Allison Gerrard OMS IV1*, Rollin J. Hawley M.D2
1Edward Via College of Osteopathic Medicine in Blacksburg, VA, USA
2Neurology Consultant, Carilion New River Valley Medical Center in Christiansburg, VA, USA
*Corresponding Author: Allison Gerrard OMS IV, Edward Via College of Osteopathic Medicine in Blacksburg, VA, USA
Abstract
We present the case of a 55-year-old male with a history of chronic alcohol abuse leading to multiple complications, including hypokalemia with evidence of electrocardiogram (EKG) changes, cognitive decline, macrocytic anemia, alcoholic nutritional peripheral polyneuropathy, and cerebellar degeneration. Our case report follows the patient through an emergency department visit prompted by weakness leading to a 26-day hospitalization, followed by a neurology consultation after discharge from rehabilitation through a skilled nursing facility. This case report outlines multiple complications of chronic alcohol use and their potential short- and long-term effects.
Introduction
Alcohol abuse is a common problem in the United States, and it is defined as a pattern of consuming alcohol that interferes with typical daily activities. Alcohol abuse affects 17% of adults at some point within their lifetime, with 12.5 % being alcohol dependent [1]. Heavy alcohol consumption can be defined as consuming more than four drinks a day for men or more than three drinks a day for women [2]. Chronic, heavy alcohol consumption can have dangerous consequences that negatively impact a person’s health. These consequences include, but are not limited to, electrolyte abnormalities, Wernicke-Korsakoff syndrome, hemodynamic disturbances including anemias, cerebellar degeneration, nutritional peripheral polyneuropathy, and liver disease.
Electrolyte abnormalities are common among malnourished alcoholic patients and generally worse in patients with protein-calorie or vitamin deficiencies [3]. Common electrolyte disturbances due to alcohol use include hypokalemia and hyponatremia.
Hypokalemia generally occurs due to decreased intake and increased excretion, usually through diarrhea [3]. Hypokalemia can lead to serious cardiac arrhythmias and severe myopathy, leading to muscle weakness [3]. The treatment for hypokalemia is potassium replacement and frequent electrolyte reassessment. Hyponatremia is common in patients with alcohol-induced cirrhosis due to water ingestion in vasopressin-induced renal impairment, causing decreased free water clearance [4]. Because of this faulty mechanism, the initial treatment for hyponatremia is simply water restriction [4]. Hypertonic saline could be administered in severe cases, but rapid correction of hyponatremia can lead to severe complications, including central pontine myelinolysis [5].
The Wernicke-Korsakoff syndrome is another potential severe consequence of chronic alcohol consumption. The Wernicke-Korsakoff syndrome is due to a nutritional deficiency of thiamine or vitamin B1 [6]. Treatment focuses on thiamine replacement, and some studies have investigated using thiamine for prevention in at- risk patients [7]. While the two are often combined into one syndrome, Wernicke’s Encephalopathy and Korsakoff syndrome have different symptoms. Wernicke’s involves three main symptoms: ocular abnormalities (including nystagmus, weakness, and ophthalmoplegia), ataxia, and decreased consciousness or mental disturbances [8]. Wernicke’s Encephalopathy can be diagnosed on brain magnetic resonance imaging (MRI) because the MRI will often show atrophy of the mamillary bodies [9]. Korsakoff syndrome is characterized by a memory gap with anterograde or retrograde amnesia, and confabulation is sometimes evident [8].
Cerebellar degeneration is a common complication of heavy alcohol use and could affect up to 66 % of chronic alcoholics [10]. This cerebellar degeneration typically affects the patient’s gait and stance while sparing the upper limbs and speech [11]. A clinical neurological examination is necessary to diagnose cerebellar degeneration, and there could be some benefits in performing computerized tomography (CT) of the brain for diagnosis assistance [12]. Current treatment recommendations include thiamine, cessation of alcohol consumption, and symptom management with medications.
