Fatemah Salem Al Thallab1, Diaa M. Soliman MD2*, Mohammed Al-Mutairi3, Muna Al Rumh4, Anwar Saad Alanazi5
1Senior Specialist in Public Health, Kuwait Center of Health Information, Ministry of Health, Kuwait
2Junior Doctor, Ministry of Health, Kuwait
3Medical Student, Faculty of Medicine, Kuwait University, Kuwait
4Metro, Head Nurse, Kuwait Center of Health Information, Ministry of Health, Kuwait
5Clark, Kuwait Center of Health Information, Ministry of Health, Kuwait
*Corresponding Author: Diaa M. Soliman, MD, Medical Intern, Ministry of Health, Kuwait.
Abstract
Background: The diversity of COVID-19 is broad and diverse in individuals with or without co-morbid conditions. Unquestionably, COVID-19 is related to many factors.
Aims: We aim to find the frequency of COVID-19 among patients in Kuwait with non-communicable diseases and to find a link between patients with non-communicable diseases and disease outcome and severity.
Methods: A study sample of 731 patients with lab-confirmed COVID-19 in the period between 02/2020 to 06/2020 was included in the study. The co-morbidities included in the survey were type 2 diabetes, cardiovascular diseases, chronic obstructive airway disease, and cancer. Data were collected electronically based on a survey form.
Results: There was a total of 329 diabetic patients (46 %) and 362 patients (49.7 %) with cardiovascular disease in the study with COVID-19 positive status. It was found that diabetes and cardiovascular diseases were associated with hospitalization and worse outcomes among patients with COVID-19. The risk of severe cases was higher in COVID-19 patients with diabetes and cardiovascular diseases, and the risk of death was also higher (P- value < 0.001). In contrast, there was no association between patients with COPD and cancer and disease mortality, severity, and outcomes from COVID-19 (P-value = 0.556, P-value = 0.293, respectively).
Conclusion: There is evidence of increased severity of COVID-19 in patients with non-communicable diseases. Therefore, policymakers may create innovations that may be useful to treat patients with those co-morbidities having an increased emphasis on vaccination prioritization for these groups.
Key Words: Non-communicable diseases, COVID-19, Frequency, Severity
Introduction
Background
The World Health Organization (WHO) declared the COVID-19 pandemic on January 30, 2020. COVID-19 is an infectious disease caused by an RNA virus named coronavirus. It is without a doubt that the COVID-19 pandemic has hit our health drastically; however, COVID-19 causes diverse and different types of diseases in phenotypically other individuals. This pandemic resulted in increased deaths and sicknesses in most of the world's countries. There are about 510 million cases, with about 6.2 million deaths.
The diversity of COVID-19 is broad and diverse in individuals with or without co-morbid conditions. The symptoms, which can be less severe in some, can also be debilitating and life-threatening in others. Of the currently active cases, 99.6 % are in a mild condition and 0.4 % in a severe or critical illness. In addition to either having mild or severe disease, some individuals reported no symptoms. Therefore, some factors aid this virus to be more susceptible to a more severe spectrum of disease progression.
For this pandemic’s pandemic’s prognosis, there is approximately 14 % that have a severe illness, 5 % have a critical condition, and 80 % have a mild form of the disease. They can develop a broad spectrum of symptoms from no symptoms to severe pneumonia, to acute respiratory distress syndrome (ARDS), and finally to multiple organ failure and subsequent death [22]. Therefore, it is unquestionable that COVID-19 is related to many factors. These factors include whether or not the patient has previous non-communicable conditions on top of COVID-19. However, the timing of the symptoms differs. Initially, the symptoms are similar, whether there is the presence of co-morbidities or not. Despite that, studies have shown a worse prognosis for individuals with chronic diseases, such as diabetes (DM), hypertension (HT), or cardiovascular disease (CVD) [21].
