Ale J. Hejase1, Hussin J. Hejase2*
1Adnan Kassar School of Business (AKSOB), Lebanese American University, Beirut, Lebanon
2Basic and Applied Sciences Research Center, Al Maaref University, Beirut, Lebanon; IEEE Senior Member
*Corresponding Author: Hussin J. Hejase, Basic and Applied Sciences Research Center, Al Maaref University, Beirut, Lebanon; IEEE Senior Member.
Abstract
The cost and affordability are significant factors in numerous healthcare systems. Worries may result in limitations on using costly medications and effective treatments. This research aims to investigate the awareness and attitude of 307 Lebanese citizens towards the affordability of new expensive medicines versus individuals' economic status. It also explores respondents' actions when faced with the unaffordability of new medications. A survey is administered to a convenient sample of Lebanese citizens based on their willingness to participate. The necessary ethical measures were applied to data acquisition and confidentiality promised including no identity being public and respondents can quit the exercise with no questions asked. Descriptive analysis was performed using IBM SPSS software. Findings show that 86.2% of respondents believe that low-income individuals become even poorer as they cover health costs out of their pockets; 88.9% agree that family savings will be depleted because of elevated healthcare costs; and 78.1% believe that elevated medication prices ought to encourage people to sell their assets to preserve the lives of their loved ones. Ultimately, the profound essence of sacrifice, or relinquishing what an individual deems crucial for their welfare, is illustrated in that 80.7% of respondents stated that they would consider selling their homes to protect the life of a relative. Results shall form an informed platform for related stakeholders in the healthcare system and to officials of the Ministry of Health (MOH), concerned researchers, and professionals in pharmaceutics dealing with particular expensive medications.
Keywords: Healthcare, medications, affordability gap, decision-making, Lebanon
Introduction
A major work by the National Academies of Sciences, Engineering, and Medicine. (2018) [52] posits that "The significant expense of healthcare has long been a challenge for patients, their families, and society in general. Individuals with long-term health issues are at a higher risk because their ailments or the therapies for their ailments hinder their capacity to hold a job, resulting in some individuals completely losing their jobs. These people often accumulate large financial debt and exhaust the resources required for medical care, sometimes leading to bankruptcy" (p. 11). According to WHO (2023), "before the onset of the COVID-19 pandemic, advancements in achieving Universal Health Coverage (UHC) were already in decline. The UHC service coverage index only rose by 3 points to 68 by 2019 and remained stagnant at this level until 2021. This means that in 2021, approximately 4.5 billion individuals did not have complete access to necessary healthcare services" (para 11). However, the aforementioned became more serious when dealing with out-of- pocket (OOP) health expenses (indicator SDG 3.8.2). According to the United Nations Statistics, UNStats. (2023) [80], "Indicator 3.8.2 is defined as the "Proportion of the population with large household expenditure on health as a share of total household expenditure or income" (p. 1). The Organization for Economic Co-operation and Development [55] informs "Out-Of-Pocket (OOP) payments are categorized within the health care financing schemes (HF) section of the International Classification for Health Accounts (ICHA)." Moreover, [80] contends that "Health system funding is highly unfair because it depends only on how much households are willing and able to pay, granting access to health services and products based solely on individual financial resources, with no solidarity between healthy and sick people outside of the household" (p. 2). As for WHO (2023), "The percentage of the population facing significant OOP health expenses (SDG 3.8.2) rose steadily from 9.6% in 2000 to 13.5% in 2019, exceeding 1 billion people. Additionally, in the year 2019, 344 million individuals were pushed deeper into extreme poverty and 1.3 billion into relative poverty as a result of OOP healthcare expenses. Overall, during 2019, a total of 2 billion individuals experienced some type of financial difficulty (such as catastrophic, impoverishing, or a combination of both)" [83] (para 11).
Furthermore, a severe and substantial breach exists between the modern advances in medications and population affordability [1,3,64] Ongoing innovations in what relates to cell therapies, gene editing, stem cells, and biomechanical treatments are well beyond the reach of billions of our planet's populations. It is a fact that Gene therapy is one of the fastest-growing areas of healthcare, with over 2,000 therapies in development globally. These new techniques are being developed to conquer some of the world's most feared diseases such as HIV and cancer [60].
Gene therapies, also known as genetically modified cellular therapies, involve the direct modification of a patient's genes or genetic code to address or potentially cure their illness. Gene therapies are given in cases where conventional treatments are unable to address the root genetic issue [19]. According to Antrobus (2021) [4], gene therapies can treat diseases that were once untreatable like sickle cell disease, however, the treatment is extremely costly. Sickle cell disease changes the shape of red blood cells into a rigid sickle-like form, resulting in intense pain and weakness that can ultimately be fatal. Gene therapy appears to be the most effective remedy for sickle cell disease, but it comes with a high cost. Only those who are extremely rich can afford to be treated with a single dose for $2 million US dollars [4].
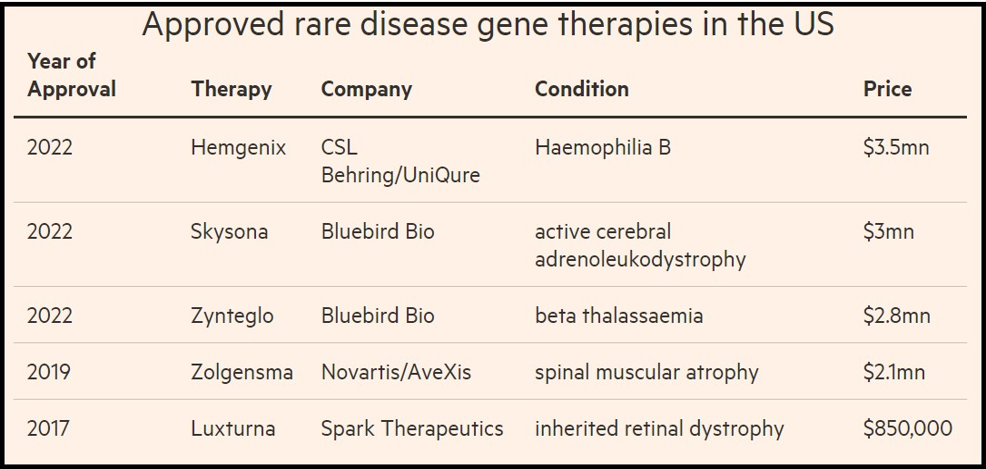
Cell and gene therapies are extremely expensive because producing, handling, and controlling the cells required to make them is far more complicated than working with the chemicals used to make traditional pharmaceuticals and even biopharmaceuticals [25]. For example, CART-cell therapy which is used predominantly in the treatment of hematological malignancies, including acute lymphoblastic leukemia, chronic lymphocytic leukemia, and lymphoma [87] has an estimated cost between $500,000 and $1000,000 [68]. Hemgenix priced at roughly $3.5 million is considered the world's most expensive medication used as a one-time gene therapy for hemophilia B bleed [26]. People with hemophilia B bleed longer than other people, and bleeds can occur internally, into joints and muscles, or externally, from minor cuts, dental procedures, or trauma [53]. Likewise, the cost of stem cell therapy can vary significantly depending on several factors. "Stem cell therapy, also known as regenerative medicine, promotes the repair response of diseased, dysfunctional, or injured tissue using stem cells or their derivatives" [17]. Stem cell therapy is the future practice in organ transplantation where cells are to be used instead of donor organs, which are limited in supply [49]. However, on average, stem cell therapy costs can range anywhere between $5,000 and $50,000 [17]. Table 1 presents a list of approved gene therapies in the United States of America including their companies, diseases, and prices.
Table 1: Approved rare disease gene therapies in the US.
Source: Smyth & Kuchler, 2022[74].
According to the World Health Organization (WHO), nearly 2 billion people have no access to basic medicines, causing a cascade of preventable misery and suffering [82] (May 11). This means essential medicines are unavailable and unaffordable for more than a quarter of the population worldwide [57]. The WHO has “hardly worked for more than 70 years to improve access to medicines and treatments because good health cannot be achieved without access to pharmaceutical products” [82] (May 11). The dilemma of affordability versus innovation in medicines has been seriously addressed since effective innovative medication continues to be available only to the rich and high-income sectors or is available to the poor when they are ready to give up their assets, belongings, and monetary savings, thus dragging them deeper into more devastating poverty [15,72]. Steinbrook (2007) [75] reported that many medications remain unaffordable in low- and middle-income countries. Moreover, as Riley reported (2012) [64], “Tell me something about your zip code (neighborhood) and I'll tell you something about your health…” (p. 173). Additionally, for middle- income patients, high medication costs beyond what insurance agencies or personal savings can handle will surely push them first into debt and later into poverty [76,83]. The poor patient’s real problem is a financial one – an inability to afford the pay or at least the co-pay for medication [51].
