Steven P. Petrosino, Ph.D. *, Arthur Armstrong, MD, Ph.D., Angela Johnson, RN, MPH, Boaz Nyona Matende, MSci
Clinical Scientist and President, Nutrition Advisor LLC, 8815 Tayport Drive, Dublin OH 43017, USA
*Corresponding Author: Steven P. Petrosino, Ph.D., Clinical Scientist and President, Nutrition Advisor LLC, 8815 Tayport Drive, Dublin OH 43017, USA
Abstract
Purpose: The purpose of the review was to explore whether the disease severity, oxidative stress, and hyper-inflammatory induction in SARS-CoV-2 infection can be used as a basis for dietary, pharmacologic, and herbal intervention in the prevention, management, and treatment of COVID-19.
Background: Coronavirus disease 2019 (COVID-19) began as a cluster of pneumonia cases reported in the Wuhan region of China in late 2019. The new disease spread to all parts of the world in a few months and as of August 2020, COVID-19 is fully established as a global pandemic and the search for urgent and effective treatment is still ongoing. Current management of COVID-19 is supportive and respiratory failure due acute respiratory distress syndrome (ARDS) is the leading cause of mortality. A clear link between diseases severity, hyper- inflammation, and major comorbidities, including hypertension, diabetes, and CVD is established.
Methodology: A scoping review methodology was used to evaluate articles published in relation to all compounds and formulations with the potential effect on disease severity, oxidative stress, and hyper-inflammatory induction in COVID-19.
Results: Numerous drugs, compounds, extracts, and formulations evaluated in the review have the potential to prevent, slow down, manage, or avert adverse outcomes associated with COVID-19. Vitamin C, Vitamin D, Zinc, and Glutathione supplementation show potential as the best dietary and supplementation approach for hyper-inflammation, oxidative stress, immune modulation, and comorbidity management. Deficiency statuses, particularly vitamin D deficiency and Zinc deficiency may likely contribute to progression in disease severity. Herbal extracts with a combination of anti-inflammatory, antioxidant, and antiviral properties may provide the most beneficial effect in COVID-19 and include curcumin, oil of Oregano, olive oil extract, flavonoids, and Echinacea.
Conclusion: Evidence presented in the scoping review indicates that proper dietary, pharmacologic, and herbal intervention targeted at disease severity, oxidative stress, and hyper-inflammatory induction in SARS-CoV-2 may help prevent, manage, and treat COVID-19.
Keywords: COVID-19, SARS-CoV-2, Dietary, Immune Response, At-Risk Group, Diabetes, Hypertension, CVD, Respiratory Disease, Cytokine Storm, Antioxidant, Oxidative Stress.
Abbreviations:
ACE2: Angiotensin Converting Enzyme-2, ARBS: Angiotensin II type-1 receptor blockers, ARDS: Acute Respiratory Distress Syndrome, ARE: Antioxidant Response Element, BWP: Bovine whey protein, CCR5: Chemokine Receptor 5, CVD: Cardiovascular Disease CWP: Camel whey protein. GR: GSSG Reductase, GSH: Glutathione, reduced glutathione, GSSG: Oxidized glutathione, IFN: Interferon, IL: Interleukin, IQR: Interquartile Range, JAK: Janus Kinase, NO: Nitric Oxide, Nrf2: Nuclear factor E2-related factor 2, Ole: Oleuropein ORF: Open Reading Frame, PMNs: Polymorphonuclear cells, RBC-GSH: Red blood cell glutathione, ROS: Reactive Oxygen Species RR: Respiratory Rate, SARS: Severe Acute Respiratory Syndrome, SBC: Social and Behavioral Change, SCT: Social Cognitive Theory STAT: signal traducer and activator of transcription proteins, TCM: Traditional Chinese Medicine, TNF: Tumor Necrosis Factor, Tregs: Regulatory T Cells, WHO: World Health Organization
Introduction
In late 2019, a cluster of severe cases of pneumonia was reported in the Wuhan region of China. Subsequent investigation identified the causative agent to be an unknown member of the Coronaviridae family. Two months later, the WHO designated the unknown viral agent as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS- CoV-2), while the ensuing illness named Corona Virus Disease 2019 (COVID-2019) (WHO 2020). COVID-19 has quickly spread around the globe with grave projections, creating a deadly emergency for nations around the world test, 2020). The preventive and therapeutic response to the novel viral syndrome has been hampered by crippling knowledge gaps in transmission dynamics, epidemiological transmission features, pathogenicity, and adequate investigation tools (Khot & Nadkar, 2020). Current intervention measures involve population-wide lockdowns, vigilant screening of suspected cases, the requirement to wear masks, isolation, and treatment of symptomatic cases, home quarantine of contacts and of those with flu-like symptoms, trial therapeutic interventions, and implementation of social distancing and strict hygiene measures as key preventive strategies. However, even in the best economies, the long-term viability of COVID-19 interventions such as lockdowns and inpatient treatment of active cases is not guaranteed. Home management of disease and symptoms are now preferred over inpatient treatment of mild COVID-19 cases. It is, therefore, crucial to develop strategies for a multi-faceted approach to the prevention, management, and treatment of COVID-19. Analysis of available evidence concerning COVID-19 disease shows that in addition to tested and experimental pharmaceutical therapies, dietary, novel therapeutic interventions and herbal remedies may offer reprieve against some of the most debilitating complications, forestall or even prevent establishment of the infection, and in effect enhance the survivability of infected persons, allowing them some level of normal societal function. The research available on COVID-19, though currently not sufficient, can facilitate a broad understanding on the nature of viral perturbation on various physiological functions and, hence, provide a framework for a broad-based intervention in the hope of preventing both morbidity and mortality.
Objectives
The present review is wide scope in nature and that is reflected in the multiplicity of specific questions that seek to be answered:
-
What is COVID-19?
-
How is the disease transmitted?
-
What is the etiologic agent?
-
What host-specific factors influence the outcome, and in what way?
-
How does SARS-CoV-2 establish itself in the host?
-
How does SARS-CoV-2 influence the immune system?
-
How do pre-existing factors affect the immune response to the disease?
-
What level of evidence exists for prevention, management, and therapeutic intervention in COVID-19?
-
What are the best opportunities for preventive, management, or therapeutic intervention?
-
From the literature review, what strategies can be used to prevent the viral establishment, delay infection progress, manage an active infection, or treat COVID-19?
Main Objective:
The main objective is to achieve a literature-based hypothesis on dietary, pharmacologic, and herbal remedies necessary for improved prevention, management, treatment, and prognosis of COVID-19.
While this review was initially intended for compounds and formulations that can be administered as dietary supplements, findings in the course of the study led to the consideration and the eventual inclusion of pharmacologic drugs and herbal remedies, and this made sense to the authors due to the need for an all- encompassing approach in combating the COVID-19 public emergency.
Specific objectives:
Three specific objectives were identified by the authors, and included the following:
-
Understanding of COVID-19, including transmission factors and pathogenesis.
-
Utilization of existing clinical data to identify persons at risk for adverse outcomes, including understanding the physiological mechanisms that account for adverse outcomes.
-
Postulating a possible link between COVID-19 pathogenesis, and particularly SARS, and elucidating key comorbidities (CVD, Diabetes, Hypertension, and respiratory disease)
-
Review of evidence on possible dietary, herbal, or prescriptive drugs that are efficacious against COVID-19, and coexisting conditions that exacerbate the situation.
Background
Virology. SARS-CoV-2 belongs to the large family, Coronaviridae, characterized by the presence of an envelope, a nucleocapsid helical symmetry, and a single-stranded positive-sense RNA genome (26 – 32 kb) (Li et al., 2020). Morphologically, the virus belongs to the group coronaviruses, which are differentiated by the presence of crown-like spikes on their surface and with a host range restricted to mammalian and avian species. Members of the family typically cause mild respiratory infections, except for a few highly virulent members, including SARS-CoV, MERS-CoV, and novel SARS- CoV-2. Coronavirus S protein has been reported as a key factor in the entry of the virus into host cells (Li et al., 2020). The envelope spike glycoprotein binds to the corresponding cellular receptor angiotensin-converting enzyme 2 (ACE2) in SARS-CoV and SARS- Cov2. This partly accounts for increased risk for diabetics and those receiving treatment with ACE inhibitors and angiotensin IItype-1 receptor blockers (ARBs) for hypertension (Fang, Karakiulakis, & Roth, 2020), although these findings have not been consistent (Fosbol et al., 2020). The level of expression of ACE2 may reflect susceptibility to COVID-19 (Wang, J. et al., 2020).
The entry of SARS-CoV into the cell was initially found to be facilitated by direct membrane fusion between the viral membrane and the membrane plasma, with an important proteolytic cleavage taking place in the S protein at position S2׳ via viral infectivity and membrane fusion (Wang, H. et al., 2008). Full-genome sequencing and phylogenetic tree analysis of SARS-CoV-2 suggests a beta coronavirus (betaCoV) in the same subgenus as SARS-CoV. Like other Coronaviruses, SARS-CoV-2 is sensitive to heat and ultraviolet rays and is effectively inactivated by lipid solvents, such as ether (75 %), ethanol (> 60 %), chlorine-containing disinfectant, peroxyacetic acid, and chloroform excluding chlorhexidine (Cascella et al., 2020).
Figure 1: A graphical depiction of SARS-CoV-2 structure.
Source: Centers for Disease Control and Prevention
Epidemiology. Coronavirus epidemics have intensified in the last three decades, albeit with wide variability in disease severity, and patterns of spread (Khot & Nadkar, 2020). SARS-CoV-2 has rapidly established itself as serious public health risk (Cascella et al., 2020). The virus is reported to have undergone animal to human transmission at the Wuhan Seafood market, but that scenario has been disputed, especially due to the finding that some of the earliest people infected with the virus in early December 2019, had no history of exposure to the market (Wu, Chen, & Chan, 2020). This has led to speculation in both published and unpublished claims of a laboratory origin of COVID -19, either through deliberate genetic engineering of animal-sourced virus to facilitate human transmission and subsequent accidental exposure, or accidental exposure to the animal-sourced human transmissible virus during investigative laboratory procedures (Chaturvedi, Ramalingam, & Singh, 2020). A study conducted by (Anderson et al., (2020) to evaluate the proximal origin of SARS-CoV-2 used genetic data to report that SARS-CoV-2 was not derived from any previously used virus backbone. The authors instead propose two scenarios, the first involving natural selection in an animal host prior to zoonotic transfer; or/and natural selection in humans before the zoonotic transfer took place (Anderson et al., 2020). Since the initial Wuhan outbreak in early December 2019, COVID-19 has quickly spread to attain a pandemic status in less than four months. Early cases outside China involved travelers from China and people who came into direct contact with these travelers. Wuhan, China apparently was the epicenter, regardless of the scenario involving the origin of the virus. On December 31, 2019, China informed the World Health Organization of a “mysterious pneumonia outbreak” that was first observed in Wuhan, an industrial city of 11 million. According to the New York Times, doctors in Wuhan were ordered to remain silent about the outbreak; one physician who issued a warning online was punished by the Chinese Communist Party (CCP), and continued to downplay the seriousness of the outbreak and initially denied human-to-human transmission as late as mid-January 2020. On January 15, 2020, in an article appearing in the Associated Press, the head of the Chinese CDC stated, “We have reached the latest understanding that the risk of sustained human-to-human transmission is low” (AP 2020). Of interest are credible reports that China restricted flights from Wuhan to mainland China but allowed flights to leave Wuhan to Europe in most of the month of January until 2 days prior to the celebration of Chinese New Year on January 24, 2020 (Elegant, 2020). On January 22, 2020, Chinese officials stopped planes and trains scheduled to leave Wuhan, blocked highways, and suspended public buses, subways, and ferries within the city, but tens of thousands of residents had already departed the city (Qin & Wang, 2020). Nine days later, on January 31, 2020, the Trump administration banned flights arriving from mainland China, with some exceptions for American citizens returning to the USA (Corkery & Karmi, 2020). Researchers in the United States first identified several cases of COVID-19 among individuals who had traveled from Wuhan, China, and who had already arrived in the US by plane in mid-January. In early March 2020, after 35 deaths from COVID had been documented in the US, the Trump administration enacted sweeping travel restrictions on 26 European countries after COVID cases had increased dramatically in Italy and many other European countries. Additionally, it was discovered that some potentially infected persons who had travelled from China to Europe were initiating new flight itineraries into the United States. As reported by BBC News, the EU condemned these restrictions, which it said were taken "unilaterally and without consultation". Officials worked to contain these early cases. However, there is some evidence that the virus was already well established in the United States in mid to late January. Researchers believe the spread may have begun with someone who arrived in the region from Wuhan on Jan. 15, 2020. (Holshue et al., (2020) report on the purported first case of COVID-19 in the United States, a 39-year-old man who visited an urgent care clinic in Washington State on January 19, 2020, with a 4-day history of cough and fever after returning to the United States on January 15th after visiting family in Wuhan (Holshue et al., 2020).
