Milos Jovanovic, DOa, Iva Minga, MDb, Mrinali Shetty, MDb, Jason C. Robin, MDb*
aDepartment of Medicine, NorthShore University Health System Evanston Hospital, Evanston, Illinois, USA
bSection of Cardiology, Department of Medicine, NorthShore University Health System Evanston Hospital, Evanston, Illinois, USA
*Corresponding Author: Jason Robin, MD, North Shore University Health System, 2150 Pfingsten Ave Suite 1200, Glenview, IL 60025.
Introduction
Azacitidine is a nucleoside metabolic inhibitor used to treat myelodysplastic syndrome (MDS) [1]. Azacitidine is a pyrimidine analog of the nucleoside cytidine [1]. It reversibly inhibits the enzymes DNA and RNA methyltransferase and subsequently blocks DNA and RNA methylation [1]. After this action, DNA and RNA are relatively hypomethylated. Thus, tumor suppressor genes previously silenced from hypermethylation are now active and expressed. Azacitidine is primarily associated with the adverse effects of neutropenia, thrombocytopenia, anemia, fever, asthenia, diarrhea, and ecchymosis. Chest pain was noted in 16 % of patients treated with Azacitidine (n=220) [2]. However, this chest pain's exact mechanism of action remains to be elucidated. Apart from chest pain, other cardiac-associated adverse effects of the drug include heart failure and pericardial effusion [2].
Fluorouracil (FU) is also a pyrimidine analog of the nucleotide uracil [3]. Specifically, it is fluoropyrimidine [3]. An active metabolite of FU, F-dUMP, inhibits the enzyme thymidylate synthetase, halting DNA synthesis and resulting in antineoplastic properties [3]. FU - and its prodrug Capecitabine - is associated with the cardiovascular side effects of angina pectoris, myocardial infarction, and vasospasm [3]. The mechanism of action of cardiac toxicity is believed to be related to endothelial dysfunction leading to coronary vasospasm [3].
Below, we present a novel case of a 63-year-old male with high-risk MDS progressing to acute myeloid leukemia (AML) on active treatment with Azacitidine who presents with angina. This is the first reported case of pretreatment with vasodilators for managing Azacitidine-associated chest pain.
Case Report
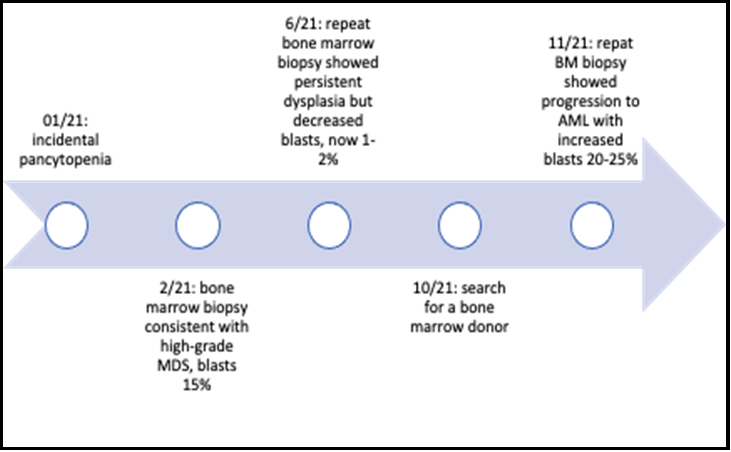
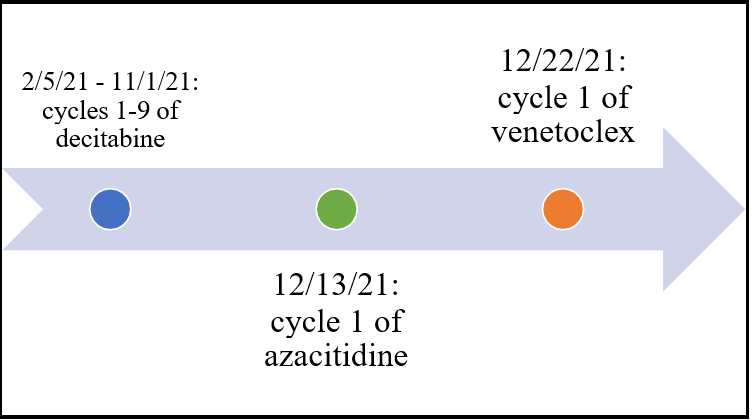
A 63-year-old male with a past medical history of coronary artery disease (CAD) previously treated with multiple stents on dual antiplatelet therapy (DAPT) and high-grade MDS with evolution to AML on active chemotherapy treatment with Azacitidine presented with angina. He was initially found to have pancytopenia in January of 2021 during an admission for a non-ST elevation myocardial infarction (NSTEMI). His peripheral smear was notable for promyelocytes and metamyelocytes. Subsequent bone marrow biopsy showed markedly abnormal megakaryocytes and increased blasts to 15 %, consistent with high-grade MDS. Flow cytometry showed 14 % myeloblasts. Next-generation sequencing showed a P53 mutation. He started cycle 1 of decitabine 20mg/m2. Venetoclex was held due to pancytopenia. After four cycles of decitabine, a second bone marrow biopsy was obtained. This biopsy showed persistent dysplasia but decreased blasts of 1-2 %. He was referred for a bone marrow transplant. Cycle 9 was completed in November 2021, and a third bone marrow biopsy was obtained. This biopsy showed progression to AML with increased blasts to 20-25 %. Decitabine was stopped after 9 completed cycles. He was subsequently started on Azacitidine. He tolerated the first two treatments of Azacitidine without any significant side effects. He developed chest pain the evening after his third day of treatment.