Penalva (2017) [58] says “The greatest of evils and the worst crime is poverty as declared by George Bernard Shaw in the introduction to his famous 1906 play Major Barbara” (para 1). “No other sin is punished as severely” [64]. Balasegaram (2014) [7] raises a big question “If a new drug is developed and nobody can afford it, where is the benefit from it?” Exhibit 1, herein, illustrates a controversial incident about the subject.
Exhibit 1: Bayer CEO Marijn Dekkers’ harsh remark
|
A story was published by Ketaki Gokhale of Bloomberg in Businessweek on January 21, 2014, discussing disagreements about drug patents. The narrative concluded with a foreboding statement by Bayer CEO Marijn Dekkers, "We didn't create this drug for the Indian market." We created it for Western patients who have the means to pay for it.” Dekkers made a remark during a December 3, 2013 gathering organized by the Financial Times, which was called "Buffering the Pharma Brand: Restoring Reputation, Rebuilding Trust." The health advocates were captivated by the article and Dekkers' quote, causing it to go viral in the health policy community. A week later, Ryan Chittum from the Columbia Journalism Review wrote an article, claiming that Gokhale had inaccurately quoted Dekker's statements. Bloomberg examined the paraphrased quote and revised the article accordingly. “So now, is this going to have a big effect on our business model? No, because we did not develop this product for the Indian market, let’s be honest. I mean, you know, we developed this product for Western patients who can afford this product, quite honestly.” Even though Dekkers' statement was slightly different from his initial quote in Businessweek, he is still more considerate in his rejection of cancer patients in India compared to the initial report. The slight variations in tone do not affect the overall message. |
Source: [10, 36]
One comment in Forbes magazine about the above matter was from LaMattina (2013) [46] who asserts "That is a rather controversial remark. During a period when the pharmaceutical industry's image is being tarnished, Dekkers' statement only adds to the problem. Instead, it confirms the idea that Big Pharma's main focus is on making money and individuals who require life-saving medications are left to fend for themselves" (para 1).
Xu K (2007) [86] contends that "Worldwide, it is estimated that around 150 million households devote more than 40 percent of their nonfood spending to health care." Similarly, "Research shows significant levels of borrowing and asset selling to deal with financial shocks from medical expenses in the developing world, with one in four families across forty developing nations turning to borrowing or selling assets, or both, to cover health care costs" [24]. The aforementioned figure was reported by Kruk and her collaborators (2009) [45] where in forty low- and middle-income countries (a combined population of 3.66 billion), on average, 25.9 percent of households borrowed money or sold items to pay for health care. Conversely, "the biopharma sector argues that elevated prices are essential to offset the development expenses of gene therapies, which at $5 billion is about five times higher than those of conventional medications" [74]. Moreover, "the markets for these medications tend to be limited, and intricate manufacturing and regulatory procedures often result in extended lead times before therapies are accessible" (ibid).
As for Lebanon where the present study is conducted, Amnesty International (2023) [2] issued a public statement that due to the prevailing economic crisis, millions of people are unable to access their rights to health in general and in particular to the availability and affordability of medicines. Worth mentioning that Lebanon is undergoing one of the worst economic, financial, and political dilemmas leading to unrest and the population is under tremendous socioeconomic conditions, not even allowed to freely access their bank saving [38,43,65,66]. In fact, according to the European Commission report (2023) [23], the current economic crisis has caused 80% of the Lebanese to live in poverty and 36% below the extreme poverty line. Another report issued by the Human Rights Watch NGO (2022) [39] stated that the median household monthly income is around USD 122, and inflation is dramatically rising. Moreover, the same report indicated that based on a survey conducted on 1209 households between November 2021 and January 2022, 43.1% were unable to pay for medicine, medical care, or health services. In addition, ESCWA (2021) [22] issued an alarming report stating that the percentage of households deprived of health care has increased from 9% in 2019 to 33% in 2021 and this percentage is on the rise since 55% of the Lebanese population is not covered by any form of health insurance. Consequently, according to the [69,77], Lebanon ranks 110 out of 166 countries with 63.9% SDG index score (worsening conditions towards poverty alleviation and other areas). Based on the previously reported facts, it can be declared that poverty leads to deteriorated health and deteriorated health will surely sustain poverty. Consequently, the poorer a population is, the less access to health services will prevail and the larger the amount of total health spending is out of pocket (OOP) [59]. It can be easily deduced that among the middle class (people with jobs that pay significantly more than the poverty line), paying for health services means spending high proportions of their income or selling their assets which will surely drag them to poverty. Here one cannot but recall Julian Tudor Hart's (1971) [28] "Inverse Care Law" which proposed that social care tends to vary inversely with the needs of the population served. Additionally, it is worth mentioning that the protected patent system with its market-driven research and development incentives has failed to provide the poor populations with necessary modern medications since the common practice to recoup the high costs of research and development is through sky-high prices [82]. Thus, the affordability of modern state-of-the-art medications that can cure many serious fatal diseases is well beyond the budgets of much of the population, motivating this paper's title "He who has the cash gets the cure."
It is undeniable that the cutting-edge medications of today are right at our doorstep. It is our duty as a nation to strategize and decide on funding for these cutting-edge treatments to reap their potential rewards while also making sure our society can afford them. It would be a great tragedy if society couldn't enjoy the benefits of modern innovations due to the inability to pay for them. That's the problem seen from one side! On the other side, another major problem presents itself. DeLuca & Cossu (2023) [18] assert that "To recoup the costs of research, development, and production of modern state-of-the-art medication, companies demand a very high price for these therapies, ranging from several hundred thousand to a few million dollars per patient."
This paper aims to assess the extent of awareness and reactions of a selected Lebanese population concerning medications, in general, and high-cost medicines, in particular. It will also investigate possible decision-making stances toward the affordability of medications if facing a serious medical condition that requires expensive medication.
The merit of this paper is manifolds. It enriches the theoretical foundations by adding to the body of knowledge new facts from Lebanon, to the best of our knowledge no research is conducted in Lebanon about the subject, therefore making it innovative, in addition that it involves a cross-country sample size covering a broad age span.
Research Methodology
This research utilized positivism. Hejase and Hejase (2013) defined it as “researchers remaining impartial and not interfering with the research subject” (p. 77). Positivists develop research questions that can be tested. This study's method is logical, deductive, and based on scientific concepts concurrently. Employing controls confirms data authenticity by clarifying the connections among variables. Using primary data to clarify concepts aids in reaching the clearness of definitions. Concepts are assessed, clarified, and subjected to quantitative analysis. Furthermore, the study utilize a survey method. This leads to a standard survey given to a selected group of people.
The objective is to collect unprocessed data for statistical evaluation. As the study takes place in a designated time during the spring of 2024, the temporal horizon aligns with a cross-sectional timeframe.
Sampling and Sample Size
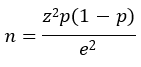
This will be achieved by considering a random sample selected from different Lebanese regions where the sample size “n” is determined by Cochran’s formula as presented in Hejase & Hejase (2013, p. 231): [30]
Where
z = The degree of confidence, for the present study, is 92% gives z = ±1.75
p =The proportion of the population facing pharmaceutical poverty, i.e., when a patient cannot afford the cost of a prescribed medication. In our case, we ignore this proportion, so we consider the case of maximum variability with p = 0.5
e = The desired level of precision (accuracy), we considered 5%. Using these values in Cochran’s formula, a sample size of 307 individuals is obtained. Out of 350 questionnaires distributed, 307 valid ones were gathered, with 43 either partially completed (31) or returned with only demographic information (12) being excluded. The response rate received was 87.71%. To increase the credibility of this sample size, another approach is employed with a sample size of 307 and a population size exceeding one million. This work adopted the approaches of [12,21,34,35,61,67] to calculate approximation reliability error values based on Hardwick's (2022) [27] findings. Table 2 shows that with a population greater than one million, a standard error of 5%, and a reliability of 6% ± 0.2%, the sample size needed is approximately 307. Therefore, at a confidence level of 95%, the sample size of 307 participants in the study yields a margin of error of ± 5.8%. This suggests that in 94.2 out of every 100 times the survey is conducted, the outcomes will differ by no more than 5.8%. Such a degree of reliability would be appropriate for this kind of initial inquiry.