Tissue sampling from a woman who died in San Jose, California on February 6, 2020, revealed that she may be the first person in America whose death has been linked to the coronavirus. This suggests that the virus may have been circulating in Northern California at least in late January (Baker, 2020). In response to the COVID-19 outbreak, the WHO proposed a number of measures, including some precautions in international travel, such as avoiding close contact with people suffering from acute respiratory infections, and the practice of cough etiquette by travelers with respiratory symptoms (such as maintaining distance, the cover of coughs and sneezes, and washing hands) (WHO 2020). The WHO neither proposed nor issued restrictions for international travel in their January 24, 2020, recommendations (WHO 2020). Although advising against travel to COVID-endemic areas, as late as February 29, 2020, the WHO was still maintaining that” travel bans to affected areas or denial of entry to passengers coming from affected areas are usually not effective.” These updated recommendations stated that “WHO continues to advise against the application of travel or trade restrictions to countries experiencing COVID-19 outbreaks” (WHO 2020). Assessments by the WHO provided a basis response in various countries, and contrary to the current recommendation of the WHO, the U.S. implemented an international travel ban on January 31st following a surge in cases in China and growing numbers in other countries. Unpublished reports show mixed findings on the strategies currently employed to prevent the spread of COVID-19. While some US regions and countries have shown a spike in cases following the easing of lockdowns, others have not shown a spike in COVID-19 cases.
Numerous localized outbreaks in many countries continue to take place, with rates of new cases in some countries outpacing those in China. Infection rates in China have begun to decline following austere containment policies which were enacted several months ago by the Chinese government, although some sources suggest significant under-reporting of cases by The Chinese government (Russel, Hellewell, & Abbot, 2020). In the United States, COVID- 19 transmission is localized in numerous clusters in almost all the states, with the greatest concentration at the time of this writing in Washington State, New York, New Jersey, Illinois, Michigan, and California (Mclntosh, Hirsch, & Bloom, 2020; CDC, 2020). As of March 16, the highest cases outside China include Italy (21,157), Iran (13,938), South Korea (8,162), Spain (7,798), Germany (5,426), France (4,511) and the U.S. (3,244), (ArGIS 2020), but with the massive increase in testing capabilities now available in the US, these case numbers will surely increase, at least transiently. Unproven claims suggest that the pandemic may have originated from bats following viral mutation in the spike glycoprotein, which enabled the human-to-human transmission (Angeleti et al., 2020). An analysis pipeline developed by (Korder et al., (2020) to facilitate real-time mutation tracking in SARS-C0V-2, and focusing initially on spike (S) proteins, showed that fourteen mutations in spike was accumulating and, therefore, affecting the ability to develop vaccine strategies and antibody-based therapeutics against COVID-19 (Korber et al., 2020).
Transmission
Although the person-to-person transmission was initially denied in early reports on January 15, 2020 by the WHO, the Chinese CDC, and the Chinese Communist Party (CPC), person-to-person transmission of SARS-CoV-2 is believed to occur via droplets to the respiratory mucosa mainly from symptomatic patients (but not excluding asymptomatic patients), which occurs in close contact, or a similar pattern to that of influenza (Dietz et al., 2020). A cough, sneeze, or conversational talk by an infected person releases the virus in droplets and in secretions, likely infecting another person who comes into direct contact with the droplets, or essentially, the mucous membranes of an infected person. Transmission can also take place when an individual touches an infected surface and then touches his or her eyes, nose, or mouth. Droplets are believed not to travel more than six feet (approx. 2 meters) and do not linger in the air for more than two to three minutes. (Van Doremalen et al., (2020) evaluated the aerosol and surface stability of SARS-CoV-2 in comparison with SARS-CoV-1 and found that while the two viruses had comparable levels of stability, differences in epidemiologic characteristics arose due to factors such as high viral load in the upper respiratory tract and the ability for the asymptomatic spread in SARS-CoV-2 (Van Doremalen et al., 2020). (Van Doremalen et al., (2020) also found that SARS-CoV-2 was more stable on plastic and stainless steel than copper and cardboard, and the viable virus was detected up to 72 hours following application on these surfaces. It is believed that SARS-CoV-2 may not be airborne, but due to the limited understanding of transmission mechanisms, airborne precautions are recommended. Besides respiratory droplets, the virus can also be spread through sweat, stool, and urine; and once in the body, it binds on enterocytes and pneumocytes, which form the initial site of infection and replication (Prajapat et al., 2020).
The etiologic evolution of the novel SARS-CoV-2 is currently under intense investigation, with significant progress in knowledge about COVID-19 attained from the Wuhan outbreak. The incubation period for COVID-19 is believed to be up to 14 days after exposure to SARS-CoV-2, with median incubation reported being 3 or 4 days (Guan et al., 2020). Besides symptomatic transmission, evidence on asymptomatic transmission of SARS-CoV-2 exists, although no current understanding exists regarding the extent to which this occurs in the population (Rothe et al., 2020). This virus is highly communicable. Evidence from a recent study shows that the rapid spread of SARS-CoV-2 takes place with an estimated average R0 of 3.28 (i.e the expected number of cases directly generated by one infected person in a population where all individuals are susceptible to infection would be 3.28 cases), which exceeds the WHO estimation of 1.4 to 2.5 (Liu et al., 2020). Based on the available data, a majority of the COVID-19 cases (approx. 80 %) presented with asymptomatic or with mild symptoms while the remaining 20% were either severe or critical (Prompetchara, Ketloy, & Palaga, 2020).
The finding of genome similarity with SARS-CoV, coupled with data from nucleic acid sequence analysis in the spike protein receptor-binding domain (RBD) predicts utilization of angiotensin- converting enzyme 2 (ACE2) as a cell receptor (Prompetchara, Ketloy, & Palaga, 2020). Viral entry into host cells also require cleavage of the viral S protein by host proteases, which results in irreversible conformational changes to the S protein which allow fusion between virus and host cell membrane (Lin et al., 2020). The host serine protease TMPRSS2 or the cysteine proteases cathepsin B or L (CatB/L) are used to achieve S protein cleavage (Simmons et al., 2005). Based on this, potential therapy targeting viral entry can be achieved by the use of serine protease or cysteine protease cathepsin inhibitors (Simmons et al., 2005; Vidal-Albalat & Gonzalez, 2016; Yamoto et al., 2016). A recent single-cell RNA- sequencing study of human and non-human primate tissues revealed the three major cell types that co-express TMPRSS2 and ACE2, including type II pneumocytes in the lung, absorptive enterocytes in the terminal ileum, and the nasal goblet secretory cells (Ziegler et al., 2020).
Clinical Characteristics and Disease Severity. Ongoing research has already identified a wide range of symptoms associated with COVID-19 infection. Patients with COVID-19 generally show clinical manifestations that include fever, non-productive cough, dyspnea, myalgia, fatigue, anosmia, ageusia, and radiographic evidence (lobular ground-glass opacity) of pneumonia (Li et al., 2020; Vaira et al., 2020). COVID-19 may also cause ischemia that causes cyanotic or “blue toes” in patients (Frankhauser, 2020). Based on findings from clinical trials, (Zu et al., (2020), recently established criteria for clinical severity for confirmed COVID-19 pneumonia, including the following categories: mild, moderate, severe, and critical. Details of the criteria are in the table below.
Table 1: COVID-19 Severity Types
|
Severity |
Findings |
|
Mild (uncomplicated Illness) |
Includes mild clinical symptoms, such as fever 38℃ (resolves without treatment), and which may present with or without cough, no gasping, no chronic disease, no dyspnea. |
|
Moderate |
Involves fever, respiratory symptoms, evidence of pneumonia as shown by imaging. |
|
Severe |
Severe COVID-19 involves any of the following symptoms:
*CT imaging shows a rapid progression (> 50 %) within 24 hours and the disease should be managed as severe. |
|
Critical |
A critical case meets the following criteria:
|
Criteria compiled by (Zu et al., (2020).
Clinical characteristics are described in a number of trials conducted in the course of the outbreak. A retrospective study conducted by (Cao et al., (2020) on 128 COVID-19 cases, and aimed at establishing clinical characteristics showed that 89.8 % of the cases had fever, 67.2 % had cough, while a minority, 14.1 %, had a sore throat. Strong evidence of symptom variation in COVID-19, depending on factors such as age and existing infections was established. According to Guan et al., females constituted 41.9 %; persons aged below 15 years accounted for 0.9 %; patients with severe symptoms were older by the median of 7 years compared to those with less severe symptoms; and the presence of a coexisting illness, including hypertension, cardiovascular disease, and diabetes, was associated with more severe symptoms (2020). In another study, persons aged less than 20 years accounted for 1.6 % of the patients; those aged 21-50 years constituted 44.5 %; 51-65 years constituted 35.1 %; while 18.8 % were older patients aged 66 years and above (Cao et al., 2020). A follow-up on a 6-month-old infant with a high SARS-CoV-2 viral load showed that the infant remained asymptomatic for the 16 days he was admitted (Kam et al., 2020). Common complications observed in severe disease include acute respiratory distress syndrome (ARDS), which was observed in 15.6 % (27/173) of patients with severe disease; physician-diagnosed pneumonia, observed in 172 patients or 99.3 % of those with severe disease; and septic shock, observed in 6.4% of those with severe disease (Guan et al., 2020). Emerging evidence also shows that acute kidney injury (AKI) may be one of the severe complications of COVID-19, and hence, highlighting the need for assessment, definition, and reporting on the same (Battle et al., 2020). A CDC report documenting severe outcomes among patients with COVID-19 in the United States revealed that fatality was highest in persons aged ≥ 85 (which ranged from 10 % to 27 %), followed by 3 % to 11 % in persons aged between 65-84 years, 1% to 3% among persons aged 55-64 years, < 1 % in persons aged 20–54 years, and zero fatalities in persons aged ≤ 19 years (CDC, 2020). More details on hospitalizations, intensive care unit (ICU) admission, and case-fatality percentages for reported COVID-19 cases are provided in the table below.
Table 2: U.S. Age-based Hospitalization, ICU admission, and Case-Fatality as of March 2020
|
Age group in years (No. of cases) |
% |
||
|
Hospitalization |
ICU Admission |
Case-Fatality |
|
|
0 – 19 (123) |
1.6 – 2.5 |
0 |
0 |
|
20 – 44 (705) |
14.3 – 20.8 |
2.0 – 4.2 |
0.1 – 0.2 |
|
45 – 54 (429) |
21.2 – 28.3 |
5.4 – 10.4 |
0.5 – 0.8 |
|
55 – 64 (429) |
20.5 – 30.1 |
4.7 – 11.2 |
1.4 – 2.6 |
|
65 – 74 (409) |
28.6 – 43.5 |
8.1 – 18.8 |
2.7 – 4.9 |
|
75 – 84 (210) |
30.5 – 58.7 |
10.5 – 31.0 |
4.3 – 10.5 |
|
≥ 85 (144) |
31.3 – 70.3 |
6.3 – 29.0 |
10.4 – 27.3 |
|
Total (2,449) |
20.7 – 31.4 |
4.9 – 11.5 |
1.8 – 3.4 |
|
*Lower bound of range = indicates the number of persons hospitalized, admitted to the ICU, or that died in the total age group; upper bound of range = number of persons hospitalized, admitted to ICU, or who died among total in age group with known hospitalization status, ICU admission status or death. |
|||
Source: Centers for Disease Prevention and Control, August 2020. However, according to (Fauci et al., (2020), the case fatality rates in COVID-19 may be considerably less and more comparable to those of a severe seasonal influenza (which has a case fatality rate of approximately 0.1 %) or pandemic influenza (similar to those in 1957 and 1968) rather than a disease similar to SARS or MERS, which have had case fatality rates of 9 to 10 % and 36 %, respectively. The analysis by (Fauci et al., (2020) based on the fact that the number of asymptomatic cases of COVID-19 may be several times higher compared to the reported cases.