Chronic alcohol use can also lead to hematologic disturbances, including anemia. In one study, 75 % of the people admitted for alcoholism had a red blood cell production disorder, with 40 % having megaloblastic anemia [13]. The megaloblastic anemia was due to folate deficiency in this study population [13]. Another study found that macrocytosis often persisted in alcoholic patients even after folate supplementation, suggesting that alcohol directly affects the development of erythrocytes [14].
Nutritional peripheral polyneuropathy is another complication of alcoholism. This type of peripheral polyneuropathy typically develops in malnourished patients who consume most of their calories from alcohol. Nutritional deficiency and the direct toxic effect of alcohol on peripheral nerves have been believed to lead to peripheral polyneuropathy in alcoholic patients [15]. The neuropathy begins with symmetric sensory symptoms and eventually involves more proximal and motor nerves [16]. As the disease progresses, it is associated with severe slowing nerve conduction velocities [16]. While the damage generally cannot be completely reversed, treatment consists of symptom management and stopping the progression of the disease through abstaining from alcohol use and beginning a nutritious diet with B vitamin supplementation [15].
Liver injury is another common effect of long-term alcohol use. Liver steatosis, or fatty liver, is the first sign of liver injury in an alcoholic patient [17]. The second stage of liver injury is fibrosis, which can lead to alcoholic hepatitis [17]. The final step is cirrhosis and end- stage liver disease [17]. Clinical signs of cirrhosis include symptoms of portal hypertension, such as esophageal varices, bacterial peritonitis, hepatic Encephalopathy, and ascites [18]. Paracentesis can provide symptomatic relief from large-volume ascites. Management of alcoholic liver disease includes cessation of drinking alcohol and liver transplantation [19].
Medication therapies have been explored, but currently, there are no medications that have shown long-term improvements in alcoholic cirrhosis [19].
During hospitalizations, patients with a recent history of chronic, heavy alcohol consumption should be monitored for withdrawal. Because alcohol is a depressant, when alcohol is abruptly reduced or stopped, brain hyperexcitability can develop and cause alcohol withdrawal syndrome [20]. Initial symptoms are minor and can include insomnia, tremors, anxiety, headache, diaphoresis, and decreased appetite [20]. More severe symptoms develop next, consisting of hallucinations and tonic-clonic seizures, and patients can ultimately create a syndrome called delirium tremens [20]. Hospitals utilize the Clinical Institute Withdrawal Assessment for Alcohol to assess a patient’s risk of developing alcohol withdrawal syndrome [20]. If indicated, patients can receive benzodiazepines to reduce their risk of withdrawal complications during hepatization [20]. The Clinical Institute Withdrawal Assessment for Alcohol should be used for every patient with the potential for alcohol withdrawal.
Case Description
A 55-year-old male presented to the emergency department with weakness in his lower extremities that had worsened over the past week. His family was concerned because he needed to lean on walls to ambulate for the past several days, and he reported frequent falls. He had a history of tobacco and alcohol use, and he admitted drinking both liquor and beer daily.
A review of systems was only positive for weakness in his legs, and his vital signs were interpreted as normotensive, not tachycardic, afebrile, not tachypneic, and not hypoxic upon arrival. His lower extremities showed antigravity strength on physical exam, and the patient was ataxic. Initial labs included a complete blood count showing a hemoglobin of 9.3 g/dL (13.0-16.0 g/dL), hematocrit of 26.6 % (37-49 %), mean corpuscular volume 127.9 fL (78-98 fL), mean corpuscular hemoglobin of 44.7 pg (27-34.6 pg) and red cell distribution width of 15.4 % (11.5- 14.5 %). A comprehensive metabolic panel showed sodium 131 mmol/L (135-145 mmol/L), potassium 2.0 mmol/L (3.5-5.3 mmol/L), chloride 79 mmol/L (95- 107 mmol/L), glucose 147mg/dL (70-99 mg/dL), total bilirubin 1.5 mg/dL (<1.3 mg/dL), alkaline phosphatase 206 IU/L (42-121 IU/L), AST 108 IU/L (10-42 IU/L), anion gap 27 mmol/L (8-18 mmol/L). His ammonia level was normal at 27U mol/L (11-51U mol/L). An EKG showed normal sinus rhythm with a normal axis, prolonged QTC, and a Q-wave consistent with hypokalemia. He was treated with potassium and admitted to the hospital for further medical management.