Table 2: Statistical reliability versus sample size
|
[50/50% proportion characteristics] |
||||||
|
Population |
||||||
|
Sample Size |
500 |
1000 |
5000 |
10000 |
100,000 |
1 Million+ |
|
75 |
±10.4% |
±10.9% |
±11.3% |
±11.4% |
±11.5% |
±11.6% |
|
100 |
±8.8% |
±9.3% |
±9.7% |
±9.8% |
±9.9% |
±10.0% |
|
200 |
±5.4% |
±6.2% |
±6.8% |
±6.9% |
±7.0% |
±7.1% |
|
300 |
±3.6% |
±4.7% |
±5.5% |
±5.6% |
±5.7% |
±5.8% |
Note: At a 95% confidence level (standard error is 5%).
Source: Modified from Hardwick Research, 2022.
Survey Design
The survey consists of three sections. Section one covers fourteen demographic questions using dyadic and multiple-choice styles. Section two consists of thirty-eight questions related to wellness, health conditions, and preventive medical checkups. The third section has seventeen questions to assess awareness about medication affordability and possible decision-making situations to explore actions to take in case there is a need for expensive medications. Sections two and three comprise multiple-choice queries and an evaluation of statements using a 5-level Likert scale. These inquiries were created to assess participants' perspectives, understanding, and consciousness regarding health, medications, and cost. The participants were instructed to select the most suitable subjective responses from the provided list of closed-ended questions.
Validity
The paper's design was executed without sacrificing its validity. This design enhances external validity, enables more genuine participant reactions, and ensures the data align with the findings. Three specialists confirmed the accuracy of the evaluation's content. The main assertions are articulated, leaving no room for debate, and in line with research protocols. Because the questionnaire was constructed using information from the literature review, its validity is ensured. Nevertheless, experts recommended specific changes and after testing the survey on twenty individuals not included in the sample, the final version of the survey was determined.
Ethical Considerations
Participants received sufficient information on the topic of the study. The researchers told them that taking part in the study is voluntary, their names will remain confidential, and they can choose to stop anytime without being questioned. Additionally, the participants were guaranteed that their information and identities would be kept confidential and anonymous and that the findings would solely be utilized for academic purposes. To prevent any ethical violations, participants were informed of these guidelines in the initial survey instructions.
Data Analysis
Hejase et al. (2012) [33] argue that "making informed and unbiased decisions is crucial, are grounded in factual data and figures, genuine, pragmatically accurate, and timely data." Moreover, "descriptive statistics utilize straightforward numbers or visuals to understand a dataset" [30]. Tables display means, standard deviations, frequencies, and percentages for clarification. The analysis of data was conducted using the Statistical Product and Service Solutions, IBM's SPSS version 26.0 software package. Additional inferential statistical techniques include a one-sample T-test, Cross-tabulation, and Regression modeling analysis.
Results and Findings
Demographics
Adults above 18 years selected from seven regions in Lebanon completed a questionnaire regarding their health status and awareness of modern high-cost medications.
Among other age statistics presented in Table 3, the average age of the 283 respondents who accepted to declare their ages is 38.25 years (std. dev. of 16.01 years and a median of 33 years). Moreover, 46.9% (144 respondents) were females, and 53.1% (163 respondents) were males.
Table 3: Statistics for the ages of the respondents (years)
|
Mean |
38.25 |
Std. Deviation |
16.061 |
|
Median |
33.00 |
Minimum |
18 |
|
Mode |
23 |
Maximum |
96 |
|
|
|
|
|
|
Percentiles |
25 |
25.00 |
|
|
50 |
33.00 |
|
|
|
75 |
50.00 |
|
Note: Valid entries 283 and missing 24.
Table 4: Distribution of respondents per geographical area
|
Region |
Frequency |
Respondents, % |
|
Beirut |
127 |
41.37 |
|
Dhahieh |
53 |
17.26 |
|
Mt. Lebanon |
50 |
16.3 |
|
South Lebanon |
33 |
10.75 |
|
Shouf |
20 |
6.51 |
|
North Lebanon |
15 |
4.88 |
|
East Lebanon (Bekaa) |
9 |
2.93 |
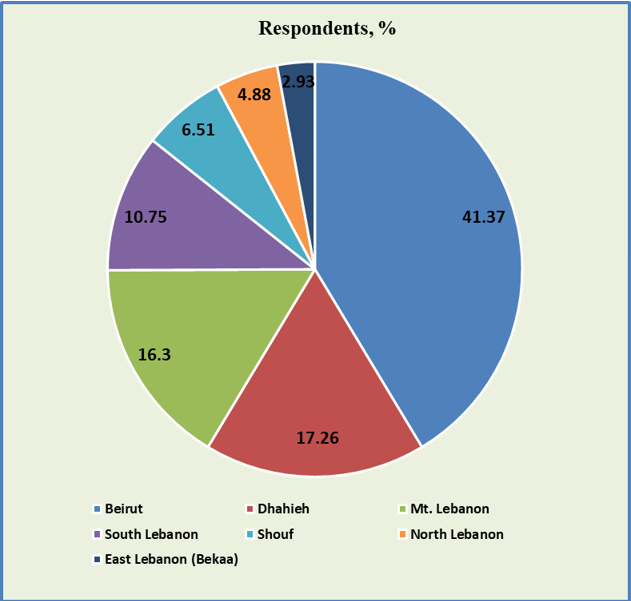
Figure 1: Distribution of respondents per geographical area
Table 4 and Figure 1 show the distribution of respondents within the seven selected regions in Lebanon. Notice that Beirut had about 41.4% of the respondents and its southern suburbs (Dhahieh) had 17.3% of the respondents (180 respondents in total). The rest of the Lebanese regions accounted for 41.3% of the respondents (127 respondents). This agrees with the figures issued by the United Nations Agency for Human Settlements [79], mainly, that the Lebanese population lives in large agglomerations mostly in the city of Beirut and its southern suburbs (Dhahieh).
Likewise, the distribution of marital status includes 48.2% being married (147 out of 305) and 45.2% being single (138 out of 305). The remaining 6.5% (20 respondents) were divorced, widowed, separated, or cohabited.
As for the educational background of the respondents (306 answered the question), 40.5% (124 respondents) had a university education, 37.9% (116 respondents) had graduate studies, 11.8% (36 respondents) high school, 6.5% (20 respondents) middle high school, 2.9% (9 respondents) primary education, and 0.3% (1 respondent) had no school education at all. These figures indicate that the selected sample is highly prepared and educated. As for answering “Where do they live?” Of the 304 who answered the corresponding question, 202 own their houses (66.4%), 66 rented houses (21.7%), and the remaining 36 respondents (11.8%) indicated that they neither own nor rent houses but live in other places.