Diagnostic Findings. Diagnosis in COVID-19 can be made by specific RT-PCR of nasopharyngeal or oropharyngeal swabs and lower respiratory tract samples with median viral shedding of 20 days, and an interquartile range (IQR) of 17-24 days (Zhou et al., 2020). The virus can also be diagnosed from stool samples (Weinkove et al., 2020). Available data shows that many laboratory parameters are abnormal in COVID-19 patients, with some identified as predictors of adverse clinical outcomes (Lippi & Plebani, 2020). Preliminary data on the abnormalities in the asymptomatic, non-severe cases, and severe cases, are available. The most frequent abnormalities reported for the non-severe cases include elevated values of C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), lactate dehydrogenase (LDH), and D- Dimer and these abnormalities were commonly identified in patients during admission (Lippi & Plebani, 2020; Guan et al., 2020). (Del Rio & Malani (2020) documented lymphopenia as the most common abnormal laboratory finding (70 %), prolonged prothrombin time (58 %), and elevated lactate dehydrogenase (40 %). Chest imaging results, which may include chest radiograph, CT scan, or lung ultrasound, are dominated by bilateral and peripheral ground glass, and consolidative pulmonary opacities or lung infiltrates > 50 %) (Bernheim et al., 2020).
Immunopathology. Evidence on host immune responses to SARS-CoV-2 is rapidly accumulating. Preliminary findings on immune response identified clinically patterns of the virus and genetic association with SARS-CoV and MERS-CoV can be used to hypothesize immune responses to SARS-CoV-2. Aggregate data from various studies investigating immune response to COVID-19 show a dysregulated immune response (Shi et al., 2020; Deng & Pei, 2020; Prompetchara, Ketley, & Palaga; 2020; and Li et al., 2020). (Shi et al., (2020) analyzed various immunopathological characteristics of COVID-19 patients in Guangzhou, China, and reported the following in severe disease: an overall decline of lymphocytes, including substantial reductions CD4+, CD8+ T cells, and NK cells; and a remarkable up-regulation in IL-2, IL-6, and IL- 10. The decline in CD4+ and CD8+ T cell numbers in SARS-Cov-2 has been corroborated by other studies (Li et al., 2020). Findings from studies of SARS-CoV show that even in the absence of antigens, CD4+, and CD8+ memory T cells and can perform a delayed type of hypersensitivity response (DTH) and production of IFN-γ thus exacerbating the pathogenic storm of cytokines associated with this infection (Fan et al., 2009).
Numerous reports have shown that ARDS is the major cause of death in COVID-19. ARDS is a common immunopathological event experienced in SARS-CoV-2, SARS-CoV, and MERS-CoV viral infections. A key mechanism of the ARDS is the cytokine storm, uncontrolled systemic inflammatory response that results from the uncontrolled release of large amounts of pro-inflammatory cytokines (IFN-a, IFN-γ, IL-1b, IL-6, IL-12, IL-18, IL-33, TNF-a, TGFb, among others) and chemokines (CCL2, CCL3, CCL5, CXCL8, CXCL9, CXCL10, etc.) by the immune effector cells in SARS-CoV infections (Li et al., 2020). In COVID-19, prediction of inflammatory response is essential since it plays a major role in lung damage and subsequent mortality (Stebbing et al., 2020).
Evidence shows that the Janus Kinases (JAKs), signal traducer and activator of transcription proteins (STATs), otherwise referred to as JAK-STAT, a molecular pathway of the signaling pathway involved in processes in the body, such as immunity, cell division, and formation of tumors, may be involved in the hyper-inflammation observed in COVID-19 and, therefore, presenting a potential therapeutic intervention using JAK inhibitors (Banerjee et al., 2017; Mehta et al., 2020). Many cytokines involved in the pathogenesis of inflammatory and autoimmune disease use the JAK and STAT signals to transduce intracellular signals (Banerjee et al., 2017). There are four types of JAK (JAK1, JAK2, JAK3, and TYK2), with each of them involved with different JAK-dependent cytokine receptors (Clark, Flanaga, & Telliez, 2014). The extent to which a specific cytokine (type I/II) may rely on the role of a JAK to traduce signals is dependent on the subunits of the cytokine receptor (Banerjee et al., 2017). For instance, the common γ-chain (γc), used by IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21, associates exclusively with JAK3 and is the only receptor subunit that uses JAK3 (Hofmann et a., 2002). A case series study conducted by (Haberman et al., (2020) in New York City showed a significant number of COVID-19 patients had an immune-mediated inflammatory disease (IMID), and this highlighted potential therapies of anti-cytokine and other immunosuppressive therapies, such as JAK inhibitors and IL-6 inhibitors or receptor blockers.
Immune Evasion. Mechanisms of immune evasion have been well documented in SARS-CoV and MERS-CoV. Normally, the evolutionary conserved microbial structures called pathogen- associated molecular patterns (PAMPs) are detected by pattern recognition receptors (PRRs). An evasion mechanism observed in both MERS-CoV and SARS-CoV is inducing the production of double-membrane vesicles that lack the PRRs and then replicating in the vesicles, thereby evading host detection of their dsRNA (Snijder et al., 2006). Type I interferon (IFN-α and IFN β) confer a protective effect on MERS-CoV and SARS-CoV, though the pathway which is blocked in infected mice (Channappanavar et al., 2016). Accessory protein 4a and open reading frames (ORF4a, ORF4b, and ORF5) inhibit IFN activity in MERS-CoV (Niemeyer et al., 2013; Yang et al., 2013). Due to limitations in existing experimental tools, the roles of many SARS-CoV-2 proteins, including ORFs, are still unclear (Liu & Li, 2020).
At-Risk Groups and Immune Function Impairment
Several risk factors have been identified for poor prognosis in COVID-19, with increased odds of in-hospital mortality, found to be higher in patients of older age, and with hypertension, diabetes, cardiovascular disease, cerebrovascular disease, and malignancy, as reported by various retrospective studies. A key finding since the outbreak of COVID-19 is that advanced age increases the risk of severe disease and mortality. This has been proposed to relate to the various comorbidities prevalent in older adults. In a prospective cohort study involving 701 patients with COVID-19 admitted in a tertiary teaching hospital following the outbreak in Wuhan, 113 (16.1 %) died in hospital (Cheng et al., 2020). The median age of the admitted patients was 63 years, (IQR, 50-71), admitted with proteinuria (43.9 %) and haematuria (26.7 %), (Cheng et al., 2020). In a study by Guan et al., (2020) at least 23.7 % of more than 1099 patients admitted to various hospitals with COVID-19 had at least one coexisting illness. (Wang, D. et al.,(2020) identified hypertension (31.2 %), cardiovascular disease (14.5 %), diabetes (10.1 %), malignancy (7.2 %), and cerebrovascular disease (5.1 %), as key comorbidities among 138 hospitalized patients with COVID19. As reported by (Yang et al., (2020), the most outstanding comorbidities in 32 non-survivors from a group of 52 patients admitted to the intensive care unit with COVID-19 were cerebrovascular disease (22 %) and diabetes (22 %). (Fang, Karakiulakis, & Roth (2020), conducted a review to find out whether patients suffering from hypertension and diabetes mellitus were at an increased risk of COVID-19 infection, and these authors linked the increased susceptibility to the ACE2 viral entry pathway.
A more recent systematic review, published in May 2020, includes findings from seven different studies that involved a total of 1576 infected patients (Yang J, et al., 2020). The findings of the review by (Yang, J. et al., (2020) showed that the most prevalent comorbidities in COVID-19 were as follows: hypertension (21.1 %, 95 % CI: 13.0–27.2 %); diabetes (9.7 %, 95 % CI: 7.2–12.2 %); cardiovascular disease (8.4 %, 95 % CI: 3.8–13.8 %); and respiratory system disease (1.5 %, 95 % CI: 0.9–2.1 %).
As earlier described, SARS-CoV and SARS-CoV 2 bind target cells through ACE2, which is substantially expressed in patients with type 1 and type 2 diabetes, and individuals that are treated with ACE inhibitors and Angiotensin II type-1 receptor blockers (ARBs), such as those with hypertension (Wan et al., 2020). It has been hypothesized that diabetes and hypertension treatment with ACE2- stimulating drugs increases the risk of developing severe and fatal COVID-19 (Fang, Karakiulakis, Roth, 2020).
In relation to cancer, there has been a general concern based on the accumulated evidence that shows a blunted immune status in association with cancer development and effect in COVID-19 (Xia et al., 2020). According to one study, patients with cancer deteriorated more rapidly than those without cancer (Liang et al., 2020). Immune system features associated with cancer, and which are likely to enhance the risk of COVID-19 include overexpression of immunosuppressive cytokines, a diminished induction of the pro- inflammatory danger signaling, impaired maturation of dendritic cells, and an increased number of immunosuppressive leukocyte populations. An interim consensus guidance on the management of haematology and oncology inpatients with COVID-19 should broadly consider the following: clinical presentation, diagnosis and treatment considerations; possible risk factors for severe COVID-19 disease, including advanced age and medical comorbidities; modification of cancer therapies in relation to the safety and health demands of COVID-19; identification of alternative ways to keep patients and families informed; special consideration for cancer- related blood transfusion; and consideration for other special circumstances, such as cellular therapies and bone marrow transplantation, clinical trial participation, and palliative care (Weinkove et al., 2020).
Smoking.
Smoking has also been found as a key risk factor for COVID-19. A susceptibility analysis conducted by (Wang, J. et al., (2020) using both human and rat data showed that cigarette smoking-induced an increase in ACE2 in the respiratory tract, which suggested that smokers were at increased susceptibility to COVID-19. At least one study conducted in France by (Miyara et al. (2020) found that active smokers may be protected against symptomatic COVID-19. Only 5 % of 482 Covid-19 patients who came to the Pitié-Salpêtrière hospital in Paris between February 28th and April 9th were daily smokers. This was seen among outpatients (who have less serious infections) as well as among hospitalized patients. The authors postulated that “the physio pathological process underlying this finding may involve nicotine through the nicotinic receptor (and not the smoke of cigarettes per se), a hypothesis which deserves further evidence” (Miraya et al., 2020). The authors encouraged caution in the interpretation of these findings. Similar findings on the suppressive effect of smoking on the coronavirus were published by (Guan et al. (2020) in the New England Journal of Medicine, who found that, of 1099 patients infected in China, 12.6 % were smokers, versus 26 % in the general population. Additional investigations are currently underway to confirm the effectiveness of nicotine patches in COVID-19.
