis and lymphopenia up to 3 % in the peripheral blood smear, increase in CRP to 134 mg/dl and progressive decrease in saturation to 88 %.
Persistent hyperglycemia to 200 mg % and compensated metabolic acidosis with persistent significant base deficiency to 8-11mmol /l was observed. Renal parameters were normal but with accompanying compensatory diuresis.
On the eighth day of the hospitalization there was a massive bleeding from the gastrointestinal tract with a decrease in hemoglobin of 5 g/dl, accompanied by symptoms of hypovolemic shock. The patient required a transfusion of 10 µL of Red Cell Concentrate.
Endoscopic examinations performed after the patient's condition was stabilized revealed: redness of the mucosa in the antral part of the stomach with single erosions in gastrofiberoscopy. In colonoscopy with intubation of the ileum: normal stool, large amounts of blood in the large intestine mainly in the left half with numerous rectal erosions (Figure 4).
Figure 4: Numerous rectal erosions in colonoscopy
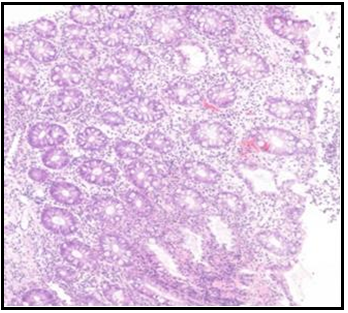
The histopathological evaluation of the specimens revealed: lymphocytes. plasmocytes and neutrophils infiltrates (Figure 5).
Figure 5: Histopathological evaluation of the specimens taken during colonoscopy (lymphocytes. plasmocytes and neutrophils infiltrates)
Enteral nutritional treatment was used combined with probiotics. After 4 days the bleeding from gastrointestinal tract subsided, no further decrease in hemoglobin level was observed.
Discussions
The most propable cause of hematochezia in presented case was colitis due to SARS-COV-2 infection. However, other causes should not be ignored here.
Firstly, it could be tissue hypoxia with loss of cell integrity and eventually their death due to respiratory failure. [2] In presented case there where pulmonary changes found in chest CT of our patient accompanied by periodic desaturation up to 88 %
Secondly, it could be the result of drugs commonly used to treat COVID -19: antibiotics, NSAIDs, corticosteroids [2]. Our presented patient had all of those risk factors like and drug therapy for COVID-19.
Thirdly, it should be remembered that COVID-19 is associated with an increased risk of thrombosis, neurological symptoms, ischemic and haemorrhagic strokes and cardiac injuries, but also skin (20 %) and eye symptoms. [3] In the presented case our patient apart from neurological symptoms due to ischemic stroke (numerous ischemic foci in central nervous system fouund in head CT) had a wall clot in the superior mesenteric artery revealed in abdominal CT.
Conclusions
Being aware of possible gastrointestinal complications in patients with COVID-19 one question may be asked – what can be done to reduce those consequences among which there may be a severe bleeding?
It is evident that the gut microbiome influences the immune response of the respiratory tract and infections in the respiratory tract causes changes in the intestinal microflora. In people with impaired function of the intestinal microbiota and with accompanying infection with SARS- COV- 2 additionally occurs the change in microbial composition, which can lead to an increase in the level of cytokines and to aggravated immune response. The intestinal microflora influences the expression of the ACE2 receptor therefore the use of probiotics and prebiotics can help restore the normal microflora and should be considered as supportive treatment. Adequate consumption of vitamine A, vitamine D, proteins and branched fatty acids can increase the production of antibodies as in the case of an anti-inflammatory diet based on the appropriate fiber intake, which reduces the risk of death caused by the infection in the digestive tract or in respiratory tract [6,7].
In case of symptomatic diarrhea due to the increased expression of the ACE 2 receptor in the intestine and the disturbance of the normal intestinal flora caused by SARS- COV- 2 invasion, the enteral nutrition is a preferred method of nutritional treatment as the lack of contact with a nutrient by intestine epithelium may lead to the atrophy of the lymphoid tissue, weakening of the immune system and translocation of bacteria. Nutritional goals are achieved by combining enteral nutrition with oral one in the case of conscious persons and enteral nutrition into the small intestine in the case of people undergoing mechanical ventilation.
A high-calorie and high-protein diet of 1500-2000 kcal/day is recommended for maintenance of metabolic functions. To achieve those nutritional goals it should be given within 24-48 hours. Sometimes achieving required caloric balance requires combining with parenteral nutrition. [8].
Abbreviations:
COVID -19- coronavirus disease 2019,
SARS-COV-2- Severe Acute Respiratory Distress Coronarovirus Syndrome 2,
WHO - World Health Organization,
ACE 2 - Angiotensin-converting enzyme 2,
BPM-Beats per minute,
BPM – Breaths per minute,
SpO2- Peripheral oxygen saturation,
CRP-C-reactive protein ,
INR-International normalized ratio,
GFR- Glomerular filtration rate,
CT- Computed tomography,
NSAIDs-Non-steroidal anti-inflammatory drugs
Declarations:
Conflict of interest: none declared , no funding to declare, patient consent for publication.
Authors contribiution: G.P., D.G, Ł.D and A.P where writing this paper together equally. A.A. worked on tissue specimens and made the tissue figure.
Acknowledgements: not applicable
References
- Umakanthan S, Sahu P, Ranade AV, Bukelo MM, Rao JS, et al. (2020) Origin, transmision, diagnosis and management of coronarovirus disease 2019 (COVID-19). Postgrad Med. J. 96(1142): 753-758.
- Galanopoulos M, Gkeros F, Doukatas A, Karianakis G, Pontas C, et al. (2020) COVID-19 pandemic:Pathophysiology and manifestations from the gastrointestinal tract. World J Gastroenterol. 26(31): 4579-4588.
- Patel KP, Patel PA, Vunnam RR, Hewlett AT, Jain R, et al. (2020) Gastrointestinal, hepatobilary, and pancreatic manifestations of COVID-19. J Clin Virol. 128: 104386.
- Ye Q, Wang B, Zhang T, Xu J, Shang S (2020) The mechanism and treatment of gastrointestinal symptoms in patients with COVID-19. Am J Physiol Gastrointest Liver Physiol. 319(2): G245-G252.
- Gao Z, Xu Y, Sun C, Wang X, Guo Y, et al. (2021) A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect. 54 (1): 12-16.
- Kariyawasam JC, Jayarajah U, Riza R, Abeysuriya V, Seneviratne SL (2021) Gastrointestinal manifestations in COVID-19. Trans R Soc Trop Med Hyg. 115(12): 1362-1388.
- Carvalho A, Alqusairi R, Adams A, Paul M, Kothari N, et al. (2020) SARS-COV-2 Gastrointestinal Infection Causing Hemorrhagic Colitis: Implications for Detection and Transmission of COVID-19 Disease. Am J gastroenterol. 115(6): 942- 946.
- T Toubasi AA, AbuAnzeh RB, Khraisat BR, Al-Sayegh TN, AlRyalat SA (2021) A meta-analysis: Proton pump current use and the risk of Coronarovirus Infectious Disease 2019 development and its related mortality. Archives of Medical Research. 52(6): 656-659.
- Aguila EJT, Cua IHY, Fontanilla JAC, Yabut VLM, Causing MFP (2020) Gastrointestinal manifestations of COVID-19: Impact on Nutrition Practics. Nutr Clin pract. 35(5): 800-805.