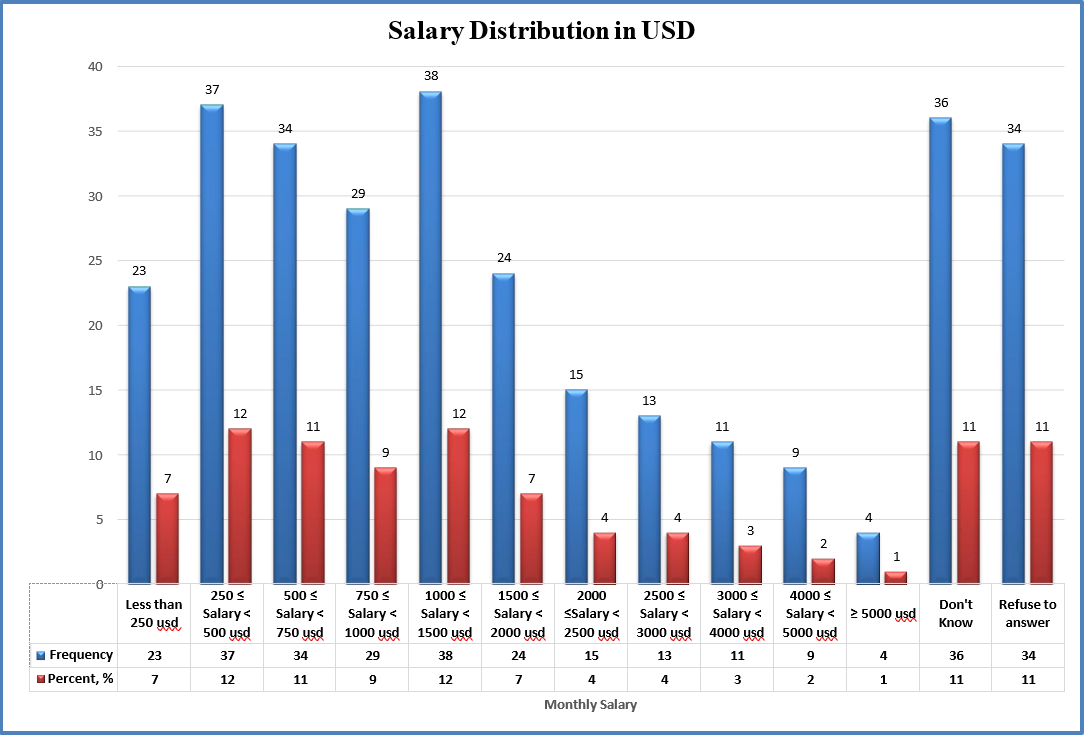
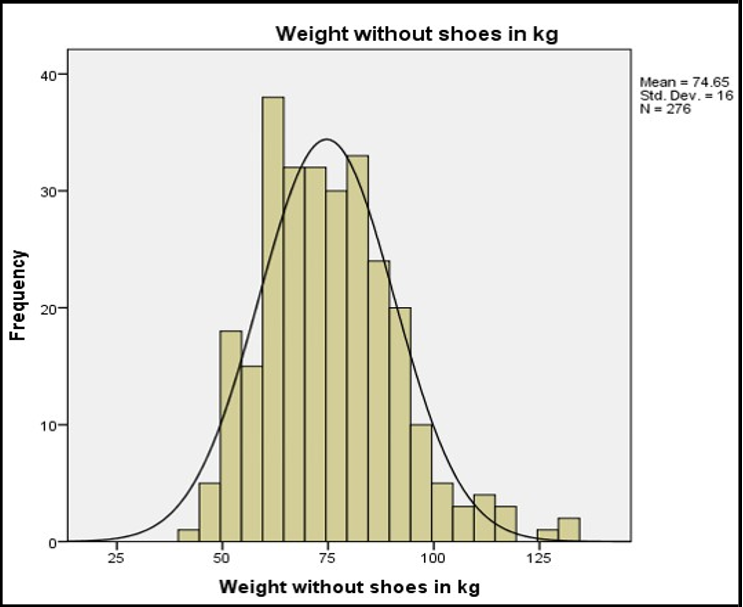
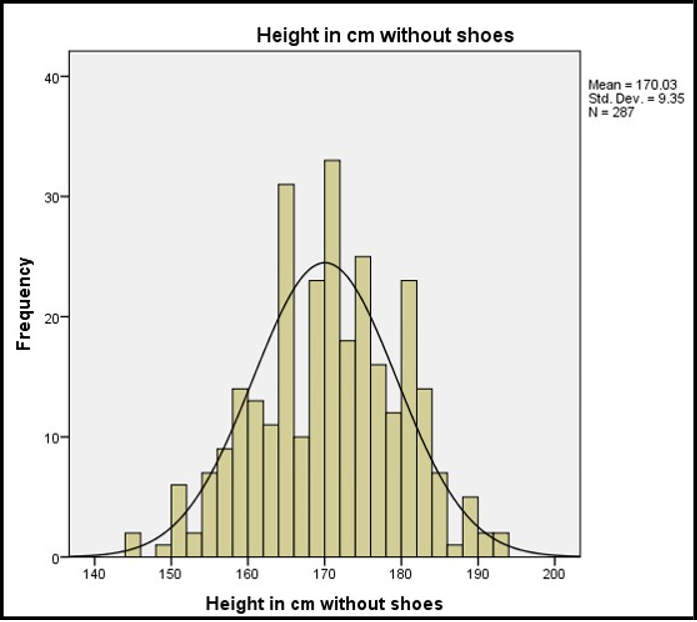
As for the working status of the respondents, 61.9% (190 respondents) work for others, 8.1% (25 respondents) had their own business, 6.5% (20 respondents) were housewives, 14.3% (44 respondents) were students, 4.2% (13 respondents) retired, 4.6% (14 respondents) were jobless, and 0.3% (1 respondent) unable to work. Figure 2 shows the distribution of the total family monthly incomes of the respondents. Likewise, Figures 3 and 4 show the weight (mean=74.65 kg with a std. dev. of 16 kg) and height (mean=170.03 cm with a std dev. of 9.35 cm) distributions of the respondents.
Figure 2: Respondents' monthly income distribution
Figure 3: Distribution of Respondents' Body weights.
Figure 4: Distribution of Respondents' heights.
Finally, when respondents were asked what plan of health insurance they owned? It is noticed that 77.3% (235 out of 304) of the respondents got some plan of insurance (business, governmental/ social security, armed forces) with 13.7% (42 out of 304) buying their insurance plan. Of those that got no insurance at all 54 respondents (17.6%) and 5.1% did not answer. Worth mentioning that Berchick, Hood, & Barnett (2018) posit “In 2017, 8.8 percent of people in the USA, or 28.5 million, did not have health insurance at any point during the year” (p. 1).
Health Status
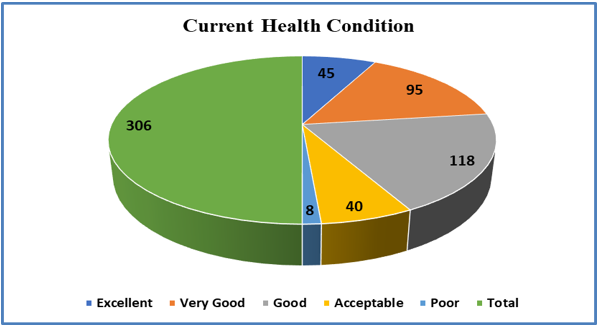
According to the National Center for Health Statistics (2024)[54], “Health status is a measure of how people perceive their health. Reported health status is a predictor of important health outcomes including mortality, morbidity, and functional status.” As depicted in Table 5 and Figure 5, among our respondents where the average and median ages are 38.25 and 33 years, respectively, the percentage of people reporting poor health status is 2.61% which is a relatively low percentage due to the relatively low age central tendency statistics.
Table 5: Respondents’ current health conditions
|
Current Health Conditions |
Frequency |
Percent, % |
|
Excellent |
45 |
14.71 |
|
Very Good |
95 |
31.05 |
|
Good |
118 |
38.56 |
|
Acceptable |
40 |
13.07 |
|
Poor |
8 |
2.61 |
|
Total |
306 |
100.00 |
Figure 5: Respondents’ current health status.
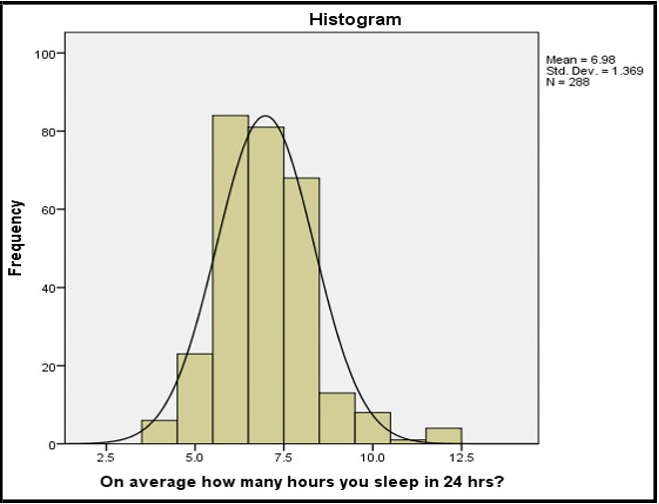
Another indicator that supports the low percentage of individuals with poor health status is the night hours of sleep. It has been reported that for adults, getting less than seven hours of sleep a night regularly is linked with poor health [56]. Figure 6 presents the nearly normal distribution of respondents’ sleeping time where the median and average times are 7 and 6.98 hours, respectively; thus, these figures support the positive health status (well-being) of the respondents.
