Khatuna Lobjanidze MD, PhD*, Ulrich Wunderle MD, Beate Ruppert MD, Marc Mendler MD,PD.
University Hospital OWL Bielefeld University, Campus Klinikum Lippe, Department of Pediatric and Adolescent Medicine, Detmold, Germany
*Corresponding Author: Khatuna Lobjanidze MD, PhD, University Hospital OWL Bielefeld University, Campus Klinikum Lippe, Department of Pediatric and Adolescent Medicine, Detmold, Germany.
Abstract
Background: Erythema multiforme major in a child was associated with Mycoplasma pneumoniae as the suspected causal agent.
Case Presentation: An 11-year-old boy presented with a 4-day history of cough, fever up to 40°C and pharyngitis. On the day of admission, additionally, the patient experienced gingival bleeding and changes in the oral mucosa. Following treatment, with the antibiotic- and glucocorticoid-therapie led to recovery and the patient was discharged at home within 3 weeks.
Discussion: EMM as a cutaneous hypersensitivity reaction contemplate to be caused by the various viral or bacterial stimuli. Mycoplasma pneumoniae occurs to be one of them in the pediatric population.
Conclusion: Clinicians should be vigilant for the systemic symptoms, extensive mucosal involvement and tendency of recurrence, therefore, should ensure timely diagnosis and management.
Keywords: Erythema multiforme major, targetoid lesions, upper respiratory infection, Mycomplasma pneumoniae
Introduction
The development of Erythema Multiforme Major subsequent to Mycoplasma Pneumoniae infection is well established in the literature. Despite this, identifying the disease is still a challenge for clinicians and is often confused with Stevens-Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN). [1,2] Albeit no form of therapy is eminent as widely effective, the importance of additional case reports are essential for further characteristics of EMM and its management.
Herein, we presents case of a pronounced erythema multiforme major induced by mycoplasma pneumoniae in a pediatric age. The rashes on the skin and mucus layers developed 98 hours after the appearance of the common cold symptoms. Glucocorticoid- therapie led to the full recovery after 3 weeks without any further complications.
Case Report
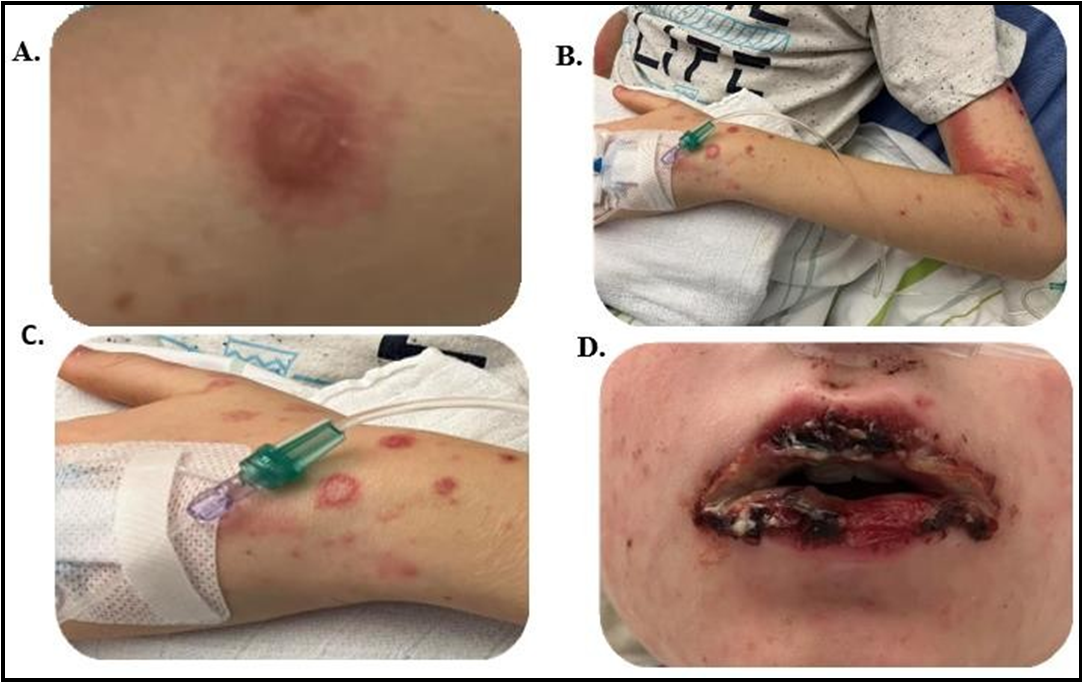
An ill-appearing, 11-year-old child with a 4-day history of a productive cough, fever and pharyngitis was admitted to our hospital, pediatric emergency room (ER) due to reduced oral intake. Physical examination revealed several pinkish-red target-like lesions over the trunk and upper extremities (Figure 1 B and C), hemorrhagic- exudative plaques on the lips (Figure 1D), gingival bleeding and changes in the oral mucosa. SJS and staphylococcal scalded skin syndrome was excluded with the negative Nikolsky sign. [3-5]
Clinical features, such as cervical lymphadenitis, strawberry tongue or desquamating perineal exanthema was not detected. [6,7] Relevant previous illnesses including herpes simplex virus infections and the intake of suspected drugs causing erythema, such as NSAID’S, certain antibiotics, and anticonvulsants was denied. [8]