The outbreak of this virus and its related complications in different spectrums of various societies has seriously affected the world. It is believed that middle-aged and elderly patients with chronic diseases, such as diabetes, cardiovascular diseases, and hypertension, are susceptible to respiratory failure and may have poorer outcomes [25]. In addition, patients with Chronic Obstructive Pulmonary Disease (COPD) are at a higher risk of more severe disease than those without [20]. The results mentioned above were not limited only to COPD patients; patients with cerebrovascular and cardiovascular diseases were associated with an increased risk for a less-than-advantaged outcome in patients with COVID-19 [26].
Data from different countries correlated the severity of COVID-19 and patients with co-morbid conditions. It was also evident that patients who were already diagnosed with cancer and are currently on anticancer medications are at increased mortality from COVID-19 [23,24]. In this research, we aim to find the frequency of COVID-19 among patients in Kuwait with non-communicable diseases and to find a link between patients with non-communicable diseases and disease outcome and severity. This will further aid to have more effective prevention programs in the community.
Objectives
The main objectives of this study were to find the frequency of non-communicable diseases among patients with COVID-19 infection and to find a link between patients with non-communicable diseases and disease outcome and severity.
Methods
We used the following criteria to define the severity of COVID-19 infection: respiratory distress RR30/min, SPO2 < 93 % at rest, PaO2- Fi O2 < 300mmhg, a patient showing rapid progression (50 %) on CT scan images 24hrs-48 hrs. In addition to respiratory failure, the need for mechanical assistance, shock, and extrapulmonary organ failure was used to define severe cases of COVID-19.
Admission to the intensive care unit was also used to define the severity of COVID-19 cases with non-communicable diseases.
Research Design: This study is a multi-centered retrospective analytical study.
Setting: The study was conducted in the 2 leading general hospitals in Kuwait: Sheikh Jaber Al Ahmad Al Jaber Al Sabah Hospital and Al-Sabah hospital. Patients with non-communicable diseases between February 24 and June 6, 2020, were eligible for inclusion in the study.
Sample and Participants: The study sample was 731 adult in-patients. All patients above 18 years old with lab-confirmed COVID- 19 were included in the study. The co-morbidities included in the survey were type 2 diabetes, cardiovascular diseases, chronic obstructive airway disease, and cancer.
Data collection: Data was collected based on the survey form. An electronic web-based secure double-encrypted database platform, Survey CTO, was used for data entry. Appropriate constraints were placed on the data field to minimize data entry errors. A quality monitoring system was also incorporated into the database platform so that all data entry forms can be re-checked for accuracy and data entry quality.
Data Management and Statistical Analysis: Data were collected and coded, then entered into an IBM-compatible computer using the SPSS version 27 for Windows. Entered data were checked for accuracy and then for normality, using Kolmogorov-Smirnov & Shapiro-Wilk tests, and proved to be normally distributed. Qualitative variables were expressed as numbers and percentages, while quantitative variables were expressed as median, mean, and standard deviation (S). The arithmetic mean was used as a measure of central tendency, while the standard deviation (S) was used as a measure of dispersion. Data analysis was done using the appropriate statistically significant test according to the objectives. A 5% level was chosen as a significance level in all statistical significance tests used.
Ethical Approval: All needed data based on the survey was registered after administrative approval from the Ministry of Health (MOH) in Kuwait. All individuals on whom this research has been carried out have given their voluntary, informed, written consent. The approval number for this research from MOH, Kuwait, is 1490/2020.
Results
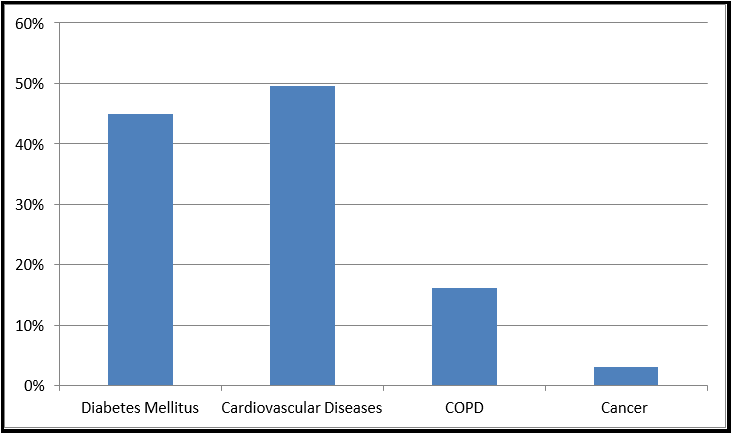
The main objectives of this study were to find the frequency of non-communicable diseases among patients with COVID-19 infection and to find a link between patients with non-communicable diseases and disease outcome and severity. The frequency of co-morbid conditions in patients with COVID-19 infection is illustrated in Figure 1.