Figure 6: The amount of sleep reported by the respondents.
Health Care Affordability
Axene (2003) [5] posits that “Healthcare affordability describes whether a person or organization has sufficient income to pay for or provide for healthcare costs.” In this study, participants were asked if during the past twelve months they were unable to see a physician due to lack of money. Fortunately, 81% (247 out of 305) of the respondents indicated a negative answer while only 18.4% (56 out of 305) affirmed that they could not see a doctor because of monetary issues.
Table 6: Health Care Habits
|
Subject |
|
Frequency |
Percent, % |
|
Last time they visited a physician for a routine checkup |
|
|
|
|
The last time visited a Dentist |
|
|
|
|
Females |
|
|
|
|
When was the last time you had a mammogram? |
|
|
|
|
When was the last time you did a cervical |
|
|
|
Table 6 shows that only 58.6% of the respondents indicated that they had visited a physician for a routine checkup during the past 12 months. According to Scripps (2023) [71], “Annual physical exams are the foundation of preventive care and doctors strongly recommend them to help manage health issues; moreover, routine checkups aim to ensure good health and prevent any serious conditions.”
Going further into dental issues, only 52.9% (162 out of 306) of the respondents indicated that they had visited a dentist within the past twelve months. The figures in Table 6 imply that financial limitations often prevent people from getting timely dental care. The College of Dentistry-UIC (2022) [16] confirms the above observation.
It was surprising that only 14.7% (21 out of 143 females) reported that they had had a mammogram during the past 12 months (see Table 6). The results above show that the sample females do not practice the recommendation by [81] who asserted that “Adult females should have a mammogram every year starting at the age of 30.” In our case, it looks like cost has acted as a barrier to screening mammography for the majority of the respondents. The literature on screening mammography is rich with studies indicating that the most tangible barrier is cost [50]. Moreover, 77.8% of the female respondents never did a cervical cancer screening and that is also attributed to financial barriers and poor healthcare affordability. This percentage coincides with a study done in the USA in 2021 where it was concluded that “72% of participants perceived financial barriers to screening” [9]. Likewise, our results are supported by the work of [41] which demonstrated the effect of cost on cervical cancer screening.
Colorectal cancer (CRC) Testing
Participants were asked if they had done Colorectal cancer (CRC) related examinations. Hejase, A., Hejase, Nemer, et al. (2020) [31] assert that “CRC continues to be one of the principal global healthcare issues where it ranks second to breast cancer among females and third after lung and prostate cancers among males.” In the current study, 296 participants answered the related question where 78.7% of the respondents indicated that they never had a colonoscopy and/or sigmoidoscopy; those who had had a colonoscopy were 10.4% (only 32 respondents) and those who had had sigmoidoscopy were 2.4% (only 7 respondents). “Medical research indicates that CRC screening reduces morbidity and mortality due to an early detection of the malignancy” [32]. Likewise, participants were asked if they had done screening for CRC with a stool test. The most common stool test is the Fecal Immunochemical Test (FIT) where a small sample of poo is sent to a lab to be checked for tiny amounts of blood which can be a sign of polyps or bowel cancer. Unfortunately, only 22.3% of the participants declared that they had done the test (67 out of 301), and 72.4% indicated that they had not done such a test. In 2018, “CRCs are the third most commonly diagnosed form of cancer globally, comprising 11% of all cancer diagnoses” [62]. As for Lebanon, [42] reported that “1463 (8.5%) CRC cases out of 17,298 new cancer cases were reported for both sexes thus ranking in fifth place after breast, bladder, lung and prostate cancers” (p. 17). Our results align with what has been reported in the literature. Lee et al. (2022) [47] reported that “OOP costs have been identified as a major barrier to screening.”
Eye Care Examination
The resulting answers were that 41.37% (127 out of 307) of respondents had never done an eye examination, and 13.36% (41 out of 307) had received an eye examination within the past 2 years. Only 10.42% (32 out of 307) of the participants reported having a vision examination during the past month. The literature indicates that affordability is a core factor significantly associated with receiving vision care [6, 40].
Diabetes Testing
Upon asking respondents, ‘When was the last time you did a diabetes test?’ The responses indicated that 40.7% of the participants (126 out of 307) have never done such a test, and 38.1% (117 out of 307) did the test sometime during the past 12 months. Researchers posit that diabetes is more prevalent in low-income populations [13]. Moreover, it has been reported that poverty is not only associated with higher diabetes incidence but also with poor diabetes testing and care [37]. Based on the aforementioned information, the 40.7% figure that participants have never done any diabetes tests supports the finding herein that the population, in question, has low healthcare affordability.
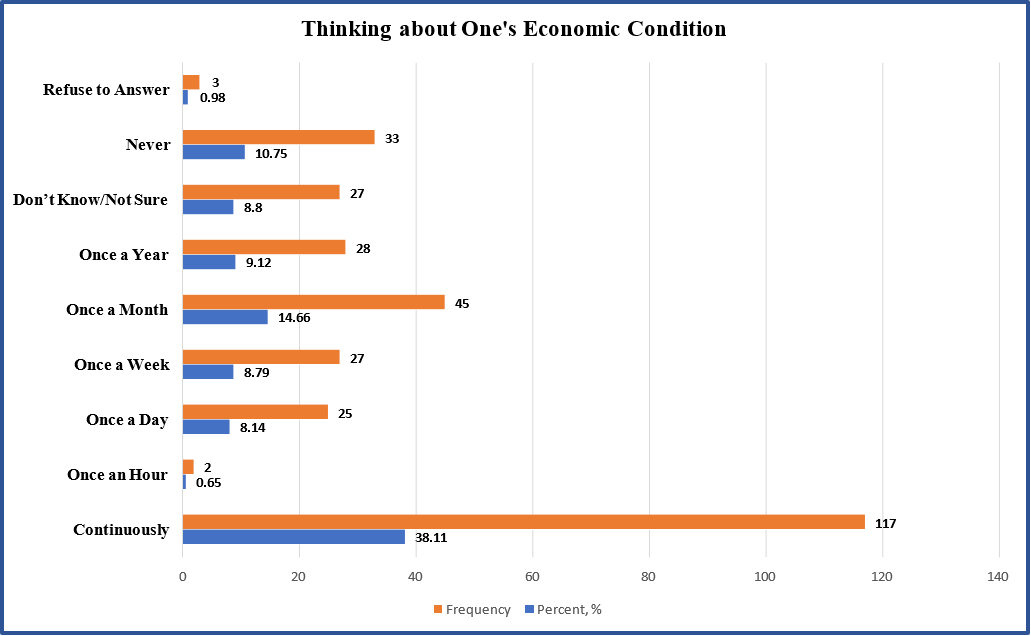
Affordability
To clarify further the issue of economic status in general and affordability in particular, participants were asked about how many times they think of their economic condition. Figure 7 depicts that 38.11% (117 out of 307) continuously around the clock think about their economic conditions while only 10.75% (33 participants) never think about that. Also, we can interpret the other readings as incidental occasions where the economic conditions governed a cost that is relatively high to pay. These figures are an unmistakable indication of the poor economic status of the population this study is dealing with. Moreover, the continuing socioeconomic crisis has significantly affected access to vital medications, which adds to the Lebanese participants’ concerns. According to El-Jardali, Masri, & Sleem (2023) [20], “Even with significant investment in pharmaceuticals (which makes up over 25% of healthcare costs), drug supplies have fallen by 50% since the crisis began, leaving over 70% of the Lebanese people unable to obtain essential medications” (para 4).
Figure 7: Participants' answers for when they think of their economic conditions.
Adherence to Medications
Researchers [8,14,73] (Tsou, Graf, Russell, & Epstein, 2021) confirm that “The cost of medicines has been thoroughly recognized as a factor that limits adherence to medications, mainly for poor populations.” Moreover, it has been reported that “nonadherence degrades health and escalates the risk of hospitalization and death” [44]. In this study, we did conclude in the previous sections that our population can be classified as poor. Therefore, in what follows, we shall investigate nonadherence to medications where the results are presented in Table 7.