The patient was sitting on the couch when the chest pain began. He described his symptoms as pressure in the center of his chest, with mild shortness of breath but without radiation or positional change. He denied any associated lightheadedness, dizziness, loss of consciousness, palpitations, or nausea. He stated that the chest pressure felt precisely like the one in April, resulting in a stent. He took one sublingual nitroglycerine with complete resolution of the pain but started developing symptoms again within 24 hours and was instructed to go to the emergency department for further evaluation. On admission, his vitals were BP 106/62, HR 78, RR 16, temp 98.2F, and SpO2 100 % (on room air). Physical examination was unrevealing and did not demonstrate reproducibility of the chest pain upon palpation. The initial basic metabolic panel (BMP) was unremarkable. Complete blood count (CBC) showed known pancytopenia (white blood cells 0.8k, hemoglobin 9.5 and platelets 26k). An electrocardiogram (ECG) showed normal sinus rhythm without ST or T wave changes. However, he was asymptomatic by this time. High sensitivity troponin was negative 8 (ng/L) then 8 (ng/L), checked 2 hours apart. Computed tomography with pulmonary embolism protocol (CT PE) did not demonstrate evidence of PE. Transthoracic echocardiogram (TTE) did not show evidence of pericardial effusion or wall motion abnormality. The Cardiology and Oncology services were consulted. Given the progression of disease burden while on treatment with decitabine, the benefits of continuing Azacitidine outweighed the risks.
Azacitidine is a pyrimidine, similar to another nucleoside analog, FU, which is a fluoropyrimidine. We hypothesized that the mechanism of chest pain is probably similar for both drugs [1,3]. Padegimas and Carver have proposed an algorithm of treatment for patients who developed coronary vasospasm while getting FU. We applied the same algorithm in this clinical scenario to allow for continued life-prolonging treatment with Azacitidine [4,5]. The patient was treated with oral diltiazem sustained release 120mg and isosorbide mononitrate 30mg on chemotherapy days. Day 5 and Day 6 of Azacitidine were administered while he was hospitalized. For both days, he was pre-treated with the above regimen and tolerated the treatment well and without recurrence of chest pain. He continued chemotherapy treatment as an outpatient with the same pretreatment medications and tolerated subsequent treatments without recurrence of his angina.
Figure 1: [Timeline of Disease Progression. A period of 10 months elapsed from the time of diagnosis to a third bone marrow biopsy despite active treatment.]
Figure 2: [Timeline of Chemotherapy. Nine cycles of decitabine were completed prior to starting Azacitidine and ultimately, venetoclex.]