Figure 1: Frequency of COVID-19 According to NCD.
There was a total of 329 diabetic patients in the study, with a frequency of 45 %. Regarding cardiovascular diseases, there was a total of 362 patients with a frequency of 49.7 %. There was a total of 118 patients with a confirmed COPD condition, with a frequency of 16.2 %. Finally, there was a total of 22 cancer patients in our study, with a frequency of 3 %.
The following results are further illustrated in Tables 1-7.
Table 1: There was no significant relation when the individual non-communicable diseases were considered. However, when all the four non-communicable diseases were combined, it showed a significant relationship to respiratory rate (P-value = 0.026), where the highest percentage of respiratory rate was 30 b/m, followed by < 30 b/m, and the least was > 30 b/m.
|
Table 1: Relation with the NCD with respiratory rate |
||||||||||||||||
|
Resp Rate |
Total |
DM |
CVD |
Cancer |
COPD |
NCD2 |
||||||||||
|
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
||
|
< 30 b/m |
712 |
322 |
45.2 |
.203 |
354 |
49.7 |
.118 |
22 |
3.1 |
.759 |
116 |
16.3 |
.328 |
505 |
70.9 |
.026 |
|
30 b/m |
8 |
4 |
50.0 |
|
5 |
62.5 |
|
0 |
0.0 |
|
0 |
0.0 |
|
6 |
75.0 |
|
|
> 30 b/m |
8 |
1 |
12.5 |
|
1 |
12.5 |
|
0 |
0.0 |
|
1 |
12.5 |
|
2 |
25.0 |
|
|
Not reported |
3 |
2 |
66.7 |
|
2 |
66.7 |
|
0 |
0.0 |
|
1 |
33.3 |
|
3 |
100.0 |
|
|
Total |
731 |
329 |
45.0 |
|
362 |
49.5 |
|
22 |
3.0 |
|
118 |
16.1 |
|
516 |
70.6 |
|
*NCD2: Combined individual non-communicable diseases
Table 2: Patients’ with diabetes who contracted COVID-19 have a statistically significant relationship with SpO2 (P-value = 0.0053) with the highest percentage of patients having SpO2 of < 93 %, followed by SpO2 = 93 %, and the least was SpO2 > 93 %. On the other hand, there was no significant relationship between the other individual non-communicable diseases and SpO2 among patients with COVID-19.
|
Table 2: Relation with the NCD with spO2 |
||||||||||||||||
|
spO2 |
Total |
DM |
CVD |
Cancer |
COPD |
NCD2 |
||||||||||
|
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
||
|
< 93 % |
20 |
16 |
80.0 |
.005 |
14 |
70.0 |
.178 |
0 |
0.0 |
.503 |
2 |
10.0 |
.502 |
18 |
90.0 |
.093 |
|
= 93 % |
2 |
1 |
50.0 |
|
1 |
50.0 |
|
0 |
0.0 |
|
0 |
0.0 |
|
1 |
50.0 |
|
|
> 93 % |
705 |
312 |
44.3 |
|
347 |
49.2 |
|
22 |
3.1 |
|
116 |
16.5 |
|
497 |
70.5 |
|
|
Total |
727 |
329 |
45.3 |
|
362 |
49.8 |
|
22 |
3.0 |
|
118 |
16.2 |
|
516 |
71.0 |
|
*NCD2: Combined individual non-communicable diseases
Table 3: There was a significant relationship between patients with diabetes, cardiovascular diseases, and NCD2 who had COVID-19 infection and the use of a ventilator (P-value < 0.00, P-value = 0.001, P-value < 0.00 respectively). However, patients with cancer and COPD were not associated with the use of a ventilator (P-value = 0.898, P-value = 0.758, respectively).