Table 7: Respondents' answers related to nonadherence to medications.
|
Statement |
SA |
A |
N |
D |
SD |
Mean |
Std Dev (SD) |
|
|
Percent, % |
* Based on Codes |
|||||
|
Not using the prescribed medicines will lead to health deterioration and higher health costs. |
19.0 |
57.8 |
14.1 |
6.9 |
2.3 |
3.84 |
0.888 |
|
Not using the prescribed medicines will lead to worse health condition and higher death risk |
19.0 |
62.7 |
9.5 |
6.2 |
2.6 |
3.89 |
0.871 |
|
I agree that when medicine costs are high one may abandon the treatment |
20.6 |
50.0 |
11.8 |
13.7 |
3.9 |
3.70 |
1.066 |
|
I am aware that when medicine costs are high one takes the treatment even though one has to get loans |
11.8 |
55.6 |
19.3 |
10.5 |
2.9 |
3.63 |
0.926 |
|
I agree that the poor suffer due to the high cost of medicines |
52.0 |
40.8 |
5.2 |
0.3 |
1.6 |
4.41 |
0.751 |
Note: A 5-level Likert scale is used with SA: Strongly Agree (5), A: Agree (4), N: Neutral (3), D: Disagree (2), and SD: Strongly Disagree (1). * Codes: 1 to 5. The same notation is used in Tables 9 and 10.
The data shown in Table 7 illustrate that 81.7% of the respondents agree and strongly agree that nonadherence to prescribed medications worsens health and increases the risk of death (mean=3.89, SD=0.871) this coincides with the conclusions of Kim et al. (2018) [44]. Additionally, 70.6% of the respondents approve (mean=3.70, SD=1.066) that when medicine costs are high, they may abandon the medical treatment as concluded in diverse studies [8,14,73,84] (Tsou, Graf, Russell, & Epstein, 2021).
Table 8: Respondents’ awareness about their inability to buy high-cost medicines
|
Statement |
SA |
A |
N |
D |
SD |
Mean |
Std Dev (SD) |
|
|
Percent, % |
*Based on Codes |
|||||
|
I agree that the high costs of medicines lead to poverty |
13.4 |
49.3 |
25.5 |
9.8 |
2.0 |
3.62 |
0.905 |
|
I agree that high-cost medicines can cure dangerous diseases |
12.7 |
57.2 |
18.6 |
10.1 |
1.3 |
3.70 |
0.865 |
|
I agree that many suffer or die because of their inability to get medicines whose production costs are a few dollars |
37.3 |
51.6 |
7.5 |
2.6 |
1.0 |
4.22 |
0.772 |
|
I agree that many suffer or die because of their inability to buy high-cost medicines |
36.3 |
54.9 |
6.9 |
1.3 |
0.7 |
4.25 |
0.695 |
|
Pharmaceutical companies don't help the poor. They steal the poor to pay the rich. |
32.0 |
39.9 |
21.2 |
4.9 |
2.0 |
3.95 |
0.952 |
Note: For abbreviations, see note in Table 7.
Table 8 demonstrates that 62.7% of the respondents (mean=3.62, SD=0.905) approve (adding strongly agree and agree) that high-cost medicines lead to poverty; additionally, 69.9% of the respondents accept that high-cost medicines can cure dangerous diseases. The most notable result in Table 8 is that 88.9% of the respondents (mean=4.22, SD=0.772), support that many suffer or die because of their inability to get medicines whose production costs are a few dollars. This result goes in parallel with what Bernie Sanders; the US Senator for Vermont wrote: "No one in America, or anywhere in the world, should die or suffer unnecessarily because they cannot afford a prescription drug which, in many cases, costs a few cents or a few dollars to manufacture" [70]. In addition, Table 8 shows that 91.2% of the respondents are aware that many suffer or die because of their inability to buy high-cost medicines. The World Bank and WHO (2017b) [85] and Taylor (2023) reported that "Half the world lacks access to essential health services, and 100 million are still pushed into extreme poverty because of health expenses." As for the pharmaceutical companies, 71.9% of the respondents believe that pharmaceutical companies don't help the poor; they steal from the poor to pay the rich. This once again agrees with what Bernie Sanders wrote: "The business model of the pharmaceutical industry values dollars gained over lives saved." [70]. "Now we must have the courage to stand up to the pharmaceutical industry. Let's do it." [70].
Finally, Table 9 provides the respondents' answers related to healthcare expenses and the assets they own. This table is aligned to the title of this paper "He who has the cash gets the cure." A strong validation is scored as our paper's title is congruent with a statement made by the Director of the WHO, General Gro Harlem Brundtland, who posited that "For many, the reality is stark: No cash, no cure" [63]. Results depicted in Table 9 indicate that 86.2% of the respondents approve (adding agree and strongly agree) that poor people become poorer due to paying health expenses with their own money. Additionally, 88.9% of the respondents accept that family savings will drain due to high healthcare expenses. Likewise, 78.1% of the respondents support that high medicine costs should motivate individuals to sell their properties to save the lives of family members. Finally, the great spirit of sacrifice or giving up what a person considers essential to their well-being is presented in the answers to the question: "I am ready to sell all my properties to get a high-cost medicine that can save one of my family members". Astonishingly, 80.7% of the respondents (246 out of 305) declared that they were ready to sell their properties to save the life of a family member. Those who disagreed (adding disagree and strongly disagree) with the statement were only 20 respondents (6.6%).
Table 9: Respondents' answers related to their assets and medication expenses.
|
Statement |
SA |
A |
N |
D |
SD |
Mean |
Std Dev |
|
|
Percent, % |
*Based on Codes |
|||||
|
Poor people become poorer due to paying health expenses out of pocket |
29.7 |
56.5 |
9.8 |
3.3 |
0.70 |
4.11 |
0.757 |
|
Family savings will drain due to high healthcare expenses |
27.1 |
61.8 |
9.2 |
1.3 |
0.70 |
4.13 |
0.676 |
|
High medicine costs should motivate individuals to sell their properties to save the lives of family members |
27.8 |
50.3 |
13.7 |
5.9 |
2.3 |
3.95 |
0.926 |
|
I am ready to sell all my properties to get a high-cost medicine that can save one of my family members. |
39.9 |
40.8 |
12.7 |
3.3 |
3.3 |
4.11 |
0.971 |
Note: For abbreviations, see note in Table 7.
To check if gender is an influential factor in health treatments, the relationship between gender and the question, "Are you aware that when medicine costs are high you may abandon the treatment?" was investigated using a chi-square test of independence. With χ2 (4, N = 303) = 4.276, p < 0.37, the correlation between these variables was not statistically significant. Thus, there is no relationship between gender and being aware that when medicine costs are high one may abandon the treatment.
Conclusion and Recommendations
This research aimed to investigate the attitude and stance of a sample of Lebanese citizens, aged 18 to 96 years, towards the dilemma of affordability of new medication versus individuals' economic status. In addition, it explores these individuals' actions when faced with chronic conditions and how to acquire the corresponding unaffordable new medications.
The high cost of medicines compared to health concerns, awareness, and activities is the subject of the first cross-sectional study of its kind conducted in Lebanon. The ongoing stream of studies and reports addressing the affordability of expensive medicines and the significance of maintaining a healthy community served as a rationale for this kind of investigation. Motivating, creating, increasing, and maintaining the Lebanese population's understanding of the significant advantages of preventive healthcare testing to avoid chronic illnesses when affordability becomes either a killer or extreme poverty was the foundation for the current study.
