Syed Intesar Burni, Ph.D.1, Fareeha Nadeem, MBBS2, Fareena Khalil Ahmed, MBBS3, Raahim Salman Abdul Ghaffar, B.D.S4, Tazeen Saeed Ali, Ph.D.5*
1Director, National Research Institute for Fertility Care, Ministry of Health, Karachi, Pakistan
2Deputy Director, National Research Institute for Fertility Care, Ministry of Health, Karachi, Pakistan
3Associate Professor, Sir Syed College of Medical Science for Girls, Karachi, Pakistan
4Research Coordinator, Aga Khan University, Karachi, Pakistan
5Interim Dean, School of Nursing and Midwifery, Department of Community Health Science, Aga Khan University, Karachi, Pakistan
*Corresponding Author: Tazeen Saeed Ali, Ph.D., Interim Dean, School of Nursing and Midwifery, Department of Community Health Science, Aga Khan University, Karachi, Pakistan.
Abstract
Objective
As more and more cases of male infertility at a young age are being come forward, the attention is diverted toward the causes of infertility. The objective of this study is to find the association between male infertility and the distribution of different ethnic groups in Pakistan and the association of age with sperm concentration and pH among infertile men.
Material And Method
This study has been carried out in Karachi, Pakistan. This city has almost 14 to 15 million population with diverse ethnic groups from Punjab, Sindh, Baluchistan, and N.W.F.P. The subjects were males, through purposive sampling, who visited the organization or healthcare provider for the complaint of infertility. A quantity of 881 subjects were the participants of this study. Demographic details and their semen samples were taken, with their consent. Evaluation is done, mainly focused on age, sperm concentration, and pH. Mainly.
Results
The non-identical results from each provenance keep us with the idea that infertility is affiliated to the ethnic standings. The group residing in Karachi, from Punjab and Karachi, were mostly oligozoospermic, whereas the azoospermia and asthenozoospermic subjects relate to the area of N.W.F.P. and Northern Pakistan. Also, results show that age is not related to sperm concentration and pH among infertile males.
Conclusion
It has been concluded that differences in reproductive function are also based on ethnicity and should be treated on an individual basis for the proliferation of fertility ratio. Also, age is not associated with sperm concentration and pH.
Keywords: Male infertility, Ethnicity, Karachi, Pakistan, Age, pH., Sperm concentration
Introduction
Infertility of males is being the part of attention due to its worldwide prevalence and evidence of the decline in semen quality of young healthy males [1]. According to many previous studies, lifestyle, nutrition, and environment have a remarkable impact on male infertility. Intake of food and its association with reproductive health like alcohol or caffeine [2,3], the lifestyle males adopt, which affects the male physically as well as hormonally, like obesity [4,5], the environment the male is going through like industrial hazards, water contamination, and polluted air, all have some sort of link with infertility [6,7]. Although the human desire to have children is deeply ingrained, as many as 15% of all couples experience some form of infertility; of these cases, ~50% are due to infertility of the male partner. [8] Nearly 7% of the male from the general population are suffering from a lack of fertility [9], Several factors including varicoceles, hormonal imbalance, testicular trauma, anatomical abnormalities of reproductive systems, chromosomal abnormalities, and Y chromosome microdeletions have been associated with it. However, 30% of cases of infertility are still unexplained and defined as idiopathic infertility, and in at least 15% of cases, this condition is related to genetic disorders [9].
Male infertility is a multifactorial complex disease with highly heterogeneous phenotypic representation, and in at least 15% of cases, this condition is related to known genetic disorders, including both chromosomal and single-gene alterations[9]. The factors could be modifiable and non-modifiable. The Non-modifiable includes genetic factors in which studies show that Moroccan, Asian, and Caucasian infertile male has the MTHFR 677T polymorphism, NR5A1 mutations associated with fertility, or azoospermia [10]. The human Y chromosome mutation also has the highest prevalence in American and East Asian infertile men [11] Some studies have also shown that there is some social behavior that is also related to ethnicities like Sleep duration, Occupational hazards, Regional clothes, and many more.