|
Table 3: Relation with the NCD with Ventilator Use |
||||||||||||||||
|
Ventilator |
Total |
DM |
CVD |
Cancer |
COPD |
NCD2 |
||||||||||
|
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
||
|
No |
670 |
284 |
42.4 |
.000 |
319 |
47.6 |
.001 |
20 |
3.0 |
.898 |
109 |
16.3 |
.758 |
460 |
68.7 |
.000 |
|
Yes |
61 |
45 |
73.8 |
|
43 |
70.5 |
|
2 |
3.3 |
|
9 |
14.8 |
|
56 |
91.8 |
|
|
Total |
731 |
329 |
45.0 |
|
362 |
49.5 |
|
22 |
3.0 |
|
118 |
16.1 |
|
516 |
70.6 |
|
*NCD2: Combined individual non-communicable diseases
Table 4: Patients with diabetes who had COVID-19 infection were more likely to be in shock (P-value < 0.003). In contrast, there was no significant relationship between the other individual non-communicable diseases and being in shock.
|
Table 4: Relation with the NCD with shock |
||||||||||||||||
|
Shock |
Total |
DM |
CVD |
Cancer |
COPD |
NCD2 |
||||||||||
|
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
||
|
No |
715 |
316 |
44.2 |
.003 |
352 |
49.2 |
.294 |
22 |
3.1 |
.610 |
117 |
16.4 |
.241 |
503 |
70.3 |
.259 |
|
Yes |
16 |
13 |
81.3 |
|
10 |
62.5 |
|
0 |
0.0 |
|
1 |
6.3 |
|
13 |
81.3 |
|
|
Total |
731 |
329 |
45.0 |
|
362 |
49.5 |
|
22 |
3.0 |
|
118 |
16.1 |
|
516 |
70.6 |
|
*NCD2: Combined individual non-communicable diseases
Table 5: Patients with diabetes and cardiovascular diseases who had the COVID-19 infection were more likely to having organ failure (P-value = 0.009, P-value = 0.018, respectively). In addition, when the individual non-communicable diseases were combined, it was revealed that there a significant association between NCD2 and having organ failure (P-value = 0.043). With regards to cancer and COPD, there was no significant relation between patients with cancer and COPD and having organ failure (P-value = 0.203).
|
Table 5: Relation with the NCD with organ failure |
||||||||||||||||
|
Organ Failure |
Total |
DM |
CVD |
Cancer |
COPD |
NCD2 |
||||||||||
|
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
||
|
No |
722 |
321 |
44.5 |
.009 |
354 |
49.0 |
.018 |
22 |
3.0 |
.758 |
118 |
16.3 |
.203 |
507 |
70.2 |
.043 |
|
Yes |
9 |
8 |
88.9 |
|
8 |
88.9 |
|
0 |
0.0 |
|
0 |
0.0 |
|
9 |
100.0 |
|
|
Total |
731 |
329 |
45.0 |
|
362 |
49.5 |
|
22 |
3.0 |
|
118 |
16.1 |
|
516 |
70.6 |
|
*NCD2: Combined individual non-communicable diseases
Table 6: There was no significant relationship between individual and combined non-communicable diseases and the length of stay in the hospital.