Comorbidities and Oxidative Stress in COVID-19. While no research has established a direct link between COVID- 19 and oxidative stress, major COVID-19 comorbidities, including diabetes, CVD, and hypertension are associated with oxidative stress. Reactive oxygen species (ROS) are small, highly reactive molecules that contain oxygen, and which are naturally generated in minute amounts during metabolic reactions, and damage or react with complex cellular molecules including DNA, fat, and proteins (Wu & Cederbaum, 2003). “Oxidative stress” is generally defined as any disturbance in the balance of antioxidants and pro-oxidants in favor of the latter due to various factors that may include aging, drug actions and toxicity, inflammation, and/or addiction (Asmat, Abad, & Ismail, 2016). In general, oxidative stress occurs following excessive formation and/or insufficient removal of highly reactive molecules such as reactive nitrogen species (RNS) and ROS (Johansen et al., 2005). Oxygen is a highly reactive molecule and may become part of molecules that are potentially harmful and damaging (free radicals), which attack cells and cause them to lose their function and structure (Asmat, Abad, & Ismail, 2016). It has been shown that whereas low levels of ROS are essential for cell survival and proliferation, high concentrations may initiate DNA damage ad cell death (Cairns, Harris, & Mark, 2011; Gorrini, Harris, & Mark, 2013). Metabolites of oxidative stress have been suggested to play a role in the pathophysiology of renovascular hypertension and renal damage (Shanley, 1996). The progression of several human diseases, including diabetes and atherosclerosis, is reported to be associated with free radicals (Chiou et al., 2017). The oxidative stress mechanism involved in hypertension has been proposed to involve the conversion of oxygen free radicals (superoxide) with the NO to form peroxynitrite, which has a greater oxidative capacity compared to all other compounds (Pryor & Squadrito, 1995). The increased superoxide production is linked to Angiotensin II (Ang ii) as demonstrated by (Rajagopalan et al., (1996). A review of several studies show that hypertension may be induced by smaller elevations in circulating levels of angiotensin that are not appropriate for the existing levels of extracellular fluid volume, and also show that hypertension may alsoresult if the intake of sodium is inappropriate with existing levels of circulating Angiotensin II (Romero & Reckelhoff, 1999). Essential hypertension is a major factor in the development of CVD, renal failure, and stroke (Wong et al., 2001). In relation to CVD, ROS are now known to function as signaling molecules that regulate a wide range of processes in the cardiovascular system and help in the maintenance of cardiovascular homeostasis (Droge, W. 2002). Sustained and/or excessive ROS generation plays a critical role in the pathological changes observed in CVD (Touyz & Briones, 2011). Oxidative stress has been implicated in the onset and progression of diabetes, and in the emergence of complications. The oxidative environment may result in the development of insulin resistance, β-cell dysfunction, mitochondrial dysfunction, and impaired glucose tolerance that may ultimately lead to a diabetic state (Rains & Jain, 2011). Oxidative stress is inferred in diabetes pathogenesis through alteration of enzymatic systems, lipid peroxidation, impaired glutathione metabolism, and decreased levels of vitamin C (Asmat, Abad, & Ismail, 2016). Oxidative stress results in the increased superoxide production, which plays a key role in the development of diabetes complications through five key pathways: polyol pathway, increased formation of advanced glycation end products (AGES), increased expression of receptors for AGES, and activation of protein kinase C isoforms, the activation of ligands, and hyperactivity of the hexosamine pathway (Giacco & Brownlee, 2010). Diabetes is the leading worldwide cause of blindness, end-stage renal disease, macrovascular complications (such as strokes and myocardial ischemia), as well as amputations, with all of the aforementioned pathways involving a common feature of increased oxidative stress that is marked by an increase in the levels of ROS (Sekhar et al., 2011). Additionally, aging, which is regarded as an impairment of body functions over time as a result of the accumulation of molecular damage in DNA, proteins, and lipids, is also associated with an increase in intracellular oxidative stress that takes place following the continued decline in intracellular ROS scavenging (Minella et al., 2009). The oxidative stress the hypothesis is supported by data from studies investigating the disproportionate the ability of COVID-19 to adversely affect people with the described comorbidities. A study conducted by (Mehra et al., (2020) investigated whether the increased COVID-19-associated morbidity and mortality in patients CVD was due to the harmful effects of ACE inhibitors or angiotensin receptor blockers (ARBs), but the findings showed the use of ACE inhibitors and ARBs were in fact associated with increased survival rates.
Oxidative Stress Mechanism and the Inflammatory Response, including ARDS and SARS. As noted earlier, the imbalance that takes place between the production of oxidants and their elimination by protective mechanisms typically may take place in all cells of the body as this occurs in normal cellular metabolism (Durackova, 2010). Most ROS products are generated during the mitochondrial respiratory chain, and these include superoxide anion (O2-), hydrogen peroxide (H2O2), hydroxyl radical (OH•), and organic peroxides occurring as normal products during the reduction of the oxygen molecule (Poyton, Ball, & Castello, 2009). In hypoxic conditions, mitochondrial respiration produces Nitric Oxide, which can generate other reactive nitrogen species through the induction of excessive lipid peroxidation (Reuter et al., 2010). During sustained conditions of environmental stress, ROS production occurs over an extended period, causing significant damage to the cell structure.
Inflammation may take place due to a wide variety of causes, including microbial and viral infections; exposure to toxic and radiation chemicals; conditions such as autoimmune, chronic diseases, and obesity; and consumption of alcohol, tobacco use, and high calorie diet (Reuter et al., 2010). Oxidative stress may account for inflammation, marked by increased circulating levels of IL-6 and TNF-α in chronic conditions such as diabetes, where the increase of ROS occurs because of acute hyperglycemia (Esposito et al., 2002). There are two stages of inflammation, including acute and chronic inflammation, mostly differentiated by the length of time taken before the inflammatory response resolves. In addition to the contribution of existing ROS to the inflammatory response, a respiratory burst occurs during inflammation following the recruitment of mast cells and leukocytes to the site of damage and increased oxygen utilization, which causes a further accumulation of ROS at the site of damage (Nagata, 2005). Inflammatory cells also continue to produce soluble mediators (such as cytokines and chemokines) which continue to recruit other inflammatory cells, producing more reactive species.
Lung tissue is generally exposed to higher oxygen concentration levels in comparison to other tissues in the body, with increased oxidative stress, found to be part of the pathogenesis of obstructive lung diseases, such as asthma, parenchymal lung disease, and chronic obstructive pulmonary disease (Barbaro et al., 2007; Kinnula & Crapo, 2003). Oxidant protection in the lung tissue is achieved through a variety of mechanisms among which superoxide dismutases (SODs) are vital (Kinnula & Crapo, 2003). There are three different mammalian SODS involved in the decomposition of superoxide radicals to H2O2 and include intracellular copper-zinc SOD (CuZnSOD), extracellular SOD (EC-SOD), and mitochondrial manganese SOD (MnSOD), which have been detected classes of lung tissue but with significant variability and cell-specificity (McCord & Fridovich, 1969). Numerous scavenging enzymes are involved in the H2O2 degradation in the lung, most important of which include glutathione peroxidases and catalase (Kinnula & Crapo, 2003).
The elucidation of key inflammatory mediators (such tumor necrosis factor (TNF)‐α, interleukin (IL)‐1β, IL‐6, platelet-activating factor (PAF), IL‐10, granulocyte macrophage‐colony stimulating factor (GM‐CSF), complement component C5a, intercellular adhesion molecule (ICAM)‐1, substance P, chemokines (VEGF, IGF‐I, KGF,) in the lungs as a response to the earlier established causes of inflammation, coupled with the continued rise in the level ROS and reactive nitrogen species (RNS) play a key role in the pathogenesis of ARDS. The dysregulated response by pro- inflammatory cytokines is a key feature in SARS as shown by the finding of increased serum levels of cytokines in SARS and COVID-19 patients (Gu & Korteweg, 2007; Qin et al., 2020). Available evidence points to the role of oxidative stress in the induction of inflammation and the formation of abundant fibrotic tissue which impairs organ function, as partly observed in ARDS and SARS (Gu & Korteweg, 2007; Pizzino et al., 2017; Bhatia & Moochhalia, 2004). Based on these findings, provision of antioxidant supplementation, coupled with specific inhibitors of key pro- inflammatory mediators may provide a treatment option for severe COVID-19. Such supplementation may also, confer protection against major comorbidities in COVID-19 (old age, hypertension, diabetes, CVD, respiratory disease), which are all associated with oxidative stress, a possible major factor in severe COVID-19 pathogenesis as evidenced above.
Treatment, Therapeutic agents, their Mechanisms of Action, and Prognosis Factors. Timely and effective therapeutic intervention in COVID-19 is greatly hampered by the lack of effective vaccines and drugs and, hence, a major contributing factor to the observed adverse outcomes. Preliminary investigations show that several drugs may have antiviral activity against COVID-19. Dong, Hu, and (Gao (2020) have evaluated various drugs with potential efficacy against COVID-19. Emerging in vitro data shows that chloroquine or chloroquine phosphate (used interchangeably), a widely used antimalarial and autoimmune disease drug, may inhibit SARS-CoV2-2 replication (Touret & de Lamballerie, 2020). Past research has shown some in-vitro activity of chloroquine against viruses, but no beneficial effect has been shown in animal models (Touret & de Lamballerie, 2020). Multicenter clinical trials conducted in China showed that chloroquine phosphate had an apparent efficacy and acceptable safety against pneumonia associated with COVID-19 (Gao, Tian, & Yang, 2020). It is postulated that chemical components in chloroquine phosphate compete with porphyrin and bind to the viral protein, which inhibits viral protein attack on heme or binding to the porphyrin (Liu & Li, 2020). Another antimalarial drug, hydroxychloroquine, which has similar pharmacological activity as chloroquine, has also been used and recommended for hospitalized COVID-19 patients for reducing or eradicating viral load (Gautret et al., 2020).
Azithromycin has also been administered alongside hydroxychloroquine to prevent bacterial super-infection (Gautret et al., 2020), and may enhance the effectiveness of hydroxychloroquine through some unknown mechanism. While research on the effectiveness of chloroquine and hydroxychloroquine against SARS-CoV-2 is still ongoing, their known safety profiles and good tolerance has been established in COVID-19 (Colson et al., 2020). Remdesivir, an investigational intravenous drug that generally inhibits viral replication through premature termination of RNA transcription and has in vitro activity against SARS-CoV-2, is used for the treatment of hospitalized patients with COVID-19 and pneumonia (Wang, M. et al., 2020). Favipiravir is another broad-spectrum antiviral drug being studied in the treatment of COVID-19 treatment (Dong, Hu, & Gao, 2020). Evidence exists that Traditional Chinese Medicine (TCM) has been used in combination with Western medicine with some success in the treatment of COVID-19 (Ni et al., 2020). Therefore, while TCM is mainly described as preventive, these authors found that it may be used for treatment purposes when combined with conventional Western medicine. Nabirotchkin et al., (2020) investigated the unfolded protein response and autophagy-related pathways to reposition common approved drugs against COVID-19. The authors aimed at enabling fast track of already approved medication for population use in COVID-19 treatment, and this included previously approved drugs, utilizing the unfolded protein response (UPR) pathway and autophagy pathways of host cells, which have been found to be important for the life cycle of previously characterized coronaviruses (Nabirotchkin et al., 2020). Using repositioning strategies, the authors prioritized two additional druggable pathways that were similarly important for the viral cycle and tightly linked to UPR/autophagy signaling, including the mitochondrial permeability transition pores (MPTP) and NLRP-3 inflammasome pathways (Nabirotchkin et al., 2020).
Poor prognosis in COVID-19 is currently found to be associated with multilocular infiltration on the chest imaging, bacterial co- infection, smoking history, diabetes, lymphopenia, chronic conditions such as hypertension, and age > 60 years (Khot & Nadkar, 2020). A rough assessment of the prognostic factors points to immune function and oxidative status as important factors to consider in COVID-19. A study reviewing the development of the immune system from infancy to old age concluded that the poor immune status in the very young and the very old may reflect the importance of the young adult in the procreative potential and survival of a species, as evidenced by similar patterns in antimicrobial activity by neutrophils and macrophages, reduced antigen presentation and decreased NK killing activity, and somewhat compromised adaptive lymphocyte responses in the newborn and the aged organisms (Simon, Hollander, & McMichael, 2015). An increase in oxidative stress associated with the production of ROS during mitochondria respiration in chronic comorbidities (such as diabetes and malignancies) is thought to play a role in the decreased serological efficacy of influenza vaccines among the elderly, who also tend to be more prone to pulmonary complications (Song et al., 2010). An attack on the mitochondrial DNA (mtDNA) results in mutations that alter the function of mitochondrial respiratory complex, leading to increased production of reactive oxygen species and more damage to the mtDNA (Judge et al., 2005). Reduced white blood cell and lymphocyte counts were demonstrated in most of the investigated cases, with lymphopenia, consistently stressed to be a negative prognostic factor (Cascella et al., 2020). Lymphopenia is mentioned extensively in clinical and pathological findings in severe cases of COVID-19 and is increasingly thought to be a critical factor in disease severity and mortality. Findings of a systematic review conducted by (Vardavas & Nikitara (2020) showed that smoking was associated with negative progression and adverse outcomes in COVID-19. A finding that could be due to existing evidence on the blockage of the antiviral effects of IFN-γ by cigarette smoke extract, which increases susceptibility to respiratory viral infection in persons exposed to cigarette smoke (Modestou et al., 2010).
For severe and critical cases, measures such as protective mechanical ventilation, high-flow nasal oxygen (HFNO), or non- invasive ventilation (NIV) is indicated. Other therapeutic strategies, such as the use of corticosteroids for the treatment of viral pneumonia or ARDS are not recommended (Cascella et al., 2020). Prevention Strategies. At present social and behavior change (SBC) is the most efficacious means of limiting SARS-CoV-2 transmission. Theoretically, SBC promotes the change of attitudes, perceptions, and practices, usually in relation to health and dietary decision-making. While the benefits of dietary modification are not completely understood, a drastic modification in social and hygiene behaviors significantly slows COVID-19 community transmission (Dalton et al., 2020). Reducing the number of contacts each person makes reduces the risk of transmission per contact and the epidemic potential of SARS-CoV-2. Ideally, a distance of 2 meters is recommended between two individuals, particularly when contact is made with an individual with suspected symptoms. Hygiene measures are mostly secondary as they reduce the risk of transmission if direct contact is established with contaminated material or an infected person. Epidemiological observations in China show that pre-emptive implementation of social distancing and hygiene measures may be effective in preventing widespread community transmission and the outbreak of COVID-19 (Dalton et al., 2020).
