B.P.N.Wijerathne1, S.H.S.Sineka2*, M.A.M.N.Bandara3 , B.I.Thanthrige4
1Consultant Surgeon, Teaching Hospital Kuliyapitiya, Sri Lanka
2Relief House Officer, Teaching Hospital, Kuliyapitiya, Sri Lanka
3Medical Officer, Teaching Hospital, Kuliyapitiya, Sri Lanka
4Intern House Officer, Teaching Hospital Kuliyapitiya
*Corresponding Author: S.H.S.Sineka, Relief House Officer, Teaching Hospital, Kuliyapitiya, Sri Lanka.
Introduction
Ano-genital warts are sexually transmitted disease entity, caused by Human Papilloma Virus (HPV). Treatment is either surgical or non- surgical such as cauterization, local applications. However, in extensive disease surgical excision would be the most effective way of treatment. Here we present a case of extensive ano-genital warts in a female and her surgical treatment.
Case Illustration
55-year-old female presented with proliferative type perineal growth around anus, vulva and natal cleft. She has had localized perineal warts first in 2011 and cauterized with liquid nitrogen therapy. Then the Histology was compatible with Verruca vulgaris. Cauterization and IMIQUIMOD local application controlled her warts, but not totally eradicated and no regular follow up. In 2023 she presented with a warty lesion in the perineal area as described above. Due to the worsening of symptoms such as itching and oozing (Figure 1 a, b, c) she did not have urinary or defecation problems. She did not have any significant past history of immune suppression.
Neither she nor her husband has had high risk sexual behavior. As she defaulted follow-up, no records of HPV, HIV, HBV, HCV were found. No family members having similar problems. No history of other STI. She has not had overseas contacts or employment.
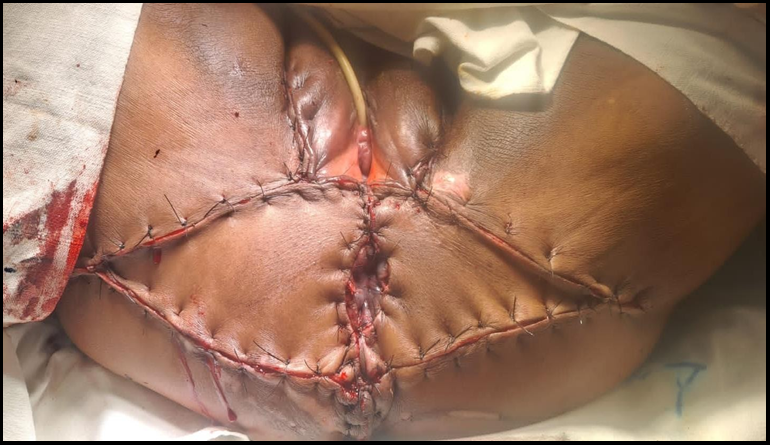
During this admission we excised whole lesion with at least 5mm clearance of free margin all around the whole lesion and sample sent for histology. De-functioning sigmoid colostomy was performed during same procedure. After a few days’ skin cover was achieved with local advancement flaps and skin mobilization and primary closure in same area (Figure 3). Other options of skin cover are skin grafting, musculo-cutaneous flaps from the thigh or abdomen. She recovered though she got a minor catheter related urinary tract infection.
Discussion
Genital warts are sexually transmitted diseases. Commonly it is caused by HPV which has more than 100 genotypes. According to the previous histology this patient was having benign common viral warts, Verruca vulgaris. (Ex type 2,6,11). This patient was investigated for cervical poly back in 2011 and found to have only endo-cervical polyp and pap smear negative. She presented this time with more extensive genital warts suggestive of condyloma acuminatum. Other than that CD4 counts impact on wound healing [5].
Figure 1(a,b,c): Warty lesions in perineal area
Figure 2: Excised whole lesion
Figure 3: Flap advancement and primary closure
We suppose it is ideal that we rescreen this patient for HSV, HIV, HPV, HBV, and HCV for the identification of relevant infections and gear on management.
For treatment options for warts are non-surgical such as cauterization and local applications (IMIQUIMOD) and surgical excision. Patient’s deviation from medial management is solely due to the severe pain following cauterization with poor response to oral analgesics. However for large extensive condyloma surgical excision is recommended [1]. In that case surgical excision and inward nursing benefitted the patient to satisfy the therapy. Furthermore, the rapid and aggressive nature of this flare up might cause malignant transformation of the HPV lesion (Type 16,18) [2]. However, upon resection no aggressive down growth to dermal structures were noted. This much of a big lesion may warrant primary surgical options than medical therapy as the whole lesion can be excised at the same time [3]. But the skin cover in the large lesion is a technical challenge in this area. Warts have been grown to this big size mainly due to the cultural and social issues. People in this culture is shy to come out with problems in that area and socially embarrassed to expose as they feel guilty about the disease.
Problem of leaving without treatment will cause psychological issues, which might lead to severe distress and even suicide, physical effects such as pain and affects in the bladder.
These are pre malignant conditions and as long term can transform into cancerous lesions [6]. If transformed these can be invasive squamous cell carcinoma (SCC) and its common in immunocompromised patients. Foci of invasive carcinoma notes in 50% and carcinoma in situ in 8% [4].
References
- Aldabek K, Elbakry AA, Gelman J, Fooks H (2022) Management of a case of extensive penile condyloma acuminata with full thickness skin graft for penile skin reconstruction. Urology Case Reports. 45: 102212.
- Chondros K, Grekos K, Klambatsas A, Dimasis N (2018) ‘Extensive anogenital warts: A multidisciplinary surgical management’, Pan African Medical Journal. 30: 277.
- Yunir PE, Mochtar CA, Hamid ARAH, Sukasah CL, Umbas R (2016) Surgical Management of Giant Genital Condyloma Acuminata by Using Double Keystone Flaps. Case Reports in Urology. 2016: 4347821.
- Mingolla GP, Potì O, Carbotta G, Marra C, Borgia G, et al. (2013) Reconstructive surgery in anal giant condyloma: Report of two cases. International Journal of Surgery Case Reports. 4(12): 1088–1090.
- Uribe N, Millan M, Flores J, Asencio F, Díaz F, et al. (2004) Excision and V-Y plasty reconstruction for giant condyloma acuminatum. Techniques in Coloproctology. 8(2): 99–101.
- Zekan J, Petrovic D, El‑Safadi S, Banovic M, Hulina D, et al. (2013) ‘A surgical approach to giant condyloma (buschke- löwenstein tumour) with underlying superficial vulvar carcinoma: A case report. Oncology Letters. 5(2): 541–543.