|
Table 6: Relation with the NCD with duration admission (LOS) |
||||||||||||||||
|
LOS |
Total |
DM |
CVD |
Cancer |
COPD |
NCD2 |
||||||||||
|
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
||
|
1-5 days |
299 |
145 |
48.5 |
.316 |
156 |
52.2 |
.399 |
8 |
2.7 |
.544 |
57 |
19.1 |
.106 |
219 |
73.2 |
.078 |
|
6-12 days |
216 |
92 |
42.6 |
|
107 |
49.5 |
|
5 |
2.3 |
|
37 |
17.1 |
|
153 |
70.8 |
|
|
13-21 days |
149 |
60 |
40.3 |
|
65 |
43.6 |
|
5 |
3.4 |
|
16 |
10.7 |
|
93 |
62.4 |
|
|
>21 days |
67 |
32 |
47.8 |
|
34 |
50.7 |
|
4 |
6.0 |
|
8 |
11.9 |
|
51 |
76.1 |
|
|
Total |
731 |
329 |
45.0 |
|
362 |
49.5 |
|
22 |
3.0 |
|
118 |
16.1 |
|
516 |
70.6 |
|
*NCD2: Combined individual non-communicable diseases
Table 7: There was a significant association between COVID-19 and mortality among patients with diabetes (P-value < 0.000). In addition, patients with cardiovascular diseases were associated with a significantly greater risk of mortality from COVID-19 (P-value = 0.001). In contrast, there was no association between cancer and COPD and disease mortality from COVID-19 (P-value = 0.293, P-value = 0.557, respectively). However, there was a significant association between COVID-19 and mortality among patients with NCD2 (P-value = 0.007).
|
Table 7: Relation with the NCD with the Final Outcome |
||||||||||||||||
|
Outcome |
Total |
DM |
CVD |
Cancer |
COPD |
NCD2 |
||||||||||
|
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
+ve |
% |
p |
||
|
improvement |
690 |
299 |
43.3 |
.000 |
332 |
48.1 |
.001 |
22 |
3.2 |
.293 |
113 |
16.4 |
.557 |
480 |
69.6 |
.007 |
|
death |
39 |
30 |
76.9 |
|
29 |
74.4 |
|
0 |
0.0 |
|
5 |
12.8 |
|
35 |
89.7 |
|
|
Total |
729 |
329 |
45.1 |
|
361 |
49.5 |
|
22 |
3.0 |
|
118 |
16.2 |
|
515 |
70.6 |
|
*NCD2: Combined individual non-communicable diseases
COVID-19 And Diabetes
There was a total of 329 diabetic patients in the study, with a frequency of 45 %. Our research found that diabetes is associated with hospitalization and worse outcomes among patients with COVID-19. The risk of severe cases was higher in COVID-19 patients with diabetes and the risk of death was also higher (P-value < 0.001). Patients with diabetes who contracted COVID-19 have a statistically significant relationship with SpO2 (P-value = 0.0053), with the highest percentage of patients having SpO2 of < 93 %, followed by SpO2 = 93 %, and the least was SpO2 > 93 %. In addition, there was a significant relationship between patients with diabetes who had COVID-19 infection and the use of a ventilator (P-value < 0.000), being in shock (P-value < 0.003), having organ failure (P-value < 0.009), and being admitted to the ICU (P-value < 0.001). In addition, there was a significant association between COVID-19 and mortality among patients with diabetes (P-value < 0.000). There was no significant relation between diabetic patients and respiratory rate (P- value = 0.203).
COVID-19 And Cardiovascular Diseases
The second most studied chronic illness is cardiovascular disease, including hypertension. Our study had a total of 362 patients with cardiovascular disease, with a frequency of 49.7 %. Similarly, to the case of diabetes, it was revealed that cardiovascular disease is strongly associated with both severity and mortality. Patients with cardiovascular diseases who had COVID-19 infection have a statistically significant association with ventilator use (P-value < 0.001), have organ failure (P-value = 0.018) and are more likely to require ICU admissions (P-value < 0.001). In addition, they were associated with a significantly greater risk of mortality from COVID- 19 (P-value = 0.001).
COVID-19 And COPD
One of the most prevalent chronic illnesses associated with adverse outcomes due to COVID-19 is COPD (chronic obstructive pulmonary disease). There was a total of 118 patients with a confirmed COPD condition, with a frequency of 16.2 %. There was no association between COPD and disease mortality, severity, and outcomes from COVID-19 (p-value = 0.556). Additionally, there was no significant difference in the combined risk of requiring admission to the ICU (P- value = 0.640) and receiving mechanical ventilation (P-value = 0.758) for people with COPD and the risk of death from COVID-19 (P-value = 0.557). It was suggested that COPD is not an independent risk factor for the clinical outcomes of COVID-19. Furthermore, COPD was not associated with an increased risk of hospitalization in patients who contracted COVID-19 (P-value = 0.106).