There have been reports that Chinese herbal formulae maybe helpful in the prevention of COVID-19. Available historical records show that Traditional Chinese Medicine (TCM) has been used in the prevention and treatment of infections, including existing clinical evidence for use of the herbal formulae for the treatment and prevention of SARS and H1N1 influenza (Luo et al., 2020). Chinese authorities have also directed health care providers to use TCM in their COVID-19 prevention programs (Wang, Z. et al., 2020). While there is a need for rigorous prospective studies on the potential prevention effect of TCM, existing evidence shows that the formulation provides an alternative approach for the prevention of COVID-19) (Luo et al., 2020).
Theoretical Framework
The proposed dietary protocols for the management of COVID-19 in at-risk groups utilize a theoretical framework proposed in the Social Cognitive Theory (SCT) (Stacey et al., 2015). According to the theory, people are not driven by inner forces, but by external factors that motivate them to make choices. The key constructs of SCT include the following: knowledge of health risks and benefits; perceived self-efficacy that a given person can take charge of their own health habits; the expected outcomes or costs and benefits; consideration of the proximal and distant intentions to engage in the behavior; social support and facilitators of the health behavior; and the barriers to the making of the required changes (Bandura, 2004). The SCT model proposes an understanding of human functioning through interaction between behavior, personal, and environmental factors, often referred to as reciprocal determinism. COVID-19 represents a situational influence that generally demands behavior mediation based on learning derived from the available evidence. While broad behavior changes are required in response to any pandemic, proposed protocols suggest optimizing dietary interventions for enhancing immune function, particularly in the identified at-risk groups. These include persons with a general immunocompromised status, the elderly (> 65), and those with coexisting illness (such as hypertension, lung disease, cardiovascular disease, and diabetes), which have been collectively associated with adverse clinical outcomes in this pandemic. The protocols may also help address problematic dietary patterns that may exacerbate risk by contributing to obesity and to the co-morbidities identified above.
2.0 Methods
Scoping review methodology is appropriate for the present study area given the complexity, preliminary and broad nature of existing research on the topic. The intention is to identify and define the efficacy or mechanism (if possible) of possible agents, compounds or formulations that can potentially be used to intervene in COVID-19. We also aimed at explicating various agents/compounds described in literature and characterizing them according to evidence of pharmacologic effects and mode of use (either as a dietary supplement, pharmacologic drug, or herbal remedy). We followed the preferred reporting items for systematic reviews and meta-analysis extension for scoping reviews (PRISMA- ScR) procedures, albeit slightly modified to take into consideration the broad nature of the review (Shamseer et al., 2015). This review was carried out in eight stages: identification of sources; development of search terms; selection of sources; charting of retrieved data; definition of data items; critical appraisal of categories in relation to evidence; collating results; and provision of summaries for main findings for various categories.
2.1. Sources
Three reference databases were searched for literature published between 2005 and 2020: PubMed, EMBASE, and PubMed Central (PMC). The Google Scholar search engine was used for preliminary literature search. References of articles with broad content were scanned to identify if any useful papers were missed. Articles were excluded from the main review if the compounds they describe had no specificity for a known pathway in beta coronavirus pathogenesis or known efficacy evidenced by clinical trials. Titles and abstracts were independently reviewed by two authors (SP and BNM). Articles identified to be representative of the inclusion criteria were subjected to a full-text independent review by all the authors.
2.2 Search Terms
The broad nature of the review and the fact that much of the data on COVID-19 is not yet supported by strong scientific evidence was taken into consideration when drafting a search strategy. The search terms developed reflected the large diversity of possible compounds with anti-SARS-CoV-2 activity. Broad and specific terms were used in the search, noting that some formulations exert their therapeutic function in a more holistic way, while others utilize a more specific targeted approach. The resultant key term search strategy used the following combination of words “Therapeutic remedies for COVID-9”, “Herbal remedies for coronaviruses”, “Traditional Medicine for coronaviruses”, “Immunotherapy in COVID-9”, “Inhibitor of SARS-CoV”, “Inhibitor of SARS-CoV, MERS-CoV Protein”, “Inhibitor of SARS-CoV, MERS-CoV Replication”, “and Antioxidants against coronaviruses/viruses”, “protease inhibition in coronavirus replication cycle”. The terms “dietary”, “pharmacologic”, and “herbal” were selected to classify agents as either dietary supplemented, medically prescribed, or administered as herbal remedies. The term “herbal remedies” was taken to refer to non-specific, holistic, and broad-based remedies. Advanced age is highlighted as a major risk for severe symptoms and adverse outcomes on COVID and, therefore, the keyword “elderly” was used combined with other relevant keywords to help identify factors that enhance the risk for the aged. Table 1 summarizes the PubMed search strategy. Similar or slightly varied versions were employed for the other two databases. Duplicate references were filtered out during searches in subsequent databases. Articles were also filtered in relation to accessibility (abstract or full article access), and research design. Only English-language articles were retained for the review.
Table 1: PubMed Search Strategy
|
Tier 1 Keywords: COVID-19, SARS-CoV-2, Beta coronavirus, SARS-CoV, MERS-CoV, Diabetes, Hypertension, Cardiovascular Disease, and Cancer, oxidative stress, Tier 2 Keywords: Therapeutic, prevention inhibitors, treatment, antiviral, pharmacologic, immune system, anti-inflammatory Tier 3 Keywords: Agent, compound, extract, traditional medicine, antioxidant, vitamin, supplements, protease, drugs, herbal formulation Tier 4 keywords: Old age/elderly (expressly considered due to the high number of adverse outcomes in elderly COVID-19 patients). *Keywords in the different tiers were combined and searched in the PubMed Database. The results yielded in the preliminary searches helped identify specific compounds and further refinement of the search terms. For instance, a search for “beta coronaviruses protease inhibitors”, yielded broad results, which included zoonotic, human, numerous target sites for both human and viral proteases. The refinement of the search terms, in consideration with preliminary COVID-19 findings summarized in the background section, led to the finding of serine and cysteine protease inhibitors that might be effective in in inhibiting SARS-CoV-2 entry and establishment. *Sample findings below |
|
|
PubMed Search Terms and Results Sample |
|
|
Data Item |
Total Number of Articles |
|
Vitamin C |
(Vitamin C +COVID-19 =14, Vitamin C + SARS-CoV-2 =5, vitamin C+ Diabetes = 2,161, Vitamin C + cardiovascular disease = 4,772, vitamin C + hypertension = 869, Vitamin C+ oxidative stress = 7,997, Vitamin C+ antiviral = 945, Vitamin C+ immune system 2,791, Vitamin C + anti-inflammatory = 3,079). Total = 21,764 (Before filtering on the basis of described exclusion criteria). |
2.3 Selection of Sources
The etiological agent responsible for COVID-19 is SARS-CoV-2, a novel virus that is not yet well understood. Therefore, for the purpose of ameliorative intervention in COVID-19, the data sought was mainly based on comparable findings in closely related pathogenesis, preliminary COVID-19 findings, disseminated clinical data, and the hypothesized roles of coexisting conditions. Due to the nature of the mentioned limitations, a modification in the source selection criteria was done. News articles, editorials, newsletters, or magazine articles were found to be irrelevant and rejected. Letters were included on the basis of the level of evidence or sources provided. Subsequent abstracts were retrieved and subjected to further assessment on the basis of the following criteria:
-
Does the article provide evidence on a formulation, compound, or chemical that treats, helps manage, or prevents COVID-19, specific symptom of COVID-19, or comparable effect in closely related viral infections?
-
Does the article provide evidence on a formulation, compound or chemical that minimizes the risk of adverse outcome in COVID- 19 by modifying Is the risk attributable to coexisting illness?
-
Does the article describe a formulation, compound, or chemical that has been tried clinically and shown to be efficacious against COVID-19, even if the specific mechanism of action is still unknown?
-
Does the article describe a formulation, compound, or chemical that improves immune function in a manner that might be beneficial for the prevention, treatment, and management of COVID-19?
2.4 Charting Data
For articles found to be eligible for inclusion in this review, data related to the compound with a hypothesized curative or preventive property against SARS-CoV-2 was extracted by the lead author (SP) and reviewed by all contributing authors. Data extracted from the numerous eligible studies were entered into records and synthesized in summary format. A systematic approach to data charting was developed by authors, utilizing Microsoft Excel sheets that were calibrated and tested by authors. Charting used the three broad categories (herbal, pharmacologic, and herbal), which were then subdivided based on the mode of action, sources, chemical classification, and origin. The PRISMA flow diagram below represents the charting process utilized in the present study. Studies in each of the specific categories described were subjected to the PRISMA review process (diagrammatically represented in the results section).
2.5 List and Definition of Data Items
The broad nature of the review had an implication on the multiplicity of the items for which data was sought. Data items were broadly categorized into dietary supplements, pharmacologic drugs, and herbal remedies. The broad categorization was split into smaller descriptive categories that were used to classify and define the various agents, compounds, or formulations included in the review.
2.5.1 Dietary Supplements
A dietary supplement as defined by Congress as a product taken by mouth and which contains a “dietary ingredient” that is intended to supplement what is consumed through the diet, and which may include vitamins, minerals, herbs or other botanicals, amino acids, and substances such as enzymes, organ tissues, glandular, and metabolites (Graham et al., 2008). Between 69 % and 78 % of US adults take dietary supplements on a regular basis (CRN 2020). Supplements can be consumed as concentrates of extracts found in various forms, including tablets, capsules, powders, liquids, soft gels, or gelcaps. Dietary supplements included in the present review include the following:
-
Antioxidants
Antioxidants are generally described as substances that remove oxidizing agents and free radicals that can potentially cause harm to live organisms. Some vitamins may function as antioxidants, but for the purpose of this review, such will be classified under vitamins. Antioxidants included in the present review include the following: glutathione, flavonoids,
-
Vitamins
Vitamins are generally described as natural substances that are required in small quantities, often obtained from food, and necessary for good growth and good health. Vitamins included in the present review include the following: vitamin C, vitamin D.
-
Minerals
The term can have many different meanings. In the dietary context, minerals are generally described as a chemical required as a non- essential nutrient by an organism to perform key functions required to sustain life. Minerals included in the present review include the following: Zinc, Magnesium, and Selenium.
-
Humic Substances
Humic substances can be described as the endpoints of organic degradation, basically describing what is left following microbial decomposition of organisms and dead plant matter, but remain highly concentrated in minerals, trace minerals, amino acids, and fatty acids. They act as free radical scavengers, enhance the transport of nutrients, and help to facilitate oxygen transfer to the cells. Humic substances fall under three main groups, including humin, humic acid, and fulvic acid.
2.5.2 Pharmacologic Compounds
For the purpose of the present review, pharmacologic compounds include approved or investigational compounds with known mechanism and target, and which are administered for prevention, treatment, or management of COVID-19 and associated conditions. Pharmacologic compounds included in the present review include the following.
-
Antivirals
Antivirals are drugs, compounds, or products that exhibit the ability to kill or suppress viruses. Both synthetic and natural compounds can exhibit antiviral activity. Antivirals included in the review include the following: Cathepsin inhibitors, anti-inflammatory drugs, antivirals, JAK inhibitors, antimalarials, antibiotics, immunoglobulins, and humanized antibodies.
Antimalarial drugs
Antimalarial drugs are drugs used in the treatment of malaria. Antimalarial drugs that are currently being tested for COVID-19 treatment include the following: Chloroquine or Chloroquine phosphate, hydroxychloroquine.
Antibiotics
Antibiotics are antimicrobial substances that are active against bacteria, typically used to treat bacterial infections. Azithromycin is the only antibiotic currently used in the treatment of COVID-19.
Anti-inflammatory Drugs
In relation to COVID-19, anti-inflammatory drugs intended for the inhibition of excessive immune reaction by limiting the induction of various cytokines, such as Interleukin-6 (IL-6), and interferon-alpha (IFN-α). Currently, JAK inhibitors are the only anti-inflammatory drugs used in the prevention of hyper-inflammation in COVID-19. The JAK inhibitors to be reviewed in the present paper include baraticitinib, tofacitinib, fedratinib, and ruxolitinib.
Probiotics
Probiotics are live microorganisms that confer health benefits to the host when administered in appropriate amounts. Probiotics may play a role in immune modulation, work as anti-inflammatory agents, and produce inhibitory metabolites that work as antivirals. Probiotics to be included in the review include lactic acid bacteria, Lactobacillus, and Pediococcus.