Short sleep duration and poor sleep quality are increasingly prevalent in modern society. To investigate that 842 healthy men were screened as potential sperm donors using the Pittsburgh Sleep Quality Index (P.S.Q.I.). [12]
Men who slept less than 6.0 h/d and higher than 9.0 h/d had lower sperm volume of 12%and 3.9% respectively, compared to those who slept 7.5-8.0 h/d [12]. Also, Compared to men with a night sleep duration of 7.5–8.0 h/d, the men who slept less than 6.0 h/d had lower total and progressive sperm motility of 4.4%. This shows that both longer and shorter sleep duration can cause a decrease in sperm quality [12]
In the same way, active sperm production is dependent on an environment of the testis that is 3 to 4°C lower than the normal body temperature [13]. An early investigation on the effect of sauna bathing demonstrated a transient decrease in sperm count in 12 voluntarily exposed men; they stayed on the average 15 minutes in the sauna bath eight times over a 2-week period. The study group welders experienced a reversible decrease in semen quality, possibly caused by the moderate exposure to radiant heat. Sperm morphology showed deterioration during 6 weeks of exposure and increased after a break in the exposure. [13]
Older studies show that the age-related decline in fecundity for men is more controversial. Male fertility peaks at about 35 years of age and declines sharply after 45 years of age. However, men have reportedly fathered children into their 80s (S. Samal, 2012). There are many variations that were noted as the age of the men increases, which are volume (Homonnai ZT, 1982) (H.Barad M.D., 1995), semen concentration [14], sperm motility [15,16] and sperm morphology [17,18]
Of these numerous constituents that are responsible for male infertility, this study aims to evaluate that ethnicity also plays a role in male reproductive health. Also, how does age affect the pH and concentration of the semen?
Material And Method
This study was conducted in Karachi, Pakistan, on adult males who were patients at the clinic visited for complaints of infertility. The patient is then evaluated and diagnosed by the physician and considered as the participant of the study after they met the definition of infertile i.e. one year of unprotected intercourse not leading to conception. In this way, the participants were recruited through purposive sampling. This study was approved by the ethical committee, Basic Medical Science Institute, Jinnah Post Graduate Medical Centre, with ERC no. F.1-2/2019/BMSI- E.COMT/FK/JPMC, in which the subject of 881 infertile men was clinically evaluated, including 48 fertile men who were (proven) fathers before, i.e., females had already given birth to the children with the sperm of these participants. The range of age of the fertile and infertile subjects were chosen between 22 to 57 year (mean: 33.05), with the mean duration of infertility was 9 years (3-14)
First, the subjects were evaluated by the urologist for physical and genital examination. The subjects were then evaluated through demographical questions like Identifying data (name, age, residence, ethnic group, B.M.I.- height - weight), contraceptive practice (if any), any drug for treatment (previous history) if live birth is still child alive (yes/no), does the woman want to get pregnant (yes/no), the number of previous marriages of husband, did any former wife become pregnant by him : (yes/no), the number of additional wives, any of these wives get pregnant by him, duration of the marriage, parity, Ethnic origin, duration of infertility, the fertile status of the martial partner and Laboratory parameters of the samples
Male subjects were evaluated for semen analysis. Semen and blood samples were collected by their consent, for the evaluation of semen and other tests which were mandatory for the evaluation of infertility. The sample was collected through daily visits to the healthcare department over the period of five years (2018-2023). The semen sample was collected by masturbation into the non-sperm toxic container at the clinic in the private room and handed to the laboratory technician.