Covid-19 And Cancer
The fourth co-morbidity that was studied was cancer. Our study had a total of 22 cancer patients with a frequency of 3 %. It was justified that no significant association was found between mortality among COVID-19-infected patients and cancer (P-value = 0.293). In addition, there was no association between patients with cancer and ventilator use (P-value = 0.758), being in shock (P-value = 0.241), having organ failure (P-value = 0.203), and requiring ICU admissions (P-value = 0.640).
Discussion
The current study has significant public health implications with findings regarding the associations between COVID-19 and populations at risk, including those with non-communicable diseases. This pandemic resulted in excessive and vital consequences. To fight against the COVID-19 pandemic, these findings are essential in future planning, risk prevention, and risk stratification in specific communities as more public health awareness is needed to decrease the severity of COVID-19 in patients at risk.
As stated in previous studies, the prevalence of diabetes in COVID- 19 patients varies from 14 % to 44 % [1,2,3, 4]. It was reported that mortality was higher among patients with diabetes compared to non- diabetic patients [5]. In addition, another research reflected similar results as in our study by stating that patients with non-communicable diseases, specifically those with diabetes, are associated with adverse clinical outcomes, including mortality, admission to the ICU, and severe infection in COVID-19 patients [6]. In our study, patients with diabetes who contracted COVID-19 have a statistically significant relationship with SpO2 being < 93 % (P-value = 0.0053), the use of a ventilator (P-value < 0.000), being in shock (P-value < 0.003), having organ failure (P-value < 0.009), and being admitted to the ICU (P- value < 0.000). In addition, our study had a significant association between COVID-19 and mortality among diabetes patients (P-value < 0.000).
A literature review established those cardiovascular diseases, in addition to diabetes and hypertension, are the most prevalent chronic illnesses among COVID-19 patients [7]. The prevalence of hypertension in COVID-19 patients varies from 15.6 % to 22 % [8,9,10]. Another thorough literature review proposes that hypertension was associated with poorer outcomes (risk ratio (RR) 2.1 95 % CI 1.9–2.4) and mortality (RR 2.2 95 % CI 1.7–2.8), severe COVID-19 (RR 2.0, CI 1.7–2.5), ARDS (RR 1.6, 95 % CI: 1.1–2.4), ICU admission (RR 2.1, 95% CI: 1.3–3.3), and disease progression (RR 3.0, 95 % CI: 1.5–6.0) [11]. In our study, similarly to the case of diabetes, it was revealed that cardiovascular disease is strongly associated with both severity and mortality. Patients with cardiovascular diseases have a statistically significant association with ventilator use (P-value < 0.001), being in organ failure (P-value= 0.018) and are more likely to require ICU admissions (P-value < 0.001). In addition, they were associated with a significantly greater risk of mortality from COVID-19 (P-value = 0.001).
One of the most prevalent chronic illnesses associated with adverse outcomes due to COVID-19 is COPD (chronic obstructive pulmonary disease). It was evidenced by a previous study that having lung disease was associated with higher mortality (HR 1.6; 95 %CI 1.2– 2.2) [12]. However, in our research, there was no association between COPD and disease mortality, severity, and outcomes from COVID- 19 (p-value = 0.556). Additionally, there was no significant difference in the combined risk of requiring admission to the ICU (P-value = 0.640) and receiving mechanical ventilation (P-value = 0.758) for people with COPD and the risk of death from COVID-19 (P-value = 0.557). It was suggested that COPD is not an independent risk factor for the clinical outcomes of COVID-19. Furthermore, COPD was not associated with an increased risk of hospitalization in patients who contracted COVID-19 (P-value = 0.106). The findings mentioned above in our study are the opposite of what is already established in previous literature reviews and reflections on this topic; for example, Awortwe et al. [13] indicated that chronic obstructive pulmonary disease worsens the clinical outcomes including mortality, admission to ICU, and severe infection in COVID-19 patients.