Immunoglobulins/Humanized antibodies
In immunology, Immunoglobulins refers to antibodies or Y-shaped proteins that are used to neutralize pathogens, and often include IgG, IgA, IgM, and IgE. Traditionally, Immunoglobulins are administered as convalescent sera, which involve harvesting serum from individuals that have been exposed and healed from the disease to individuals that are yet to be exposed to the disease to transfer neutralizing antibodies. At the time of this writing, no convalescent serum is currently indicated for COVID-19, but the area provides a probable interventional strategy that may need to be investigated if other interventions do not yield effective treatments. Humanized antibodies can be described as antibodies (usually monoclonal) for non-human species that have their protein sequences altered to confer similarities with antibody variants that are naturally produced by humans. Humanized monoclonal antibodies to be reviewed in the present study include tocilizumab an antibody against (IL-6 receptor), and leronlimab (chemokine receptor 5 antagonist).
Nitric Oxide (Methylprednisolone)
Nitric oxide (NO) is a gas approved for the treatment of pulmonary hypertension in newborns suffering from hypoxic respiratory failure. The recommended use of NO in adults with acute respiratory distress syndrome (ARDS) is the basis of its inclusion in the review as a probable COVID-19 treatment for patients indicating with ARDS.
2.5.3 Herbal extracts/Traditional Medicines
Traditional Chinese Medicine
The WHO defines traditional herbal medicines as naturally occurring, plant-derived substances that have been subjected to minimal or no industrial processing and which have been utilized in local or regional healing practices. Traditional Herbal Medicines and extracts to be included in the present review are Chinese Traditional Medicine (TCM).
3.0 Results
Following a scoping methodology, a total of 105,062 articles for all the compounds and formulations investigated, the majority of the articles were excluded after finding that their titles did not relate to the present study, with more studies excluded on the basis of accessibility to the full article, research design, and duplication of the study area (preference is given to most recent studies and systematic reviews). A total of 203 articles were selected for inclusion in the review, and involved various designs, including clinical trials, systematic reviews, scoping reviews, and meta- analysis. The results were organized into categories in relation to the broad definitions of data items. The flow diagram provides a summary of the synthesis of the results.
Figure 2: PRISMA 2009 Flow Diagram for all papers reviewed
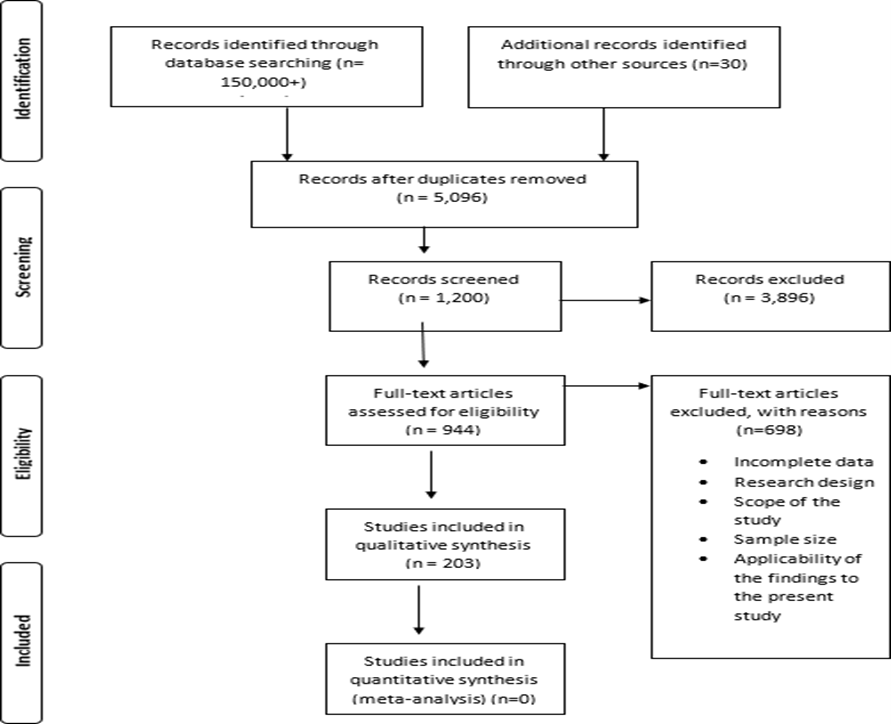
Thematic analysis of the numerous studies included in the review generally show that many drugs, compounds, extracts,and formulations can potentially help prevent, slowdown, manage, or avert adverse outcomes associated with COVID-19. Evaluated studies anticipate that increased utilization of these agents, supported by the recommended changes in social behaviours may help reduce the rate of symptomatic cases and adverse outcomes in COVID-19.
Table: Evidence Summary
|
Category |
Properties of interest |
Number of Studies(n) |
Research Design |
Key Findings |
|
Dietary Supplements |
||||
|
Vitamin C |
Antioxidant, Immune modulator, Antiviral |
11 |
RCTs (n=5), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=4), Scoping Reviews (n=1) |
Evaluated sources indicate that Vitamin C is a strong antioxidant, and its supplementation in COVID -19 may enhance immune response and reduce potential negative role of ROS. Vitamin C may also enhance immune response to viruses or be directly involved in the inhibition of viral infections. |
|
Vitamin D |
Antioxidant, Immune modulator, Anti-inflammatory, antiviral |
11 |
RCTs (n=2), Clinical Trials (n=0), Meta-Analysis (n=1), Systematic Reviews (n=6), Scoping Review (n=2) |
Evaluated studies provide evidence that Vitamin D could play a key role in boosting mucosal defenses against SARS-CoV-2 as it generally protects against respiratory infections, may also help alleviate the inflammatory response associated with severe COVID-19. More studies required to confirm the effect |
|
Zinc |
Antioxidant, Anti-inflammatory, Antiviral |
16 |
RCTs (n=10), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=6), Scoping Review (n=1) |
Studies provide strong evidence on the roles of zinc as antioxidant and how its deficiency leads to oxidative stress. Zinc may exert anti-inflammatory and antiviral effects through antioxidant pathways. It is also believed to improve the efficacy of hydroxychloroquine, when supplemented during treatment with hydroxychloroquine. More RCTs are required to identify impacts of zinc deficiency or supplementation in COVID-19. |
|
Magnesium |
No direct relation to major variables (Anti-inflammatory, antioxidant, antiviral) but important in CVD, Hypertension, and Diabetes |
9 |
RCTs (n=1), Clinical Trials (n=0), Clinical Trials (n=0), Meta-Analysis (n=1), Systematic Reviews (n=7), Scoping Review (n=0) |
The reviewed studies reveal that magnesium deficiency is common in people that heavily depend on modern processed foods, and supplementation is important for protection against CVD, Hypertension, and Type 2 diabetes and, therefore, important for protection against severe COVID-19 |
|
Selenium |
Antioxidant, Immune modulator, synergistic role in antiviral therapy |
11 |
RCTs (n=5), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=5), Scoping Review (n=1) |
The evidence reviewed shows that selenium is an antioxidant, with effects channeled through glutathione peroxidases. Selenium deficiency plays a role in viral pathogenesis, and hence supplementation improves the ability for antiviral therapy to prevent infection. High levels of serum selenium concentration is however associated with diabetes in both adults and children. |
|
Glutathione |
Antioxidant, Ant-inflammatory, Immune modulator |
16 |
RCTs (n=8), Clinical Trials (n=0), Meta-Analysis (n=), Systematic Reviews (n=9), Scoping Review (n=) |
The reviewed studies provide strong and detailed evidence on the roles of glutathione as an antioxidant. Glutathione plays a major role in the neutralization of toxic ROS. Adequate glutathione levels are necessary for optimal immune function, including cytokine production and effector T-cell function. Glutathione deficiency is also implicated in hypertension, diabetes, old age. Supplementation is optimized using N Acetyl Cysteine, a glutathione precursor. |
|
Plant Extracts |
||||
|
Curcumin |
Anti-inflammatory, antioxidant, Antiviral,
|
9 |
RCTs (n=5), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=3), Scoping Review (n=0) |
The studies provide strong evidence on the anti-inflammatory, antioxidant, and treatment of diabetes disorders, treatment of hypertension, reduction of CVD risk, and antiviral properties against Hepatitis and HSV-1. Potential use in COVID-19 requires more investigation |
|
Oil of Oregano |
Anti-inflammatory, antioxidant, antiviral, |
8 |
RCTs (n=6), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=2), Scoping Review (n=0) |
The studies reviewed provide strong evidence on antioxidant properties of the oil of Oregano, which are may explain why the essential oil is effective against inflammation, hyperglycemia, and high blood pressure. The oil also exhibits antiviral effects against several viruses, including HHV-1, HHV-1, BoHV-1, BoHV-2, HRSV, BVDV, and Rotavirus. |
|
Olive leaf Extract |
Antioxidant, Anti-inflammatory, and Antiviral. |
4 |
RCTs (n=2), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=2), Scoping Review (n=0) |
The studies evaluated show that secoiridoid Ole, the major biophenol constituent of olive leaf extract has ant-inflammatory, antioxidant, and antiviral effects. Ole has been shown to demonstrate antiviral activities against herpes mononucleosis, Hepatitis virus, Rotavirus, Bovine rhinovirus, Canine Parvovirus, Feline leukemia virus, Respiratory syncytial virus, and Parainfluenza type 3 virus. |
|
Fenugreek Seeds |
Antioxidant, anti-hypertensive, ant-hyperglycemic |
7 |
RCTs (n=5), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=2), Scoping Review (n=0) |
The studies reviewed provide strong evidence that fenugreek seeds extracts, particularly Trigonella, possess strong antioxidant properties and can potentially protect against diabetes, high blood pressure, and CVD. |
|
Flavonoids |
Anti-inflammatory, antioxidant, and antiviral, ACE inhibitor |
8 |
RCTs (n=5), Clinical Trials (n=0), Meta-Analysis (n=1), Systematic Reviews (n=1), Scoping Review (n=1) |
Evidence from the reviewed studies show that flavonoids exhibit antioxidant properties through the ability to capture superoxide, hydroxyl, and lipid radicals; anti-inflammatory properties through the ability to reduce macrophage proliferation; direct antiviral activities against various viruses, including Hepatitis B, enteroviruses, Influenza A and B viruses; and protection against hypertension, CVD, and diabetes. |
|
Echinacea |
Anti-inflammatory, Antiviral, Antioxidant |
7 |
RCTs (n=5), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=2), Scoping Review (n=0) |
The reviewed sources indicate that Echinacea has strong anti-inflammatory, antioxidant, and antiviral effects. E. purpurea root exhibits potent water-soluble antiviral ingredient against HSV-1 and influenza virus. The evidence also shows that E. Purpurea root extract also inhibits inflammatory cytokines secreted in upper respiratory infections and, hence, might be effective against COVID-19. Evidence also shows that Echinacea purpurea flower extract possesses antidiabetic and antihypertensive properties through the ability for its caffeic acid derivatives to inhibit ACE, a-amylase, and a-glucosidase activities. |
|
Soil Humus |
||||
|
Humic Substances |
Antioxidant, Anti-inflammatory, antiviral, immunomodulation |
4 |
RCTs (n=2), Clinical Trials (n=0), Meta-Analysis (n=0), Systematic Reviews (n=2), Scoping Review (n=0) |
Evaluated studies show that humic substances have antioxidant, anti-inflammatory, antiviral, and immunomodulation. According to the sources, humic substances can inhibit both enveloped and naked viruses, including Coxsackie A9 virus, Influenza A virus, Herpes simplex virus type 1 (HSV-1), and HIV viruses. |
|
Microorganisms |
||||
|
Probiotics |
Anti-inflammatory, immunomodulation, Antiviral |
6 |
RCTs (n=0), Clinical Trials (n=0), Meta-Analysis (n=3), Systematic Reviews (n=3), Scoping Review (n=0) |
The reviewed studies show that probiotics play a role in immunomodulation, antioxidant, and inhibition of certain viruses through direct interaction, production of antiviral inhibitory metabolites, and stimulation of the immune system and this includes clear benefits for the respiratory tract. |
|
Pharmacologic Treatments |
|
|||
|
Anti-hypoxic Nitric Oxide (Methylprednisolone) |
Treatment of hypoxia in COVID-related ARDS |
4 |
RCTs (n=1), Clinical Trials (n=3) Meta-Analysis (n=0), Systematic Reviews (n=1), Scoping Review (n=0) |
Evidence shows that Nitric Oxide may be used for the treatment of hypoxic respiratory failure, which is seen in COVID-19. Several clinical trials are currently underway to confirm the effectiveness of nitric oxide in the treatment of hypoxia in COVID-19 |
|
Antimalarials (Chloroquine or chloroquine phosphate, and hydroxychloroquine [HCQ]) |
Limiting pneumonia and general COVID-19 disease progression. |
11 |
RCTs (n=2), Clinical Trials (n=8) Meta-Analysis (n=0), Systematic Reviews (n=1), Scoping Review (n=0) |
Evidence from evaluated studies show that HCQ may be effective in the treatment of pneumonia and shortening of disease progression. For the effects to be achieved, HCQ should be used early in the infection, and coupled with azithromycin and zinc supplementation. Further trials are required to confirm above benefits due to mixed findings based recent data. |
|
Antibiotics (Azithromycin) |
Enhanced COVID-19 treatment when combined with hydroxychloroquine |
N=5 |
RCTs (n=4), Clinical Trials (n=0), Meta-Analysis (n=2), Systematic Reviews (n=0), Scoping Review (n=0) |
More trials required to determine usefulness in COVID-19 therapy. |
|
Antivirals |
||||
|
Remdesivir |
Inhibition of SARS-CoV-2 replication |
4 |
RCTs (n=1), Clinical Trials (n=2) Meta-Analysis (n=0), Systematic Reviews (n=1), Scoping Review (n=0) |