In the personal history, five weeks ago, the patient was infected with the contagious hand-mouth-foot disease, which caused fever, sore throat, reduced appetite, and small spots on the mucous membranes in the mouth. [9] The symptoms resolved within a few days without complications.
The overall presentation was accord with EMM. Chest x-ray demonstrated a viral pneumoniae without focal consolidation. Laboratory analysis revealed leukocytosis with significantly elevated C-reactive protein. Serologically were excluded the infections and possible causes of EMM, such as herpes simplex virus (HSV)-1, HSV-2, parvovirus B19, cytomegalievirus (CMV)and Epstein-Barr virus (EBV). The elevated antibodies, in particular, immunoglobulin A (IgA) and IgG against Mycoplasma pneumoniae, led us to the final diagnosis, namely EMM as a secondary disease developing after a primary Mycoplasma pneumoniae infection.
Treatment was started with Antibiotic, namely Clarythromycin and subsequently, due to the substantial mucosal involvement and persisted mucosal ulceration Prednisolone and an adhesive ointment containing glucocorticoids was used. Under these therapeutic measures, lesions together with other symptoms, productive cough, malaise, reduced oral intake showed regression and the patient was discharged at home.
Figure 1: (A) Initially, target-like, round, papulo-urticarial plaques with a livid center, a lighter intermediate zone and a dark red border. (B and C) several pinkish-red, eroded lesions on theupper extremities. (D) Hemorrhagic-crusted lesions, plaques on the labium superius oris und labium inferius oris.
Discussion
EMM is an acute inflammatory reaction following viral infections or drug intake that affects skin and mucosal surfaces. [10,11] It comprises symmetrically distributed polymorphous eruption of maculopapular skin efflorescence and target-like lesions, less than 3 cm in size and bubble formation in the center. The lesions group over the distal extremities and trunk and commonly appear 3–14 days after exposure. [12,13] Mycoplasma pneumoniae, a bacterium, which is known to elicit the pulmonary and extra-pulmonary complications, is a frequent cause of EMM within the pediatric population. [14-15] Studies related to the diagnosis and treatment of EMM, use of systemic steroids remains controversial, hence the consultation with a dermatologist for the treatment and desired outcome is consequential. [19]
Accordingly, the initial stage of the disease are generally treated symptomatically, supportive therapy is mostly based on the history and examination. During severe cases, when oral mucous membranes are involved, to suppress the cytokine and chemokine response and correspondingly decrease the inflammatory reactions, an adjuvant therapy with steroids are conceivable.[16-18]
Footnotes
Informed Consent: written informed consent was obtained from the patient for publication of this case report and images.
Conflict of Interest Statement:
The authors have no conflicts of interest to declare.
Author Contributions:
Authors declare that they have all participated in the design, execution, analysis and the approval of the final version of the paper.