Initially, the semen was left to liquefy (commonly for 15-30 minutes). Once done the semen was examined for colour, P.H., volume, and consistency. The motility of the sperm was evaluated quantitatively by counting motile and immotile sperm in 10 separate, randomly selected fields. The sperm concentration was determined by the preferable hemocytometer method. The pH. of the semen was determined by spreading evenly a drop of semen on the standard (1- 14) range pH. paper and after 30 seconds the color of the zone on which the sample was placed was matched with the calibration strip. All these examinations were compared according to the parameters of WHO (2010). The analysis was carried out to difference among the variables between all infertile and fertile participants. The descriptive analysis is performed to show the ethnic relation to male infertility. Based on semen analysis, subjects were categorized as Oligozoospermia, Azoospermia, Normozoospermia, and Asthenozoospermia. However, a few cases of impotency and very lowT-values are also considered.
The nomenclature of these categories of male infertility as generally accepted and standardized values of semen parameters recommended by WHO (2010) are defined as.
Oligozoospermia – total number (or concentration, depending on outcome reported) of spermatozoa below the lower reference limit. Azoospermia – no spermatozoa in the ejaculate Normozoospermia- total number (or concentration, depending on outcome reported) of spermatozoa, and percentages of progressively motile (P.R.) and morphologically normal spermatozoa, equal to or above the lower reference limits.
Asthenozoospermia- the percentage of progressively motile (P.R.) spermatozoa below the lower reference limit.
|
Parameters |
Lower Reference Limit |
|
Total Sperm Numbers (104 per ejaculation) |
39 (33-46) |
|
Progressive motile (PR%) |
32 (31-34) |
|
pH |
≥7.2 |
Results
The mean duration of infertility was 9 years (3-14). Their ages ranged from 22 to 57 years (mean: 33.05). The subjects who were proven fathers were also of the same age as another infertile male. The results show that of the total participants with infertility, 27% were oligospermic and 16.9% were azoospermic subjects, however, there were 24.7% infertile and identified as asthenozoospermic. At the same time, 1/3 of the population, which is 25% has normal semen analytical data. The percentage of impotency (1.6%) is negligible.
Ethnic Distribution
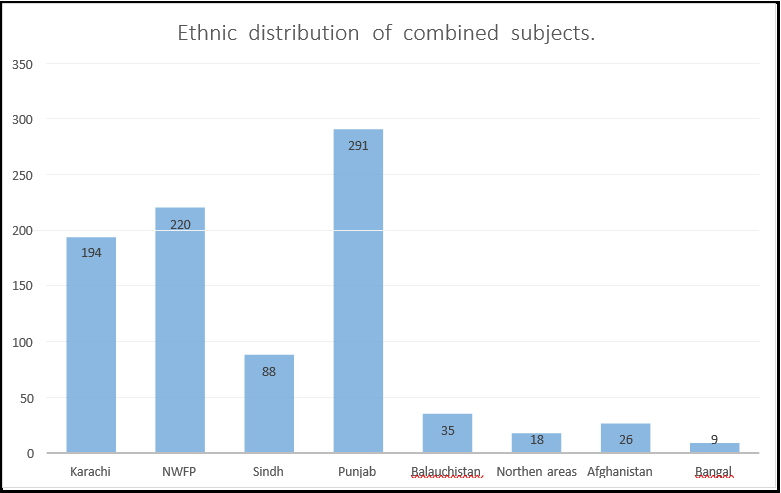
Based on ethical relationships most of them belonged to Punjab with the highest numbers of 291 (33.7%), after that NWFP occupied the size of 220 (27.4%), later Karachi had the most infertile males with 194 (21.9%) participants, and then Sindh with 88 (10.05%) participants. Other lower size participants include Baluchistan, Northern area, Afghanistan, and Bengal with the participants size of 35(2.28%), 18(1.37%), 26, and (2.28%) 9 respectively (Figure 1)
Categoric Distribution
Also, it is found that impotency rate is highest in the participants belonging to Punjab (50%). Oligozoospermic patients mostly belonged to Karachi and Punjab (31% each) whereas the azoospermia and asthenozoospermic subjects were mainly from NWFP (40% and 22%) and Punjab (34% and 40%).