Evidence from the evaluated preliminary studies show that Remdesivir, a broad-spectrum nucleoside analog, facilitates a quick resolution in COVID-19 symptoms following intravenous administration. More studies are required to confirm the effects of Remdesivir. |
|
IFN-α |
Inflammation signaling |
5 |
RCTs (n=2), Clinical Trials (n=2) Meta-Analysis (n=0), Systematic Reviews (n=), Scoping Review (n=1) |
Evidence shows that IFN-α treatment may exert a synergistic effect when used with antivirals such as ribavirin. Clinical trials on the effectiveness of IFN-α are still ongoing. |
|
NHC(β-d-N4-hydroxycytidine) |
Inhibition of SARS-CoV-2 replication |
3 |
RCTs (n=2), Clinical Trials (n=1), Meta-Analysis (n=0), Systematic Reviews (n=0), Scoping Review (n=0) |
The reviewed studies provide evidence that NHC stops viral replication and improves respiratory function in COVID-19, though more studies are required to confirm the effect. |
|
Favipiravir (Avigan) |
Inhibition of SARS-CoV-2 replication |
5 |
RCTs (n=1), Clinical Trials (n=3), Meta-Analysis (n=0), Systematic Reviews (n=0), Scoping Review (n=1) |
Reviewed studies show that favipiravir may alleviate pyrexia, cough, and ARDS in COVID-19, though testing is not conclusive. |
|
lopinavir/ritonavir, |
Inhibition of SARS-CoV-2 replication |
3 |
RCTs (n=1), Clinical Trials (n=1), Meta-Analysis (n=0), Systematic Reviews (n=0), Scoping Review (n=1) |
Reviewed studies show that lopinavir/ritonavir may not beneficial in the treatment of COVID-19, though more studies are required to confirm whether synergistic effect can be achieved when combined with ribavirin. |
|
Ribavirin |
Inhibition of SARS-CoV-2 replication |
3 |
RCTs (n=0), Clinical Trials (n=1), Meta-Analysis (n=0), Systematic Reviews (n=1), Scoping Review (n=1) |
Reviewed studies show that ribavirin may be beneficial in the treatment of COVID-19, though more studies are required to confirm whether synergistic effect can be achieved when combined with lopinavir/ritonavir. |
|
JAK Inhibitors |
||||
|
(Baricitinib, Fedratinib, Ruxolitinib, Tofacitinib) |
JAK inhibition/inhibition of hyper-inflammation |
12 |
RCTs (n=2), Clinical Trials (n=6), Meta-Analysis (n=0), Systematic Reviews (n=2), Scoping Review (n=2) |
Reviewed studies provide evidence on the potential for JAK inhibitors to inhibit various JAK inflammation pathways and, hence facilitate the prevention of hyper-inflammation and cytokine storm. All the reviewed drugs show promising results and more studies are currently underway to confirm the effectiveness of specific JAK inhibitors against COVID-19 ARDS. |
|
Cathepsin Inhibitors |
||||
|
(gallinamide A/Symplostatin 4; the miraziridine A; leupeptrin; teicoplanin) |
Blocking of SARS-CoV-2 infection through inhibition of viral endocytosis |
10 |
RCTs (n=5), Clinical Trials (n=2), Meta-Analysis (n=0), Systematic Reviews (n=2), Scoping Review (n=1) |
Evidence from the reviewed studies show that cathepsin inhibitors may block the enzymatic cleavages that take place during the infection of ACE2-expressing cells in COVID-19. While no studies have been carried out to evaluate the effect of cathepsin inhibitors in COVID-19, there is potential for the inhibitors to prevent against COVID-19 infection establishment. Clinical trials should be carried out to establish the effectiveness of cathepsin inhibitors in preventing COVID-19. |
|
Adjuvant or Humanized Antibodies |
||||
|
(Tocilizumab, Leronlimab) |
Inhibition of pro-inflammatory cytokines |
11 |
RCTs (n=1), Clinical Trials (n=7), Meta-Analysis (n=0), Systematic Reviews (n=4), Scoping Review (n=0) |
Reviewed evidence on humanized antibodies use in COVID-19 shows potential to achieve improvement in symptoms, and reduced risk of respiratory failure and respiratory failure. Treatment with Leronlimab preliminarily showed reductions in levels of IL-6 and plasma viremia. More studies are required to confirm effectiveness of humanized antibodies in COVID-19. |
|
Convalescent Sera |
||||
|
Immunoglobulins |
Immune Induction |
6 |
RCTs (n=1), Clinical Trials (n=1), Meta-Analysis (n=0), Systematic Reviews (n=2), Scoping Review (n=2) |
Evidence from the studies reviewed show that convalescent sera have previously been used to stem outbreaks. Convalescent sera may be effective for people with low immunity where provides immediate immune defense and may be associated with low mortality rates. Its use is however limited due to challenges such as dosing, difficulty in analysis of protein composition, and possible contamination. |
|
Herbal/Traditional Medicine |
|
|||
|
Traditional Chinese Medicine (TCM) |
Treatment of COVID-19 |
4 |
RCTs (n=1), Clinical Trials (n=2), Meta-Analysis (n=0), Systematic Reviews (n=1), Scoping Review (n=0) |
The evidence reviewed show that traditional Chinese medicine may be effective in the treatment of COVID-19. While research on effectiveness of TCM is relatively high(including animal experiments, in vitro cells, and data mining) evidence on effectiveness in COVID-19 is generally limited. |
Collating, Summarizing, and Reporting of Results
The collation, summarizing, and reporting of data were conducted using information organized on the data charting forms. The exercise facilitated approximation of the protective capacity of specific dietary supplements, pharmacologic drugs, and herbal medicines against COVID-19.
Findings on Approximate Role of Dietary Supplementation and COVID-19
Vitamin C Deficiency and Supplementation
Vitamin C also referred to as L-ascorbic acid, is important for various physiological roles – is an immune enhancer, enzymatic co- factor for physiological reactions (such as hormone production), and as an essential antioxidant (Padayatty et al., 2003; Boyera, Galey, & Bernard, 1998; Wintergerst, Maggini, & Homig, 2006). An optimum basal vitamin C concentration is necessary for normal host defense response and vitamin supplementation, or pharmacological application is known to enhance the function of the immune system (Heuser & Vojdani, 1997). Cellular and humoral immune responses are reduced in vitamin C deficiency (Mousavi, Bereswill, & Heimesaat, 2019; Wintergerst, Maggini, & Homig, 2006). Clinical studies show that the activities of natural killer cells, chemotaxis, and lymphocyte cell proliferation is enhanced and promoted following vitamin C treatment in healthy subjects (Heuser & Vojdani, 1997; Levy et al., 1996). Immune cells such as leukocytes have 10 to 100 times higher concentration of vitamin C than plasma levels, an increase that commonly occurs against the concentration gradient and thereby highlighting the critical immunological role of vitamin C (Mousavi, Bereswill, & Heimesaat, 2019; Strohle, Wolters, & Hahn, 2011). The concentration of Vitamin C in leukocytes and plasma declines rapidly during stress and infections (Wintergerst, Maggini, & Homig, 2006). The activity of cortisol, the stress hormone, utilizes and contributes to the depletion of vitamin C, which may account for the decline in the level of vitamin C in leukocytes and plasma during stress (Kodama, Kodama, & Murakami, 1994; Wintergerst, Maggini, & Homig, 2006). The antiviral activity of Vitamin C, particularly against the influenza virus, is well known (Kim et al., 2013). Evidence exists on the role of type 1 IFNs (IFN-α and –β) in the prevention of viral pathogenesis (Muller et al., 1994). Levels of IFN-α and –β are usually low in vitamin C insufficiency and adequate in vitamin C sufficiency, indicating that vitamin C plays an essential role in the anti-viral immune response that takes place in the early phase of virus infection (Kim et al., 2013). Vitamin C has specifically been demonstrated to inhibit the replication of herpes simplex virus type 1, poliovirus type 1, and influenza virus type A (Mousavi, Bereswill, & Heimesaat, 2019). As an antioxidant, vitamin C plays an essential role in limiting morbidity and mortality due to diseases caused or exacerbated by oxidative damage (Padayatty et al., 2003). Vitamin C maintains the redox integrity of cells and as a result confers protection against reactive oxygen species generated during inflammatory response and respiratory burst (Wintergerst, Maggini, & Homig, 2006). One of the pathways through which this is achieved through nuclear factor E2-related factor 2(Nrf2), a transcription factor associated with antioxidant response element (ARE), where vitamin C is shown to negatively correlate and dictate the levels of intracellular Nrf2 (Teskey et al., 2018). Noteworthy, the National Institute of Health (NIH) provides evidence-based guidelines on vitamin C intake, sources, deficiency, risks associated with inadequacy, and its role in health and various health conditions (National Institute of Health 2020).
Vitamin D Deficiency and Supplementation
Vitamin D, a fat-soluble vitamin that is mainly obtained through UV light-mediated process that takes place under the skin, may enhance defense against COVID-19 through several immune pathways. It is suggested that vitamin D deficiency may be key comorbidity with hypertension, cardiovascular disease, cerebrovascular disease, and many immune challenges that SARS-Cov-2 compromises to cause severe disease (Mantay, 2020). Vitamin D is widely known for its regulation of calcium and phosphate metabolism, and impacts on bone health, nonetheless, recent studies have pointed to a critical role in immunity and respiratory health (Pfeffer & Hawrylowicz, 2012). A meta-analysis of randomized controlled trials conducted by (Bergman et al., (2013) showed that daily supplementation of vitamin D was associated with a significant decrease in respiratory tract infections. In fact, there is strong evidence on the effect of vitamin D in the prevention/amelioration of both bacterial and viral respiratory tract infections (Charan et al., 2012; Martineau et al., 2017). Men who regularly supplement Vitamin D are likely to have higher levels of the biologically active form of vitamin D, 1, 25- dihydroxy vitamin D or 25(OH)D2 than those who do not use vitamin D supplements (Swanson et al., 2014). In vitro analysis showed that Vitamin D may not affect the replication of rhinovirus or respiratory syncytial virus (RSV) or influenza A virus, but they modulate the expression and secretion of type 1 interferon, chemokines (CXCL8 and CXCL10), as well as pro-inflammatory cytokines, such as TNF and IL-6 (Greiller & Martineau, 2015). Common colds increase oxidative stress, which activates monocytes and macrophages, causing enhanced production of both inflammatory cytokine IL-1α and the anti-inflammatory product IL- 1ra (Rondanelli et al., 2018). The protective role against common cold following vitamin D supplementation has been documented (Rondanelli et al., 2018). Regulatory T cells (Tregs), which includes three subsets (CD25, Foxp3 (+) Tregs, and IL-10 producing Tregs), play an important role in regulating potentially harmful immune responses (Shaik-Dasthagirisaheb et al., 2013). Vitamin D3 (cholecalciferol) modulates the immune system through an increased production of IL-10, as partly evidenced by an increased percentage of Tregs and IL-10 in patients with systemic sclerosis (SSc, also called scleroderma, an autoimmune disease) taking 25 (OH) D or cholecalciferol supplementation (Di Liberto et al., 2019). A link exists between low levels of vitamin D and the development of Epstein-Barr virus (EBV). Additionally, evidence of a cathelicidin (small, cationic, antimicrobial peptides found in humans, other mammals, birds, and fish) mediated response against Hepatitis B virus indicates a possible vitamin D anti-viral activity through human beta densin 2, cathelicidin, or possibly through the release of oxygen reactive species (Beard, Bearden, & Striker, 2011). Vitamin D deficiency may also predict an unfavorable response to antiviral treatment of recurrent hepatitis C treatment (Bitetto et al., 2011). Vitamin D modulates contraction, inflammation, and remodeling of tissue, and serum levels of vitamin D may be predictive of tissue function (Shaik-Dasthagirisaheb et al., 2013). The overall antiviral effect of vitamin D is the boosting of mucosal defenses in addition to the dampening of excessive inflammation (Pfeffer & Hawrylowicz, 2012). The NIH offers evidence-based guidelines on vitamin D intake, sources, deficiency, risks associated with inadequacy, role in health, and various health conditions (National Institute of Health 2020).