The patient was hospitalized for 26 days. During his hospital stay, he was treated for alcohol abuse and withdrawal, subacute ataxia, cognitive decline, possible chronic obstructive pulmonary disease, moderate protein-calorie deficiency malnutrition, oropharyngeal dysphagia, and anemia. Relevant consultations included tele- neurology, psychiatry, and physiatry. Follow-up labs revealed worsening anemia that eventually required a blood transfusion during his hospitalization, and fecal blood testing was negative. There was initial concern for Wernicke- Korsakoff syndrome due to his cognitive deficits, ataxia, and ambulatory dysfunction, so the patient was started on thiamine. Physical and occupational therapy worked with the patient to improve mobile function, and he did make some improvements during his hospitalization.
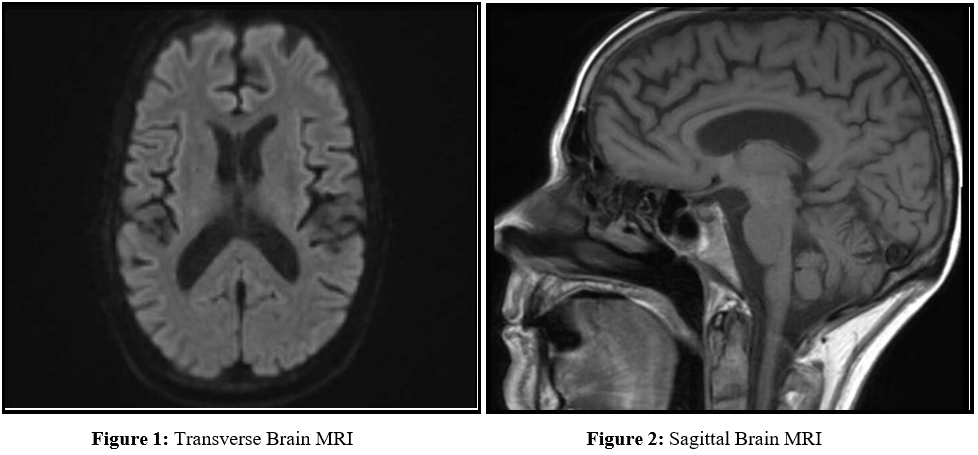
Psychiatry suggested treatment with Aricept and Namenda for his probable dementia and determined the patient also needed gabapentin for an additional painful peripheral neuropathy diagnosis, likely due to alcohol use. Relevant imaging included a right upper quadrant ultrasound that showed hepatic steatosis and a brain MRI that revealed mild generalized atrophy (Figures 1 and 2). The MRI showed no abnormalities within the mammillary bodies. His hyponatremia and hypokalemia were treated and resolved. Near the end of his hospitalization, physiatry determined the patient was an appropriate candidate for rehabilitation placement. The patient was ultimately discharged to a skilled nursing facility for rehabilitation.
About a year after his hospitalization, the patient presented for an outpatient neurology consultation. Relevant history included that he could no longer work due to decreased fine motor skills. He reported drinking a quart of rum every day since he was 21 but recently reduced his alcohol intake, saying his last drink was 3 months prior. Their family history included alcoholism in his maternal grandfather. He remained on multiple medications from his hospitalization. On physical exam, the patient was chronically ill-appearing, had an unbalanced and unsteady gait due to ataxia, wide-based stance, truncal titubation when he stood, numbness from his fingertips to elbows and toes to his hips, decreased sense of touch in stocking-glove distribution, unable to stand on his toes, heels, or perform tandem gait, areflexic, heel to shin ataxia bilaterally, did not have a finger to nose ataxia or nystagmus. He did have some orthostatic hypotension upon standing. The patient was mentally intact – he was fully oriented to time and place, able to perform serial subtractions, and could recall 3 items after 5 minutes, although he was a conspiracy theorist with some paranoid traits. The patient was ultimately diagnosed with alcoholic nutritional peripheral polyneuropathy and cerebellar degeneration. He was counseled on continued alcohol cessation, medication adherence, contacting Alcoholics Anonymous, and increasing his current dose of escitalopram to improve his depression.