|
Origin |
Father |
Normozoospermia |
Impotent |
Azozoospermic |
Asthenozoospermic |
|
Karachi |
35.42% |
31.11% |
14.29% |
11.76% |
18.52% |
|
NWFP |
20.83% |
13.33% |
28.57% |
40.00% |
22.22% |
|
Sindh |
12.50% |
15.56% |
7.14% |
4.71% |
14.81% |
|
Punjab |
27.08% |
31.11% |
50.00% |
34.12% |
40.74% |
|
Baluchistan |
2.08% |
4.44% |
0.00% |
1.18% |
3.70% |
|
Northern Area |
2.08% |
0.00% |
0.00% |
2.35% |
0.00% |
|
Afghanistan |
0.00% |
4.44% |
0.00% |
3.53% |
0.00% |
|
Bengal |
0.00% |
0.00% |
0.00% |
2.35% |
0.00% |
There was no significant difference between different age groups with respect to sperm concentration and pH of the proven fathers. Azoospermia, refers to the condition where patients do not have sperm present in their ejaculate that is why, also shows no difference in sperm concentration and pH between different age groups. Oligospermia shows a decrease in sperm concentration with increased age. The sperm concentration of asthenospermia was noted highest at the age of 20-25 (>50 million/ml)
|
CATAGORIES |
AGE |
|||||
|
21-25 |
26-30 |
31-35 |
36-40 |
41-45 |
||
|
Proven Fathers |
Sperm Concentration |
109.40±25.39 |
86.00 ± 11.94 |
76.62±16.42 |
82.24±13.51 |
10.50±0.00e |
|
Ph |
7.50±0.00 |
7.56±0.06 |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
|
|
Azoospermic Subjects |
Sperm Concentration |
00.00 |
00.00 |
00.00 |
00.00 |
00.00 |
|
Ph |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
|
|
Oligozoospermic Subjects |
Sperm Concentration |
11.40±4.27 |
6.97±1.79 |
8.90±2.41 |
8.98±1.71 |
7.00±0.00 |
|
Ph |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
|
|
Asthenozoospermic Subjects |
Sperm Concentration |
103±28.00 |
53.84±8.96 |
62.71±22.06 |
67.40±26.90 |
43.00±0.00 |
|
Ph |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
7.50±0.00 |
|
Discussion
According to previous studies, it was acknowledged that ethnicity is the major cause of male infertility. Many males remain undiagnosed due to the ethnic difference or due to the genetic difference from male of different origin. Also, factors, like sleep disturbance, traditional clothing, weather, and workplace environment, which can indirectly be the outcome of male infertility have an association with the geographical civilization.
In Pakistan, Karachi is known as a city of lights as most of its business hubs continue to commence late at night. People in this city usually get up late in the morning and start their job mostly at 12 pm or 1 pm andstay up late till night which causes a serious disturbance in their sleep hours. Karachi has a greater prevalence of shorter and longer sleep [19] Several studies have concluded that sleep duration may link with the semen quality of males. As short and long duration may affect the semen quality and motility up to 3-5% or some other studies show 12-15% [12] Like Karachi, some areas of Punjab does have the same daily spending’s but mostly like NWFP, Baluchistan and some area of Punjab do start their day with the sunrise and end with the sun sets. So, it needs to figure out that when these people, from the remaining part of Pakistan, move to Karachi, have a serious disturbance in the continuation of their sleep and daily passing does this affect the fertility status of the man, and moving to Karachi has the participation in that.
Recent studies also relate infertility to the increase in the age of men. Advanced male age has been associated with Signiant reductions in pregnancy rates, increased time-to-pregnancy, and increased sub- fecundity [20] Heat and the occupational environment may also affect the semen quality and quantity. [21,22] Men who mostly work in the naked sun or are habitual of living in a warm environment like gulf countries or having a sauna bath daily have the main association with the lower semen count. The environment of Karachi usually has sunny weather and the temperature here is almost 25.9 degrees Celsius annually [23]. The highest temperature recorded was 44.8 °C and the combination of extreme humidity and the high temperature was the driving factor of this serious event [23]. Here in winter, the weather is quite bearable as compared to the northern side of Pakistan. On the other hand, In Punjab temperature varies between − 2 and 45°C but can reach as high as 47 °C in summers and as low as − 5 °C in winters [24]. Likewise, NWFP is also the colder region of Pakistan. The body of people who are living in those regions compensate for that environment, but moving from colder to warmer region can have some sort of effect on their bodies [25].