Discussion
We present a case of a 63-year-old male with high-risk MDS and subsequent progression to AML on active treatment with Azacitidine who presents with angina.
FU is the third most commonly prescribed chemotherapeutic agent worldwide for solid tumor malignancies [3] After anthracyclines, FU is the second most common chemotherapy that can lead to cardiac toxicity [3]. When cardiac toxicity occurred with FU, 69 % of cases experienced symptoms in the first 72 hours of initial infusion, with the most common symptom being angina [3]. The mechanism of cardiac toxicity has not yet been elucidated; however, it is believed to be multifactorial and is most likely related to coronary vasospasm [3]. The coronary vasospasm is believed to occur secondary to active FU metabolites that result in dysfunction of the endothelium that increase the release of the vasoconstrictor endothelin-1 and decrease the release of the vasodilator prostacyclin [3,4]. Coronary vasospasm has been demonstrated in patients using coronary angiography [3]. Since vasospastic angina is treated with calcium channel blockers and long- acting nitrates - and given that there is no significant drug interaction between Azacitidine and the two vasodilators - the decision was made to use them as pretreatment on chemotherapy days [4,6]. Given the pretreatment regimen, the patient could successfully tolerate and complete the remainder of his cycle 1 treatment with Azacitidine. In summary, our case report presents a patient who was pre-treated with vasodilators on chemotherapy days, so the adverse effect of Azacitidine-induced angina was not experienced.
Conclusion
Azacitidine-related chest pain is a significant side effect that can limit ongoing chemotherapy treatment with this agent. We hypothesize that the mechanism of action of Azacitidine-related chest pain is similar to FU-related chest pain leading to coronary vasospasm. Treatment with agents that target coronary vasospasm can lead to resolution of chest pain and tolerance of further chemotherapy treatments. Given that chest pain has been observed in 16% of patients on therapy with Azacitidine, our case highlights the need for other studies to evaluate the pathophysiology and efficacy of coronary vasodilators for its treatment [2].
Declarations
Ethical approval: This is a case report and not a research study. IRB approval was not obtained.
Consent for publication: Written informed permission was obtained from the patient to publish this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of data and material: N/A
Competing interests: No one
Funding: None
Author contributions: MJ: responsible for writing and editing the manuscript. IM and MS: responsible for writing parts of the manuscript and reviewing; JR: responsible for reviewing and editing the manuscript.
Acknowledgments: None
Funding Support and Author Disclosures: The authors have reported that they have no relationships relevant to the contents of the paper to disclose.
Abbreviations and Acronyms:
AML acute myeloid leukemia BMP basic metabolic panel
CAD coronary artery disease CBC complete blood count
CT PE computed tomography with pulmonary embolism protocol
DAPT dual antiplatelet therapy
DES drug-eluding stent ECG electrocardiogram FU fluorouracil
MDS myelodysplastic syndrome
NSTEMI non-ST elevation myocardial infarction
RCA right coronary artery
TTE transthoracic echocardiogram
References
- Yang Y, Li J, Geng Y, Liu L, Li D (2021) Azacitidine regulates DNA methylation of GADD45γ in myelodysplastic syndromes. J Clin Lab Anal. 35(2): e23597.
- Highlights of Prescribing Information. Bristol Myers Squibb, Mar. 2020.
- Zafar A, Drobni ZD, Mosarla R, Alvi RM, Lei M, et al. (2021) The Incidence, Risk Factors, and Outcomes With 5-Fluorouracil- Associated Coronary Vasospasm. JACC CardioOncol. 3(1):101- 109.
- Padegimas A, Carver JR (2020) How to Diagnose and Manage Patients With Fluoropyrimidine-Induced Chest Pain: A Single Center Approach. JACC CardioOncol. 2(4): 650-654.
- Sheth MA, Widmer RJ, Dandapantula HK (2021) Pathobiology and evolving therapies of coronary artery vasospasm. Proc (Bayl Univ Med Cent). 34(3): 352-360.
- Ambrosy AP, Kunz PL, Fisher GA, Witteles RM (2012) Capecitabine-induced chest pain relieved by diltiazem. Am J Cardiol. 110(11): 1623-6.