Discussion
This case is unique because it follows a patient through multiple phases and complications of chronic alcohol abuse over a year. It follows him through an emergency department visit leading to a lengthy hospitalization and outpatient follow-up months after his rehabilitation and skilled nursing facility stay. The case shows acute and chronic problems and the effects of medical treatment and rehabilitation on these issues.
The patient’s diagnosis of chronic alcoholic nutritional peripheral polyneuropathy was determined due to his sensory loss in a stocking-glove distribution, and he reported numbness from his fingertips to elbows and toes to his hips. He was showing signs of this during his Hospitalization, where he was prescribed gabapentin for symptom management, and during his outpatient neurology consult. Because his symptoms were symmetric and primarily sensory, we can conclude that his peripheral polyneuropathy is in the beginning stages of the disease [16].
He also was diagnosed with cerebellar degeneration due to his ataxia and ambulatory dysfunction. The patient’s presentation followed the typical symptoms of alcoholic cerebellar degeneration: his gait, stance, and lower extremities were affected, but he was still able to use his upper extremities usually [11]. During his outpatient neurology follow-up appointment, he could ambulate, using a walking stick for assistance. If the patient continues to use alcohol, we expect this condition to worsen. The patient did not have a CT scan, which could have aided the diagnosis, but it is ultimately unnecessary as a thorough clinical neurological exam is sufficient [12].
When the patient arrived at the emergency department, he was severely hypokalemic.
His hypokalemia led to EKG changes and a prolonged QTC interval. Without treatment and potassium supplementation, the patient was at risk of dangerous cardiac arrhythmias [3]. Because his hypokalemia was so severe, the patient was also at risk for an acute myopathy, although we do not believe he experienced this complication [3]. His hypokalemia resolved with potassium supplementation and electrolyte reassessment, as expected.
While the patient did show evidence of cognitive decline during his hospitalization, he was mentally intact by his outpatient neurology follow-up appointment. His brain MRI during hospitalization also did not show proof of Wernicke-Korsakoff syndrome, as his mammillary bodies showed no acute or chronic changes [9]. MRI has a specificity of 93% in diagnosing Wernicke-Korsakoff syndrome, indicating that this form of imaging can accurately rule out the disease [21]. At the time of the neurology consultation, his previous imaging and cognitive state would exclude Wernicke-Korsakoff from the diagnosis. The patient possibly had an acute episode of Wernicke’s Encephalopathy during his hospitalization that was reversed with thiamine replacement.
This patient also showed early liver damage, as seen on his right upper quadrant ultrasound. His liver injury, steatosis, is in the initial stage of alcoholic liver disease [17]. If he continues to consume alcohol, he is at risk of developing fibrosis and cirrhosis.
Cirrhosis can lead to multiple dangerous complications due to chronic portal hypertension [18]. The patient should be monitored for progressive liver disease and complications, including esophageal varices, hepatic encephalopathy, and ascites [18].
During his hospitalization, the patient was at risk for alcohol withdrawal, so he took certain precautions to avoid potentially serious complications. The Clinical Institute Withdrawal Assessment for Alcohol was used to assess his risk of developing alcohol withdrawal syndrome. The protocol was followed and successfully treated his withdrawal symptoms, and he did not establish life-threatening withdrawal symptoms while hospitalized. The presented patient shows multiple complications and consequences of chronic alcohol consumption. These complications are followed for over a year, beginning with a hospitalization. This case is beneficial to review because it shows the progression of these complications and patient follow-up.
Conclusion
Chronic, excessive alcohol use can lead to multiple complications, including severe electrolyte abnormalities, cognitive deficiencies, Wernicke-Korsakoff syndrome, hemodynamic disturbances, cerebellar degeneration, and nutritional polyneuropathy. These consequences of consuming alcohol can be dangerous and significantly decrease a patient’s quality of life. We discussed the case of a 55-year-old alcoholic male with multiple complications from his alcohol use, and we followed him through an emergency department visit leading to hospitalization and a follow-up outpatient neurology consultation. This case is beneficial and unique because it follows a patient through multiple stages of alcoholism over a year, including his response to hospitalization and treatment.