Also, Karachi is considered the big city of Pakistan and people here are living in their modern branded getups like jeans and pajamas [26]. The living fashion of Karachi is adopted by the people who came from Punjab Baluchistan and NWFP, where the traditional wearing is practiced, which includes loose salwar and kurta. Tight clothes do affect [27], that circulation and also cause heat production over the testes of males which certainly be the cause of infertility. But fortunately, this is reversible once the subject removes or changed his surrounding after about 25-35 days [13,28]. Also, the men who are working with the chemicals like Di bromochloropropane, which is used in pesticides, or under radiation or metal which are lethal to human health like lead, may report infertility. [13] Karachi is an industrial area and working in this environment may change the body normally for people who have come from other parts. Water is also, the major cause of infertility in males. As discussed in the previous studies different areas of water have different concentrations of impurities in them. The most common ones are organic pollutants such as oil and pesticides. Inorganic pollutants include anions and cations (sulfate, nitrate, phosphate, fluoride, chloride, calcium, magnesium, sodium, and potassium), pathogens (bacteria, protozoa’s, and viruses), and radioactive substances that are water-soluble [29]. Selenium present in the water is also somehow related to the status of male infertility. a small deviation, either deficiency or excess, leads to abnormal development [30] A maximum acceptable concentration of 10 μg/L has been specified for selenium in drinking water by the federal and provincial regulatory agencies [31]. People living on the northern side of Pakistan usually consume water rich in minerals and metals. In Karachi, people consume mineral water in which arsenic and selenium are removed [32], which may affect males for their reproductive health.
The education and literacy rate of the population do also link with the health of male infertility. Pakistan has only 56% of literacy rate [33] which shows that almost half of the population is lacking about the basic knowledge, Despite a very low average literacy rate, however, there are exceptional cases where the rate is very high; for example, in Lahore, Islamabad and Karachi. In these cities, the literacy rate is almost 75% [33], and due to the lack of education, the population get more chances to be infected. and research tells us that the education of health care staff can improve infection control practices as it has previously been demonstrated that increased compliance with precautions [34] and lack of education increases the risk of spreading the infection, which somehow affects male infertility [35]
Conclusion
The conclusion of the study is that people residing in the Karachi belongs to the different origin, based on ethnicity, has different volume of population for male infertility also sperm concentration and pH are not associated with age.
Future Recommendations
Keeping the results Infront of this study, it has been recommended for the future researcher that, All patient has to be specific, and each individual must be assessed to identify the cause in order to alleviate fertility- associate problem.
There should be further studies done for the clearance of the query regarding the variation in the results of the participants belonging to the different ethnic groups and further assemble the mind about the association of infertility with the migration from one region to another. Researcher in future should collect the data of the infertile male that if this problem present before the migration or it occur after moving to another place.
Reader of the study must also gain confidence and improve the awareness among the healthcare provider regarding ethnic consequences. It would provide awareness between the healthcare provider, that each patient may be treated according to their ethnical history and the effects which their body has gone through after the migration. This will help restore the confidence of the public in general and the infertility population in particular in medical science and may stop infertile couples from turning toward quacks.
In the end results of this study, it is recommended that there is a lot more space to be filled in this relevance that those people who came from a different region to Karachi and have the complaint of infertility, do the cause of it, is the migration to that region which is warmer, polluted, unrelated sleep schedule which is all connected to infertility at some position or they face this, if they were in their native respected regions.
The environmental change, usually regarding nutrition and water, containing higher selenium and arsenic concentrations, which is harmful to male fertility health, should be the center of future research if shifting from ground to mineral water can create trouble for their reproductive health.
But in this study, the direct link between age and infertility wasn't able matched which shows the least association between age and infertility.