Finally, the prevalence of cancer among COVID-19 patients ranges from 1.2 % [14] to 3.5 % [15]. Contrary to other studies, it was justified in our research that there was no significant association was found between mortality among COVID-19-infected patients and cancer (P-value = 0.293). In addition, there was no association between patients with cancer and ventilator use (P-value = 0.758), being in shock (P-value = 0.241), having organ failure (P-value = 0.203), and requiring ICU admissions (P-value = 0.640). On the other hand, previous studies showed a significant association between mortality and severity among COVID-19-infected patients and cancer (RR 2.3, 95 % CI 1.8–3.0) [16].
There are a few hypotheses as to why patients with co-morbid diseases are associated with more pronounced COVID-19 complications. First, it was evidenced that patients with diabetes and cardiovascular disease have increased ACE2 (angiotensin-converting enzyme 2) receptors, which allow the entry of the virus into the host body [17]. On the other hand, despite previous literature reviews that showed a significant relationship between patients with COPD and COVID-19, our study indicated the opposite. This may be due to the decreased gene expression for ACE2 receptors in patients with COPD, which may be protective against COVID-19 infection [18]. Secondly, patients with co-morbid diseases may have an increased risk of severe COVID-19 illness due to the continuous level of inflammation that may result in a "cytokine storm" [19]. This cytokine storm may be hazardous to COVID-19 infection [17].
Conclusion and Recommendations
There is evidence of increased incidence and severity of COVID-19 in patients with co-morbid diseases, such as diabetes, cardiovascular diseases, cancer, and COPD. COVID-19 could have a substantial effect on the pathophysiology of these diseases. This may be due to the two reasons that were previously mentioned: the increased ACE2 (angiotensin-converting enzyme 2) receptor expressions, which facilitates the entry of the virus into the host body; and the hyperinflammatory response, referred to as "cytokine storm."
Based on this, a few recommendations might be added to this research. First, because of times like today and the need to move with today’s technological advances, innovations like telemedicine may help treat patients with those co-morbidities. It would be incredibly beneficial for patients with a higher risk of severe COVID-19 to limit human-to-human interactions and decrease close contact. This may be done virtually rather than being in-person.
Second, because patients with co-morbidities are at higher risk for severe COVID-19 disease, they need careful observation and early intervention. This study showed evidence of the association between the incidence of co-morbidities and COVID-19 and identified further vulnerable groups, including patients with diabetes and cardiovascular disease. Due to this, further study should be conducted on which groups should be prioritized if a vaccination becomes available. The high mortality associated with COVID-19 in these chronic conditions calls for an increased emphasis on future preventative therapies and vaccination programs for these groups.
The COVID-19 pandemic has altered both the global and local landscape. In the future, we may face viral attacks in waves over a long time. Thus, there is an urgent need for a vaccine to combat the virus and for us to benefit from lessons learned in the initial wave of COVID-19. Notably, hospitals must balance bed availability for patients with COVID-19 and non-communicable diseases.
References
- Mahumud RA, Kamara JK, Renzaho AMN (2020) The epidemiological burden of and overall distribution of chronic comorbidities in coronavirus disease-2019 among 202,005 infected patients: evidence from a systematic review and meta- analysis. Infection. 48(6): 813–833.
- Thapa Bajgain K, Badal S, Bajgain BB, Santana MJ (2020) Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature. Am J Infect Control. 49(2): 238-246.
- Qiu P, Zhou Y, Wang F, Wang H, Zhang M, et al. (2020) Clinical characteristics, laboratory outcome characteristics, comorbidities, and complications of related COVID-19 deceased: a systematic review and meta-analysis. Aging Clin Exp Res. 32(9): 1869-1878.
- Hu Y, Sun J, Dai Z, Deng H, Li X, et al. (2020) Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol.127: 104371.
- Yan Y, Yang Y, Wang F, Ren H, Zhang S, et al. (2020) Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care. 8(1): e001343.