References
- Canavan TN, Mathes EF, Frieden I, Shinkai K (2015) Mycoplasma pneumoniae-induced rash and mucositis as a syndrome distinct from Stevens-Johnson syndrome and erythema multiforme: a systematic review. J Am Acad Dermatol. 72(2): 239-45.
- Chen N, Li M (2022) Case Report and Literature Review: Clinical Characteristics of 10 Children With Mycoplasma pneumoniae-Induced Rash and Mucositis. Front Pediatr. 10: 823376.
- Maity S, Banerjee I, Sinha R, Jha H, Ghosh P, et al. (2020) Nikolsky's sign: A pathognomic boon. J Family Med Prim Care. 9(2):526-530.
- Eginli A, Shah K, Watkins C, Krishnaswamy G (2017) Stevens- Johnson syndrome and toxic epidermal necrolysis. Ann Allergy Asthma Immunol. 118(2): 143-147.
- Grunwald MH, Ginzburg A, David M, Feuerman EJ (1984) Nikolsky's or Pseudo-Nikolsky's sign in bullous pemphigoid. Int J Dermatol. 23(9): 629.
- Patrizi A, Raone B, Savoia F, Ricci G, Neri I (2008) Recurrent Toxin-Mediated Perineal Erythema: Eleven Pediatric Cases. Arch Dermatol. 144(2): 239–243.
- Isidori C, Sebastiani L, Cardellini MC, Di Cara G, Rigante D, et al. (2017) Early Desquamating Perineal Erythema in a Febrile Infant: A Characteristic Clinical Featureof Kawasaki Disease. Int J Environ Res Public Health. 14(7): 710.
- Aswath N, Rakshana R (2022) Drug induced erythema multiforme of the oral cavity. Arch ClinCases. 9(4): 157-160.
- Zhu P, Ji W, Li D, Li Z, Chen Y, et al. (2023) Current status of hand-foot-and-mouth disease. J Biomed Sci. 30(1): 15.
- Lerch M, Mainetti C, Terziroli Beretta-Piccoli B, Harr T (2018) Current Perspectives on Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Clin Rev Allergy Immunol. 54(1): 147- 176.
- Lamoreux MR, Sternbach MR, Hsu WT (2006) Erythema multiforme. Am Fam Physician. 74(11): 1883-8.
- Trayes KP, Love G, Studdiford JS (2019) Erythema Multiforme: Recognition and Management. Am Fam Physician. 100(2): 82-88.
- Bau JT, Cooper CL (2019) Erythema multiforme major associated with Mycoplasma pneumoniae infection. CMAJ. 191(43): E1195.
- Auquier-Dunant A, Mockenhaupt M, Naldi L, Correia O, Schröder W, et al. (2002) Correlations between clinical patterns and causes of erythema multiforme majus, Stevens-Johnson syndrome, and toxic epidermal necrolysis: results of an international prospective study.Arch Dermatol. 138(8): 1019- 24.
- Vujic I, Shroff A, Grzelka M, Posch C, Monshi B, et al. (2015) Mycoplasma pneumoniae-associated mucositis--case report and systematic review of literature. J Eur Acad Dermatol Venereol. 29(3): 595-8.
- Riley M, Jenner R (2008) Towards evidence based emergency medicine: best BETs from theManchester Royal Infirmary. Bet 2. Steroids in children with erythema multiforme. Emerg Med J. 25(9): 594-5.
- Chan M, Goldman RD (2013) Erythema multiforme in children: the steroid debate. Can Fam Physician. 59(6): 635-6.
- Michaels B (2009) The role of systemic corticosteroid therapy in erythema multiforme major and stevens-johnson syndrome: a review of past and current opinions. J Clin Aesthet Dermatol. 2(3): 51-5.
- Siedner-Weintraub Y, Gross I, David A, Reif S, Molho-Pessach V (2016) Paediatric Erythema Multiforme: Epidemiological, Clinical and Laboratory Characteristics. Acta Dermato- Venereologica, 97(4): 489–492.