Due to the lack of awareness and policy guidance in Pakistan, people ended up visiting the quacks and making the assumption that was made with just inappropriate past scenarios which lead to the patient nothing but more harming himself. So, we are in a greater need to focus on male infertility policy making, which has gotten reduced attention because of the population growth stress.
Policy Relevance
The clinician must adopt such a method to gain a friendly relationship with the patient, otherwise, the people will be lost to the quacks, which can lead them, apart from gaining any benefit, to harm the health but also to their wealth. In Pakistan, quakes are advertising their services through newspapers, banners, and even written on the wall of the many streets all across Pakistan. For that, now, the government bears the burden of making and maintaining the policy for these individuals, which should be a person-friendly program to spread awareness for the patient as well as healthcare providers to get confidence and bring the actual demographic picture of the region.
Conflict Of Interest: Author declares that they have no conflict of interest.
References
- Agarwal A, Mulgund A, Hamada A, Chyatte MR (2015) A unique view on male infertility around the globe. Reproductive Biology and Endocrinology. 13(1): 37.
- Muthusami KR, Chinnaswamy P (2005) Effect of chronic alcoholism on male fertility hormones and semen quality. Fertil Steril. 84(4): 919–24.
- Ricci E, Viganò P, Cipriani S, Somigliana E, Chiaffarino F, et al. (2017) Coffee and caffeine intake and male infertility: a systematic review. Nutr J. 16(1): 37.
- Calderón B, Gómez‐Martín JM, Vega‐Piñero B, Martín‐Hidalgo A, Galindo J, et al. (2016) Prevalence of male secondary hypogonadism in moderate to severe obesity and its relationship with insulin resistance and excess body weight. Andrology. 4(1): 62–7.
- Dupont C, Faure C, Sermondade N, Boubaya M, Eustache F, et al. (2013) Obesity leads to higher risk of sperm DNA damage in infertile patients. Asian J Androl. 15(5): 622-5.
- Gabrielsen JS, Tanrikut C (2016) Chronic exposures and male fertility: the impacts of environment, diet, and drug use on spermatogenesis. Andrology. 4(4): 648–61.
- Richard S, Moslemi S, Sipahutar H, Benachour N, Seralini GE (2005) Differential effects of glyphosate and roundup on human placental cells and aromatase. Environ Health Perspect. 113(6): 716–20.
- Sudhakar DVS, Nizamuddin S, Manisha G, Devi JR, Gupta NJ, et al. (2018) NR5A1 mutations are not associated with male infertility in Indian men. Andrologia. 50(3): e12931.
- Krausz C, Escamilla AR, Chianese C (2015) Genetics of male infertility: from research to clinic. Reproduction. 150(5): R159– 74.
- Zare-Abdollahi D, Safari S, Mirfakhraie R, Movafagh A, Bastami M, et al. (2015) Mutational screening of the NR5A1 in azoospermia. Andrologia. 47(4): 395–401.
- Fan Y, Silber SJ (2019) Y chromosome infertility. GeneReviews®[Internet].
- Chen HG, Sun B, Chen YJ, Chavarro JE, Hu SH, et al. (2020) Sleep duration and quality in relation to semen quality in healthy men screened as potential sperm donors. Environ Int. 135: 105368.
- Lähdetie J (1995) Occupation-and exposure-related studies on human sperm. J Occup Environ Med. 37(8): 922-30.
- Auger J, Kunstmann JM, Czyglik F, Jouannet P (1995) Decline in Semen Quality among Fertile Men in Paris during the Past 20 Years. New England Journal of Medicine. 332(5): 281–5.
- Schwartz D, Mayaux MJ, Spira A, Moscato ML, Jouannet P, et al. (1983) Semen characteristics as a function of age in 833 fertile men. Fertil Steril. 39(4): 530–5.
- Henkel R, Bittner J, Weber R, Hüther F, Miska W (1999) Relevance of zinc in human sperm flagella and its relation to motility. Fertil Steril. 71(6): 1138–43.