- Awortwe C, Cascorbi I (2020) Meta-analysis on outcome- worsening comorbidities of COVID-19 and related potential drug-drug interactions. Pharmacol Res.161: 105250.
- Wolff D, Nee S, Hickey NS, Marschollek M (2021) Risk factors for Covid-19 severity and fatality: a structured literature review. Infection. 49(1): 15–28.
- Hu Y, Sun J, Dai Z, Deng H, Li X, et al. (2020) Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol.127: 104371.
- Emami A, Javanmardi F, Pirbonyeh N, Akbari A (2020) Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis. Arch Acad Emerg Med. 8(1): e35.
- Mahumud RA, Kamara JK, Renzaho AMN (2020) The epidemiological burden of and overall distribution of chronic comorbidities in coronavirus disease-2019 among 202,005 infected patients: evidence from a systematic review and meta- analysis. Infection. 48: 813–833.
- Pranata R, Lim MA, Huang I, Raharjo SB, Lukito AA (2020) Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: A systematic review, meta- analysis, and meta-regression. J Renin Angiotensin Aldosterone Syst. 21(2): 1470320320926899.
- Nachtigall I, Lenga P, Jóźwiak K, Thürmann P, Meier-Hellmann A, et al. (2020) Clinical course and factors associated with outcomes among 1904 patients hospitalized with COVID-19 in Germany: an observational study. Clin Microbiol Infect. 26(12): 1663–1669.
- Awortwe C, Cascorbi I (2020) Meta-analysis on outcome- worsening comorbidities of COVID-19 and related potential drug-drug interactions. Pharmacol Res.161: 105250.
- Hu Y, Sun J, Dai Z, Deng H, Li X, et al. (2020) Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol.127: 104371.
- Bajgain KT, Badal S, Bajgain BB, Santana MJ (2021) Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature. Am J Infect Control. 49(2): 238-246.
- Noor FM, Islam MM (2020) “prevalence and associated risk factors of mortality among COVID-19 patients: a meta-analysis”. J Community Health. 45(6): 1270-1282.
- Singh AK, Gupta R, Ghosh A, Misra A (2020). Diabetes in COVID-19: Prevalence, pathophysiology, prognosis, and practical considerations. Diabetes Metab Syndr. 14(4): 303–310.
- Hughes-Visentin A, Paul ABM (2020) Asthma and COVID-19: What do we know now. Clin Med Insights Circ Respir Pulm Med. 14: 1179548420966242.
- Azar WS, Njeim R, Fares AH, Azar NS, Azar ST, et al. (2020) COVID-19 and diabetes mellitus: how one pandemic worsens the other. Rev Endocr Metab Disord. 21(4): 451-463.
- Alqahtani JS, Oyelade T, Aldhahir AM, Alghamdi SM, Almehmadi M, et al. (2020) Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS One. 15(5): e0233147.
- de Almeida-Pititto B, Dualib PM, Zajdenverg L, Dantas JR, de Souza FD, et al.(2020) Severity and mortality of COVID 19 in patients with diabetes, hypertension and cardiovascular disease: a meta-analysis. Diabetol Metab Syndr. 12: 75.
- Huang I, Lim MA, Pranata R (2020) Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia - A systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 14(4): 395-403.
- Lee LY, Cazier JB, Angelis V, Arnold R, Bisht V,et al. (2020) COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study.Lancet. 395(10241): 1919-1926.
- Lee LYW, Cazier JB, Starkey T, Briggs SEW, Arnold R,et al. (2020) COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol. 21(10): 1309-1316.
- Liu H, Chen S, Liu M, Nie H, Lu H (2020) Comorbid Chronic Diseases are Strongly Correlated with Disease Severity among COVID-19 Patients: A Systematic Review and Meta-Analysis. Aging Dis. 11(3): 668-678.
- Pranata R, Huang I, Lim MA, Wahjoepramono EJ, July J (2020) Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19-systematic review, meta-analysis, and meta-regression. J Stroke Cerebrovasc Dis. 29(8): 104949.