The outcomes of this study support the research objectives. A gamut of previous works reported, monitored, investigated, and measured the issue of affordability of medications and the catastrophic consequences that may lead to extreme poverty undermining the global efforts in achieving Universal Health Coverage (UHC) [1,3,64,80,83,85]. The situation is so critical that WHO (2023) reported that "the proportion of individuals encountering substantial out-of-pocket (OOP) health costs (SDG 3.8.2) increased consistently from 9.6% in 2000 to 13.5% in 2019, surpassing 1 billion people. Furthermore, in 2019, 344 million people were driven further into extreme poverty and 1.3 billion into relative poverty due to OOP healthcare costs. In total, throughout 2019, approximately 2 billion people faced various forms of financial hardship (including catastrophic, impoverishing, or a mix of both)" [83] (para 11). This research capitalizes on the current findings, first in the context of Lebanon, in addition to adding new facts toward the global attitude concerning the reduction of poverty. Recalling SDG 1, the Sustainable Development Goal 1, which calls for the global efforts to end poverty in all its forms everywhere [48]. Therefore, the results of this article contribute to reducing the lack of information about Lebanon and the region, particularly given that the recent crisis in Lebanon is unique in comparison to those in other countries. Such findings may be useful to researchers and interested specialists in poverty and healthcare, who can then build on them to conduct additional studies on at least two dimensions: Examining the views of healthcare policymakers during emergencies and analyzing a representative sample of the Lebanese populace on costly drugs. Last but not least, more scholars are encouraging government action by putting out creative solutions to the affordability problem, backed by international expert organizations such as the UN, WHO, and World Bank.
Limitations
The study's sample size, respondent demographics (excluding middle and upper management from government agencies and healthcare specialists and experts for comparative purposes), and the challenge of recruiting a larger sample size due to the research's subject matter are some of its limitations. As a result, while the findings might not be broadly applicable, they are enlightening and offer valuable perspectives on the circumstances in Lebanon or a comparable nation during the severe economic and financial crises.
Future Research
There exists an ongoing and pressing requirement to initiate nationwide campaigns that help educate Lebanese citizens about chronic illnesses, the risk factors involved, and the effective treatments, as well as the potential options to support or fund the expenses of expensive medications. Therefore, a well-informed background must be present. Such need necessitates that researchers, professionals, NGOs, higher education institutions, and government agencies collaborate on a national level to profile the extreme citizen cases throughout Lebanon necessitating financial support. Consequently, create a funding body that alleviates the citizens' harsh conditions besides the typical governmental subsidies of chronic disease medications.
There is a need for further research to collect a much broader database to monitor the healthcare needs of citizens. This study offers a starting point and provides a clear view of the current Lebanese citizens' views and attitudes towards the highly priced medications. Hence, enriching the ongoing health education of various community groups (e.g., NGOs and family associations) that may assist in developing local preventive screening protocols, as well as incorporating them into health provider training programs. The Ministry of Health must establish a community consortium to respond proactively to the emerging trends in innovative drugs and their pricing strategies.
References
- Experts in Chronic Myeloid Leukemia (2013) The price of drugs for chronic myeloid leukemia (CML) is a reflection of the unsustainable prices of cancer drugs: from the perspective of a large group of CML experts. Blood. 121(22): 4439–4442.
- Amnesty International. (2023) Lebanon: Government Must Ensure medication is available and affordable.
- Antonanzas F, Terkola R, Overton P.M, Shalet N, Postma M (2017) Defining and Measuring the Affordability of New Medicines: A Systematic Review. Pharmacoeconomics. 35(8): 777-791.
- Antrobus K (2021) How we can make gene therapies available to all. Global Health.
- Axene D.V (2003) Health Care Affordability: A Valuable Concept in Understanding Our Health Care System Challenges. Health Section News. (45): 20-22.
- Bake R.S, Bazargan M, Bazar-Hejazi S, Calderón J.L (2005) Access to vision care in an urban low-income multiethnic population. Ophthalmic Epidemiol. 12(1): 1-12.
- Balasegaram M (2014) Medicine is just for those who can afford it. Al-Jazeera.
- Banerjee A, Khandelwal S, Nambiar L, Saxena M, Peck V, et al. (2016) Health system barriers and facilitators to medication adherence for the secondary prevention of cardiovascular disease: a systematic review. Open Heart. 3(2): e000438.
- Biddell C.B, Spees L.P, Smith J.S, Brewer N.T, Des Marais A.C, et al. (2021) Perceived Financial Barriers to Cervical Cancer Screening and Associated Cost Burden Among Low-Income, Under-Screened Women. J Womens Health (Larchmt). 30(9): 1243-1252.
- Cassedy C (2014) Transcript of Bayer CEO Marjin Dekkers quote at the December 3, 2013 FT Event, regarding India compulsory license of Nexavar. [Blog] Knowledge Ecology International.
- Centers for Disease Control and Prevention (CDC). (2023) Behavioral Risk Factor Surveillance System.
- Chehimi G.M, Hejase H.J (2024) Exploring the Impact of Bilingualism in Early Life on Foreign Language Learning for University Students in Lebanon Theoretical Foundations: Part I. Journal for the Study of English Linguistics. 12(1): 1-31.
- Chen Y, Zhou X, Bullard K.M, Zhang P, Imperatore G, et al. (2023) Income-related inequalities in diagnosed diabetes prevalence among US adults, 2001−2018. PLoS ONE 18(4): e0283450.
- Choudhry NK, Bykov K, Shrank WH, Toscano M, Rawlins WS, et al. (2014) Eliminating medication copayments reduces disparities in cardiovascular care. Health Aff. (Millwood). 33(5): 863-870.
- Colbert A, Andrew R, Simão M, Hill S, Swaminathan S (2020) Can affordability and innovation coexist for medicines? BMJ. 115: 17058.
- College of Dentistry-UIC. (2022) The Many Costs (Financial and Well-Being) of Poor Oral Health.
- Cona L.A (2004) DVC Stem (Da Vinci Centre). Stem Cell Therapy Cost (2024 Update).
- De Luca M, Cossu G (2023) Cost and availability of novel cell and gene therapies: Can we avoid a catastrophic second valley of death? Science & Society. 24(2): e56661.
- Draeger S (2023) Gene therapies: Can we afford the future of medicine?. OPTUM.
- El-Jardali F, Masri R, Sleem Z (2023) Rethinking Lebanon’s Healthcare System Amid the Economic Crisis. The Lebanese Center for Policy Studies (LCPS).
- El Takach A, Nassour F, Hejase H.J (2022) Digital Transformation of Media Companies in Lebanon from Traditional to Multiplatform Production: An Assessment of Lebanese Journalists' Adaptation to the New Digital Era. Žurnalistikos Tyrimai. 16: 152–173.
- ESCWA. (2021) Multidimensional poverty in Lebanon (2019- 2021): Painful reality and uncertain prospects. United Nations.
- European Commission. (2023) Lebanon: €60 million in humanitarian aid for the most vulnerable. European Neighbourhood Policy and Enlargement Negotiations (DG NEAR).
- Flores G, Krishnakumar J, O'Donnell O, Van Doorslaer E (2008) Coping with Health-Care Costs: Implications for the Measurement of Catastrophic Expenditures and Poverty. Health Economics. 17(12): 1393-1412.
- GEN. (2023) Genetic Engineering & Biotechnology News (GEN). Cell and Gene Therapy Manufacturing Costs Limiting Access.
- Green B (2023) The 5 Most Expensive Gene Therapies in the U.S. RxBenefits.
- Hardwick Research (2022) Determining Sample Size. Hardwick Research Resources.
- Hart J.T (1971) The Inverse Care Law. The Lancet. 297(7696): 405-412.
- Hartman M, Martin A, McDonnell P (2009) National Health Spending In 2007: Slower Drug Spending Contributes To Lowest Rate Of Overall Growth Since 1998. Health Affairs. 28(1): 246- 261.
- Hejase A.J, Hejase H.J (2013) Research Methods, A Practical Approach for Business Students (Second ed.). Philadelphia, PA, USA: Masadir Inc.
- Hejase A.J, Hejase H.J, Nemer H.A, Hejase C.A, Trad M.-A.M (2020) Repeated Cross-Sectional Survey of Knowledge and Attitudes to Colorectal Cancer Screening in Lebanon. Journal of Biosciences and Medicines. 8(12): 178-210.
- Hejase A.J, Nemer H, Hejase H.J, Honein Abo-Haidar G (2018) Inflatable Colon: A Tool to Raise Awareness of the Importance of Colorectal Cancer Screening. IOSR Journal of Nursing and Health Science (IOSR-JNHS). 7(4): 58-67.
- Hejase H.J, Hejase A.J, Hejase H (2012) Quantitative methods for decision makers: Management approach. Beirut, Lebanon: Dar Sader Publishers.
- Hejase H.J, Fayyad-Kazan H, Hejase A.J, Moukadem I, Danach K (2023) Needed MIS Competencies to the Job Market: Students’ Perspective. British Journal of Multidisciplinary and Advanced Studies: Business and Management Sciences. 4(5): 120-162.