- Rolf C, Behre HM, Nieschlag E (1996) Reproductive parameters of older compared to younger men of infertile couples. International Journal of Andrology. 19(3): 135–42.
- Andolz P, Bielsa MA, Vila J (1999) Evolution of semen quality in North-eastern Spain: a study in 22 759 infertile men over a 36 year period. Human Reproduction. 14(3): 731–5.
- Shivashankar R, Kondal D, Ali MK, Gupta R, Pradeepa R, et al. (2017) Associations of Sleep Duration and Disturbances With Hypertension in Metropolitan Cities of Delhi, Chennai, and Karachi in South Asia: Cross-Sectional Analysis of the CARRS Study. Sleep. 40(9): zsx119.
- Samal S, Dhadwe K, Gupta U, Gupta NK (2012) Epidemiological study of male infertility. Indian Medical Gazette. 5: 174–80.
- Bonde JP (1992) Semen quality in welders exposed to radiant heat. Occup Environ Med. 49(1): 5–10.
- Hamerezaee M, Dehghan SF, Golbabaei F, Fathi A, Barzegar L, et al. (2018) Assessment of Semen Quality among Workers Exposed to Heat Stress: A Cross-Sectional Study in a Steel Industry. Saf Health Work. 9(2): 232–235.
- Babar MS, Tazyeen S, Khan H, Tsagkaris C, Essar MY, et al. (2021) Impact of climate change on health in Karachi, Pakistan. The Journal of Climate Change and Health. 2: 100013.
- Samie A, Abbas A, Azeem MM, Hamid S, Iqbal MA, et al. (2020) Examining the impacts of future land use/land cover changes on climate in Punjab province, Pakistan: implications for environmental sustainability and economic growth. Environmental Science and Pollution Research. 27(20): 1-19.
- Kim KH, Kabir E, Ara Jahan S (2014) A Review of the Consequences of Global Climate Change on Human Health. Journal of Environmental Science and Health, Part C. 32(3): 299– 318.
- Kamran A, Dawood MA, Rafi SK, Butt FM, Akhtar K (2020) Impact of Brand Name on Purchase Intention: A Study on Clothing in Karachi, Pakistan. International Journal of Innovation, Creativity and Change. 14(11): 278-293.
- Sadeghi MR (2021) The Possibility of Increasing Oocyte Capacity to Repair Sperm DNA Fragmentation. J Reprod Infertil. 22(2): 75-76.
- Shefi S, Tarapore PE, Walsh TJ, Croughan M, Turek PJ (2007) Wet heat exposure: a potentially reversible cause of low semen quality in infertile men. International braz j urol. 33(1): 50–7.
- Memon M, Soomro MS, Akhtar MS, Memon KS (2011) Drinking water quality assessment in Southern Sindh (Pakistan). Environ Monit Assess. 177(1): 39–50.
- Ahsan U, Kamran Z, Raza I, Ahmad S, Babar W, et al. (2014) Role of selenium in male reproduction—A review. Anim Reprod Sci. 146(1-2): 55–62.
- Kapoor A, Tanjore S, Viraraghavan T (1995) Removal of selenium from water and wastewater. International Journal of Environmental Studies. 49(2): 137–147.
- Malhotra M, Pal M, Pal P (2020) A response surface optimized nanofiltration-based system for efficient removal of selenium from drinking Water. Journal of Water Process Engineering. 33: 101007.
- Rehman A, Jingdong L, Hussain I (2015) The province-wise literacy rate in Pakistan and its impact on the economy. Pacific Science Review B: Humanities and Social Sciences. 1(3): 140– 144.
- Ward DJ (2011) The role of education in the prevention and control of infection: A review of the literature. Nurse Educ Today. 31(1): 9–17.
- Schuppe HC, Pilatz A, Hossain H, Diemer T, Wagenlehner F, et al. (2017) Urogenital Infection as a Risk Factor for Male Infertility. Dtsch Arztebl Int. 114(19): 339–346.