Abderrahmane Housni1*, Imadeddine Sahri1, Zakariaa Chandide Telmçani1, Essanaa Badr, Mustapha Hemama2, Nizare El Fatemi2, El Maaqili My Rachid2
1Military Hospital Mohamed V of Rabat
2Hopital Ibn Sina Rabat
*Corresponding Author: Abderrahmane Housni, Military Hospital Mohamed V of Rabat
Abstract
Ventriculoperitoneal (VP) shunt has a long list of know complications such as infection, obstruction, over drainage, intraventricular hemorrhage, etc… But a postoperative epidural hematoma after Ventriculoperitoneal shunt insertion is unusual in adults, especially when the epidural hematoma is formed far from the site of the shunt insertion.
We report in this article the case of a 19-year-old female who has been diagnosed with a central neurocytoma complicated by obstructive hydrocephalus, medium pressure ventriculoperitoneal shunt was placed through a right temporooccipital burr-hole.
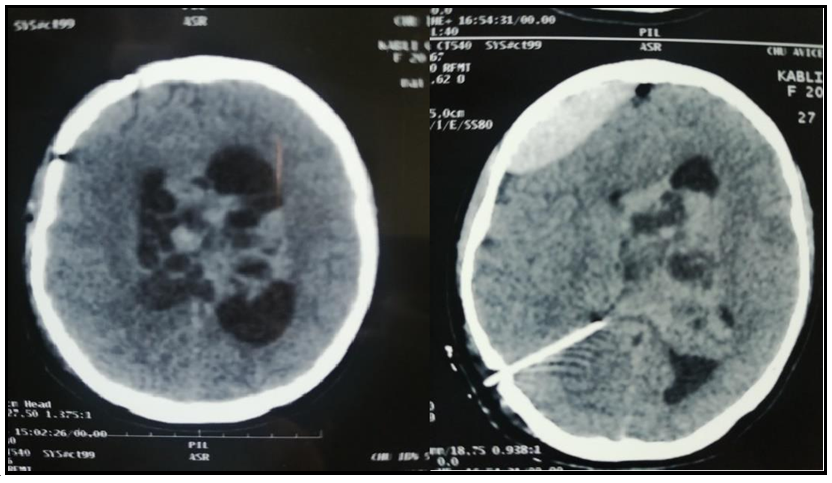
A CT scan was released the 2nd postoperative day to verify the position of the shunt resulted in the discovery of a right frontal EDH which was evacuated immediately by craniotomy
Keywords: hydrocephalus, Epidural hematoma, neurocytoma, ventriculoperitoneal shunt.
Introduction
Ventriculoperitoneal (VP) shunting is a common surgical procedure allowing long-term management of hydrocephalus. This condition occurs when excess cerebrospinal fluid (CSF) collects in the brain’s ventricles. The constitution of an epidural hematoma (EDH) after VP shunt is widely reported in the pediatric population. But in the adult population, subdural hematomas (SDH) are much more reported in comparison to EDH which very few cases have been reported. In this paper, we present the case of a neurocytoma with hydrocephalus initially treated by a VP shunt, which is complicated by EDH at a site distant from shunt insertion. We remind that EDH is a potentially life-threatening complication and represents, in consequence, a neurosurgical emergency.
Case report
A 19 years old girl was admitted to our department with a severe headache and seizures, the investigations let us find a central neurocytoma which is a rare benign brain tumor often located in the lateral ventricles, in this case, it causes obstructive hydrocephalus, Our team decided to realize a VPS in order to manage the hydrocephalus at first, medium pressure ventriculoperitoneal shunt was placed through a right temporooccipital burr-hole.
The patient was extubated with a GCS 15, the seizures disappeared, the headache did seriously decrease, and her physical exam was normal.
In order to confirm the catheter emplacement, a CT scan was performed 18 hours later, the shunt was found to be in the proper position at the right occipital horn f the lateral ventricle and functioning well, the hydrocephalus start to decline, however, we found an important right frontal EDH which was away from the site of the first surgery. We must insist that the coagulation profile including prothrombin time, international normalized ratio (INR) were normal.
The EDH remains asymptomatic but in front of its size we decided to evacuate it immediately,
The patient underwent an urgent frontal craniotomy, during surgery we could not identify any origin of bleeding, Postoperative CT showed the complete removal of the hematoma.
The patient was extubated, GCS 15, with a normal physical exam.