- Hejase H.J, El Dirani A, Haidar Z, Alawieh L, Ahmad A.A, Sfeir N (2024) The Impact of Employee Well-Being on Organizational Effectiveness: Context of Lebanon. International Journal of Human Resource Studies. 14(2): 15-54.
- Hindu Human Rights. (2014) Bayer CEO: New Cancer Medicine for Rich People, Not Indians.
- Hsu C-C, Lee C.-H, Wahlqvist M.L, Huang H-L, Chang H.-Y, et al. (2012) Poverty Increases Type 2 Diabetes Incidence and Inequality of Care Despite Universal Health Coverage. Diabetes Care. 35(11): 2286–2292.
- Hubbard B (2021) Collapse: Inside Lebanon’s Worst Economic Meltdown in More Than a Century. New York Times.
- Human Rights Watch (2022) Lebanon: Rising Poverty, Hunger Amid Economic Crisis.
- Jaggernath J, Øverland L, Ramson P, Kovai V, Chan V, Naidoo K.S (2014) Poverty and Eye Health. Health. 6(14).
- Johnson S.M (2024) Cervical Cancer Screening and Affordability of Medical Care: A Cross-Sectional Study. University of Nebraska Medical Center.
- Khachfe H.H, Salhab H.A, Fares M.Y, Khachfe H.M (2020) Probing the Colorectal Cancer Incidence in Lebanon: An 11-Year Epidemiological Study. Gastrointest Cancer. 51: 805-812.
- Khalife D, Yammine J, El Bazi T (2022) How to Put the Collapsed Lebanese Banking Sector on the Right Track? Arab Economic and Business Journal. 14(1): 31-46.
- Kim Y, Lee J, Kang H, Park S (2018) Effect of medication adherence on long-term all-cause-mortality and hospitalization for cardiovascular disease in 65,067 newly diagnosed type 2 diabetes patients. Sci. Rep. 8(1): 12190.
- Kruk ME, Goldmann E, Galea S (2009) Borrowing And Selling to Pay for Health Care in Low- And Middle-Income Countries. Health Affairs (Millwood). 28(4): 1056-1066.
- LaMattina J (2013) Does Pharma Only Develop Drugs for Those Who Can Pay? Forbes.
- Lee C, Kushi L.H, Reed M.E, Eldridge E.H, Lee J.K, et al. (2022). Impact of the Affordable Care Act on Colorectal Cancer Incidence and Mortality. American Journal of Preventive Medicine. 62(3): 387-394.
- Liu Q.-Q, Yu, M, Wang X-L (2015) Poverty reduction within the framework of SDGs and Post-2015 Development Agenda. Advances in Climate Change Research. 6(1): 67-73.
- Mayo Clinic. (2022) Stem cells: What they are and what they do.
- McAlearney A.S, Reeves K.W, Tatum C, Paskett E.D (2007) Cost as a barrier to screening mammography among underserved women. Ethn Health, 12(2): 189-203.
- Nahvi F.A (2013) The Privilege Gap in Medicine. Academic Medicine. 88(7): 907.
- National Academies of Sciences, Engineering, and Medicine. (2018) Making medicines affordable: A national imperative. Washington, DC: The National Academies Press.
- National Bleeding Disorders Foundation-NBDF. (2024) Hemophilia B.
- National Center for Health Statistics. (2024) Health Status. US Centers for Disease Control & Prevention (CDC).
- OECD (2011) Classification of Health Care Financing Schemes (ICHA-HF). In A System of Health Accounts: 2011 Edition, (pp. 153-191). OECD Publishing, Paris, France.
- Olson E.J (2023) How many hours of sleep are enough for good health? Mayo Clinic. Healthy Lifestyle.
- Ozawa S, Shankar R, Leo C, Orubu S (2019) Access to medicines through health systems in low- and middle-income countries. Health Policy Plan. 34(Suppl 3): iii1–iii3.
- Penalva J (2017) Department of Drama Presents George Bernard Shaw’s ‘Major Barbara’. Syracuse University News.
- Peters D.H, Garg A, Bloom G, Walker D.G, Brieger W.R, et al. (2008) Poverty and Access to Health Care in Developing Countries. Annals of the New York Academy of Sciences. 1136(1): 161-171.
- Pomeroy R (2022) Gene therapy: How can poorer countries access the most expensive drugs in the world? Health and Healthcare.
- Rammal H, Hejase H.J, Hazimeh H (2024) Metaverse Technology and Its Impact on the Evolving Landscape of Communication and Media: A Future Outlook for Lebanese Satellite Channels. Saudi J. Humanities Soc Sci. 9(3): 92-117.
- Rawla P, Sunkara T, Barsouk A (2019) Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Gastroenterology Rev. 14 (2): 89–103.
- Reuters (2002) U.N. Says Essential Drugs Not Sufficient. L.A. Times Archives.
- Riley W.J (2012) Health Disparities: Gaps in Access, Quality and Affordability of Medical Care. Trans Am Clin Climatol Assoc. 123: 167-174.
- Rkein H.I, Hejase H.J, Rkein A, Hejase A.J, Fayyad-Kazan H (2022a) The Use of Banks’ Financial Statements by Depositors and the Impact on Their Decision-Making: A Case from Lebanon. International Journal of Business and Social Science. 13(3): 1-11.
- Rkein A, Hejase H.J, Rkein H, Fayyad-Kazan H (2022b) Bank’s Financial Statements as a Source for Investors’ Decision-making: A Case from Lebanon. Academy of Accounting and Financial Studies Journal. 26(6): 1-14.
- Rkein H.I, Hejase H.I, Rkein A, Hamdar B, Shehadeh M (2024) Future Graduate Competencies: Perception of Lebanese Accounting Graduates, Academics, and Employers. Asian Business Research. 9(2): 1-30.
- Robinson K.M (2023) Navigating the Financial Aspects of CAR T-Cell Therapy.
- Sachs J.D, Lafortune G, Fuller G (2024) The SDGs and the UN Summit of the Future. Sustainable Development Report 2024. Paris: SDSN, Dublin: Dublin University Press. 10.25546/108572.
- Sanders B (2023) Poor people in the developing world have a right to medicine. The Guardian.
- Scripps (2023) How Important Is an Annual Physical Exam? Scripps.
- Seiter A (2007) Access to Medicines and the Innovation Dilemma— Can Pharmaceutical Multinationals be Good Corporate Citizens? In book: Business Ethics of Innovation (pp. 89-100).
- Simoens S, Sinnaeve P (2014) Patient copayment and adherence to statins; a review and case studies. Cardiovasc. Drugs Ther. 28: 99-109.
- Smyth J, Kuchler H (2022) Gene therapies may cure disease but can we afford them? Financial Times.
- Steinbrook R (2007) Closing the Affordability Gap for Drugs in Low-Income Countries. The New England Journal of Medicine. 357: 1996-1999.
- Suh G.-H (2011) High medicine prices and poor affordability. Current Opinion in Psychiatry. 24(4): 341-345.
- Sustainable Development Report. (2024) Middle East and North Africa: Lebanon.
- Terraneo M, Sarti S, Bordogna M (2014) Social inequalities and pharmaceutical cost sharing in Italian regions. Int. J. Health Serv. 44(4): 761-785.
- United Nations Human Settlements Programme - UNHSP. (2011) Lebanon Urban Profile, A Desk Review Report. UN-HABITAT.
- UNStats. (2023) SDG indicator metadata. UN: SDGs.
- Uscher J, Santora T (2024) When to Get a Mammogram. Breast Cancer.
- WHO. (2017a) Access to medicines: making market forces serve the poor.
- World Health Organization (WHO). (2023) Universal health coverage (UHC).
- Wolters Kluwer. (2023) Rising costs of prescription drugs could drive alternate options.
- World Bank and WHO. (2017b) Half the world lacks access to essential health services, 100 million still pushed into extreme poverty because of health expenses. The World Bank/WHO UHC Global Monitoring Report.
- Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, et al. (2007) Protecting households from catastrophic health spending. Health Aff (Millwood). 26(4): 972-983.
- Zaho Z, Chen Y, Francisco N.M, Zhang Y, Wu M (2018) The application of CAR-T cell therapy in hematological malignancies: advantages and challenges. Acta Pharm Sin B. 8(4): 539-551.