Financial Disclosures: None Reported
Author Contributions:
Allison Gerrard drafted the article and provided contributions to the case report. Dr. Rollin J Hawley M.D. provided revision and evaluation of the case report.
References
- Schwartz JM, Reinus JF (2012) Prevalence and Natural History of Alcoholic Liver Disease. Clinics in Liver Disease. 16(4): 659– 666.
- Drinking Levels Defined | National Institute on Alcohol Abuse and Alcoholism (NIAAA).
- Palmer BF, Clegg DJ (2017) Electrolyte Disturbances in Patients with Chronic Alcohol-Use Disorder. New England Journal of Medicine. 377(14): 1368–1377.
- Pitts TO, van Thiel DH (1986) Disorders of the serum electrolytes, acid-base balance, andrenal function in alcoholism. Recent Dev Alcohol. 4: 311–339.
- Laureno R (1983) Central Pontine Myelinolysis Following Rapid Correction of Hyponatremia. Ann Neurol. 13(3): 232-42.
- Victor M (1990) Commentary MR in the Diagnosis of Wernicke- Korsakoff Syndrome. AJNR. 11: 895-896.
- Cook CCH (2000) Prevention and Treatment of Wernicke- Korsakoff Syndrome.Alcohol & Alcoholism. 35(Supplement_1): 19–20.
- Zubaran C, Ferandes JG, Rodnight R (1997) Eponyms in medicine revisited Wernicke-Korsakoff syndrome. Postgrad MedJ. 73: 27–31.
- Charness ME, DeLaPaz RL (1987) Mamillary body atrophy in Wernicke’s encephalopathy: Antemortem identification using magnetic resonance imaging. Annals of Neurology. 22(5): 595– 600.
- Fitzpatrick LE, Jackson M, Crowe SF (2012) Characterization of Cerebellar Ataxia in Chronic Alcoholics Using the International Cooperative Ataxia Rating Scale (ICARS). Alcoholism:Clinical and Experimental Research. 36(11): 1942–1951.
- Allsop J, Turner B (1966) Cerebellar degeneration associated with chronic alcoholism.Journal of the Neurological Sciences. 3(3): 238–258.
- Hillbom M, Muuronen A, Holm L, Hindmarsh T (1986) The clinical versus radiological diagnosis of alcoholic cerebellar degeneration. Journal of the Neurological Sciences. 73(1): 45–53.
- Eichner ER, Hillman RS (1971) The evolution of anemia in alcoholic patients. The American Journal of Medicine. 50(2): 218–232.
- Chanarin AWI, Levi AJ (1974) MACROCYTOSIS OF CHRONIC ALCOHOLISM. The Lancet. 303(7862): 829–831.
- Chopra K, Tiwari V (2012) Alcoholic neuropathy: possible mechanisms and futuretreatment possibilities. British Journal of Clinical Pharmacology. 73(3): 348–362.
- Hawley RJ, Kurtzke JF, Armbrustmacher VW, Saini N, Manz H (1982) The course ofalcoholic-nutritional peripheral neuropathy. Acta Neurologica Scandinavica. 66(5): 582–589.
- LIeber CS (1995) Medical Disorders of Alcoholism. 333(16): 1058–1065.
- Schuppan D, Afdhal NH (2008) Liver cirrhosis. The Lancet. 371(9615): 838–851.
- Tome S, Lucey MR (2004) Current management of alcoholic liver disease. AlimentaryPharmacology & Therapeutics. 19(7): 707– 714.
- Puz CA, Stokes SJ (2005) Alcohol Withdrawal Syndrome: Assessment and Treatment withthe Use of the Clinical Institute Withdrawal Assessment for Alcohol-Revised. Critical Care Nursing Clinics. 17(3): 297–304.
- Sullivan EV, Pfefferbaum A (2009) Neuroimaging of the Wernicke–Korsakoff Syndrome. Alcohol and Alcoholism. 44(2): 155–165.