Figure 1: CT scan shown the right emplacement of the drain and the extradural hematoma
Figure 2: CT scan ctrl shown the correct evaluation of the hematoma
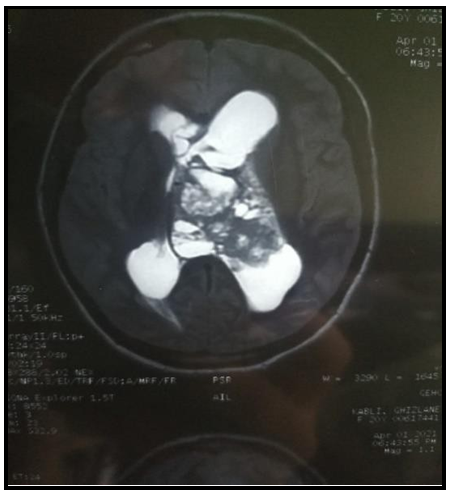
Figure 3: MRI shown the central neurocytoma
Discussion
VPS is a common procedure in neurosurgery practice, and management of hydrocephalus, however, we usually find some complications like infection, obstruction, or detachment. The bleeding complication in such an operation remains rare in the adult population [2], especially the EDH, as reported by FUKUMACHI the incidence of EDH is about 0.4 % [1], it is more frequent for the pediatric population. The incidence of epidural hematoma after ventricular shunt operation was 5.6 % in adults and 0 % in children before the advent of valve-regulated shunt [6]
As we already know Acute extradural hematoma is a potentially life-threatening complication, and its management should be urgent. The mechanism of the EDH as a complication of a VPS remains incompletely understood, for the pediatric population, some authors report that the bleeding is due to the low adhesion of the dura to the skull, in this age group and can be stripped off in a case of rapid decrease in the intracranial pressure [3] the interest of our case is that the EDH was developing away from the site of surgery which is an uncommon condition, according to our review of littérature the first case of an EDH far away from the burr hole insertion was reported by Ali YS and al [5] they suggest that the rapid decrease of the intracranial pressure can lead to an EDH even if the patient is adult, they also recommend to use high-pressure valve rather than the medium one, [5]
The manifestation of the EDH can be by seizures, a decrease of consciousness, headache or in some rare cases as our, the patient was asymptomatic it can be explained by the frontal localization which is less dangerous than parietal or temporal and also the bleeding may be so slow [4] some authors recommend Precautions during shunt insertion [6] and early detection by a close observation after surgery can prevent mortality and severe morbidity in these cases, in the paucisymptomatic cases we must underly the importance of the ct scan control.
Conclusion
EDH Following VP shunt is rare, can be totally asymptomatic, like in our case, or causes a headache, deficit syndrome in extreme cases. When it’s formed in a distant site from shunt insertion, which is exceptional, it does not require an ablation since there is no risk of obstruction of the valve, but the evacuation by craniectomy emergently is indisputable.
References
- Fukamachi A, Koizumi H, Nukui H (1985) Postoperative intracerebral hemorrhages: a survey of computed tomographic findings after 1074 intracranial operations. Surg Neurol. 23(6): 575-80.
- Noleto G, Neville IS, Tavares WM, Felippe S, Pinto FC, et al. (2014) Giant acute epidural hematoma after ventriculoperitoneal shunt: A case report and literature review. Int J Clin Exp Med. 7(8): 2355-9
- Fujimoto Y, Aguiar PH, Carneiro JD, Martins RS, Jr Ciquini O, et al. (1999) Spontaneous epidural hematoma following a shunt in an infant with congenital Factor X deficiency: Case report and literature review. Neurosurg Rev. 22(4): 226-9.
- Vinay B, Shruti R, Bhadrinarayan V (2015) Delayed incidental diagnosis of postoperative extradural hematoma following ventriculoperitoneal shunt. J Neurosci Rural Pract. 6(1): 94-6.
- Ali YS, Dagar A, Reyaz AA, Gupta LN (2016) Remote Acute Extradural Hematoma Formation after Ventriculoperitoneal Shunt - A Rare Occurrence. Int Arch BioMed Clin Res. 2(1): 29- 31
- Etemadrezaie H, Zabihian S, Baharvahdat H, Ganjeifar B (2015) Acute Epidural Hematoma after Ventriculoperitoneal Shunt Insertion: A Case Report. Iran. J. Neurosurg. 1(3): 30-32.