Zinc Deficiency and Supplementation
Zinc plays a significant role as a structural component in proteins, and plays an important role in numerous cellular functions, including cell proliferation, RNA and DNA synthesis, stabilization of cell structures/membrane, redox regulation, and apoptosis (Maywald, Wessels, & Rink, 2017). With levels between 2-4 g, Zinc is the second most abundant trace element in the human body, the following iron, but as opposed to iron, zinc cannot be stored in the body and must be taken daily through food to guarantee sufficient supply (Jarosz et al., 2017). Metallothioneins (MTs) are cysteine- rich proteins that bind to metal ions such as zinc and copper, with up to 20 % of intracellular zinc bound to MTs (Gammoh & Rink, 2017). Mild cellular oxidants readily oxidize MTs, which is accompanied by a concomitant release of zinc ions in a mechanism whereby a shift to more oxidizing conditions releases zinc, while a shift to a more reducing environment leads to its binding (Maret, 1995). The zinc ions rapidly released by MTs, play the key function of controlling oxidative stress and regulation of inflammatory cytokines (Gammoh & Rink, 2017). Repeated evidence has also shown that MTs themselves act as potent electrophilic scavengers and cytoprotective agents against inflammation and inflammatory injury, with the ability to capture a wide range of ROS, such as superoxide, hydroxyl radicals, hydrogen peroxide, and nitric acid (Kang et al., 2015; Jarosz et al., 2017). It has been proposed that Zinc may have an influence on every immunological event in both adaptive and innate responses (Bonaventura et al., 2015). The chemotaxis and phagocytosis Activities of polymorphonuclear cells (PMNs) are reduced during zinc deficiency, while zinc supplementation causes the opposite effect (Gammoh & Rink, 2017). The production and concentration of pro-inflammatory cytokines, such as IL-1β, IL-6, and tumor necrosis factor (TNF)-α, and oxidative stress increases in zinc deficiency, implying a role for zinc against the formation of free radicals and protection of biological structures from injury during the inflammatory process (Stefanidou et al. 2006; Chasapis et al. 2012; Gammoh & Rink, 2017). Zinc depletion influences the recognition of major histocompatibility complex (MHC) class I by NK cells and their lytic activity, which is some of the key known features of an induced antiviral state capable of stopping viral replication from taking place in all cells (Gammoh & Rink, 2017; Rondanelli et al., 2018). In cell culture, pyrithione has been shown to stimulate the uptake of Zn2+ within minutes through a mechanism that is understood in detail for picornaviruses (Krenn., 2009). (Te Velthuis et al., (2010) demonstrated that a combination of Zn2+ and pyrithione in low doses had the ability to inhibit SARS-CoV in cell culture. Evidence also exists on the antiviral activity of zinc against picornavirus, arenavirus, coxsackievirus, human immunodeficiency virus type 1, herpes simplex virus type 2, and influenza virus, among others (Krenn et al., 2009; Li et al., 2015; Schito et al., 2003; Antoine et al., 2012; Nasser et al., 1996). Zinc deficiency or impaired zinc utilization may cause oxidative stress associated with the exacerbation of various chronic diseases, including diabetes and CVD in which is exerted through effects on glutathione homeostasis, nitric oxide signaling, and nuclear factor kappa B– dependent cellular processes (Foster & Samman et al., 2010). In diabetes, increased oxidative and nitrosative (Reactive nitrogen species acting together with reactive oxygen species) damage and down-regulation of the expression of Nrf2 has been associated with zinc deficiency (Zhao et al., 2011). A study conducted using spontaneously hypertensive rats (SHR) also showed potential hypertension aggravation, alluding to a possible role of CU/ZN- superoxide dismutase (Sato et al., 2002). Notably, the NIH provides evidence-based guidelines on zinc intake, sources, deficiency, risks associated with inadequacy, and role in health and various health conditions (National Institute of Health 2020).
Glutathione Deficiency and Supplementation
Glutathione (γ-glutamyl-L-cysteinyl glycine, GSH) is the non- protein cell molecule with the largest abundance of all sulfhydryl groups and is essential for both direct (chemical) and enzymatic neutralization of toxic reactive oxygen species (ROS), specifically ensuring cellular protection against oxidants (Wu et al., 2004). Two cytosolic enzymes, gamma-glutamylcysteine and GSH synthetase, are involved in the subsequent synthesis of GSH from glutamate, cysteine, and glycine (Griffith, 1999). Reduced GSH is the most prevalent non-protein thiol in animal cells and is regarded as the most powerful intracellular antioxidant, playing a critical role in the detoxification of a variety of electrophilic compounds and peroxides through catalysis by glutathione-S-transferases (GST) (Fraternale et al., 2009). In an oxidative environment, two GSH molecules have their sulfur atoms donating one electron each, resulting in the conversion of GSH to glutathione disulfide (GSSG), which can be reduced back to the initial GSH molecule through the action of GSSG reductase (GR) (Giustarini et al., 2016). Though the level of GSH concentration in cells is high, an increase in GSH synthesis is part of the adaptive response to oxidative stress. Three pathways are involved in the synthesis, and include: the ability to reduce GSSG to GSH through the action of GSSG reductase; the second is the increased synthesis of new GSH through induction of glutamate- cysteine ligase (GCL), originally referred to as γ-glutamylcysteine synthetase; the third pathway is through increased levels of enzyme γ-glutamyl transpeptidase (GGT), which catalyzes the transfer of the γ-glutamyl moiety of GSH to amino acids (Pastori & Trippi, 1992; Kugelman et al., 1994). The transcription factor Nrf2 located on the promoter regions of various genes coding for antioxidant associated enzymes, binds to antioxidant response element (ARE) associated promoters during oxidative stress, causing the upregulation of antioxidant levels, such as GSH (Teskey et al., 2018). GSH deficiency may be attributed to a lower rate of synthesis and is associated with the increased rate of oxidant stress, in addition to elevated levels of plasma markers of oxidant damage (Sekhar et al., 2011). Progeria, a rare genetic condition, involves extreme glutathione deficiency and is characterized by accelerated aging (Yan et al., 1999). The cells of individuals suffering from progeria demonstrate only 50 percent of normal catalase activity and 30 percent of normal glutathione peroxidase activity. Catalase and glutathione peroxidase are two of the body’s four primary antioxidant enzymes (Yan et al., 1999). Approximately 10% - 15% of cellular GSH is located within the mitochondria, and abnormally low levels of GSH are found in cases where the electron transport chain in the mitochondria is dysfunctional (Enns et al., 2014). As a result, the depletion of GSH in the mitochondria leads to elevated levels of ROS, and a categorical depletion of ATP, which often results in the alteration of cellular apoptotic response in favor of necrosis (Garcia-Ruiz & Fernandez-Checa, 2007). Diminished GSH expression has been demonstrated as a common feature in senility and among numerous pathological conditions including some important to the present review, including hypertension, diabetes, CVD, cancer, HIV AIDS, stroke, tuberculosis, immune dysfunction, and aging (Robaczewska et al., 2016; Sekhar et al., 2011; Buijsse et al., 2012; Wu et al., 2004; Teskey et al.,2018). Increasing evidence points to the fact that intracellular GSH levels in antigen-presenting cells, including macrophages, have an influence on the Th1/Th2 cytokine response pattern, and that GSH depletion particularly inhibits Th1-associated cytokine production and/or favors responses associated with Th2 (Fraternale et al., 2006). Activated T-cells produce reactive oxygen species (ROS), which trigger GSH response required for buffing the rising ROS to prevent cellular damage, with GSH plays an important role in T cell effector functions through regulation of T cell metabolic activity (Mak et al., 2017). In hypertension, reduced levels of red blood cell decreased glutathione (RBC-GSH) and increased levels of oxidized glutathione (GSSG) is observed in hypertensive patients, causing an elevated ratio of oxidized to reduced glutathione (GSH) compared to controls (Robaczewska et al., 2016). Additionally, RBC-GSH has an inverse correlation with systolic blood pressure (Muda et al., 2003). In diabetes, a sustained hyperglycemic state associates with low cellular levels of the antioxidant GSH and its precursor amino acids cysteine and glycine, often causing tissue damage that is associated with oxidative stress (Memisogullari et al., 2003; Sekhar et al., 2011). New evidence has contributed to the understanding of the role of cysteine and glutathione in skeletal muscle wasting, and includes the following: the finding that cysteine level is primarily regulated by normal postabsorptive skeletal muscle protein catabolism; cysteine level itself is a physiological regulator of bodily cell mass and nitrogen balance; that various catabolic conditions (such as old age) have an impact on the cysteine- mediated regulatory circuit; and that disease-specific treatment (such as antiviral therapy for HIV) may be more effective when combined with cysteine supplementation (Droge & Holm, 1997). Generally, the balance between free radicals and antioxidants is essential for slowing down diseases and maintenance of health. Supplementation with natural antioxidants, such camel whey protein (CWP) and undenatured bovine whey protein (BWP) has become common since they are safe, effective, and inexpensive (Badr et al., 2017). Glutathione supplementation may particularly improve tissue changes associated with oxidative damage, although oral glutathione (GSH) supplementation is inefficient, as GSH is degraded by stomach acid. Whey protein supplementation is more effective, especially whey proteins which have not been denatured by high heat Pasteurization, which reduces the bioavailability of cysteine, an important glutathione precursor. Cystine is one of the rate-limiting factors, along with the mineral selenium, for glutathione production (Minich & Brown, 2019). N Acetyl Cysteine (NAC) is a glutathione precursor, but oral supplementation may be limited to 750 mg or less due to adverse events associated with higher doses (Mahmoudi et al., 2015). NAC is also administered intravenously (Mahmoudi et al., 2015). The effect of CWP on GSH levels has been reported in several studies, including: the finding by (Abdel- Aziem et al., (2011) reported that CWP supplementation in animals fed with an aflatoxin-contaminated diet led to a significant increase in GSH levels in comparison to those that were fed the aflatoxin- contaminated diet alone; (Ebaid et al., (2013) demonstrated that CWP suppresses oxidative stress by decreasing hepatic lipid peroxidation and increasing GSH levels through activation of glutathione-S-transferase; A study by (Sousa et al., (2012) showed that supplementation with dietary whey protein lessened several risk factors for metabolic disease, including inflammation, oxidative stress, and blood pressure.
According to (Sekhar et al. (2011), oral dietary supplementation with cysteine and glycine provided for 14 days in diabetic patients restored the fractional synthesis rates of GSH to those observed in nondiabetic control subjects. There are several forms of low-heat pasteurization whey proteins available on the US market, and these may be superior to other commercially available whey protein supplements produced from high-heat (160 degrees +) pasteurized milk sources (Patel, 2015). (Horowitz, Freeman, & Bruzzese, (2020), recently conducted a study to evaluate the efficacy of glutathione therapy in relieving dyspnea associated with COVID-19. The findings of the study showed that glutathione improved dyspnea within an hour of use in 2 patients with a history of Lyme and tick-borne co-infections (Horowitz, Freeman, & Bruzzese, 2020).
Selenium Deficiency and Effects on Immune Response Significant research has been devoted to the attempt to understand the optimal immune function of Selenium, an essential trace element for humans, plants, and microorganisms (Arthur, McKenzie, & Beckett, 2003). The four oxidation states in which selenium is available in nature, include selenite (a salt or ester of selenic acid), elemental selenium, selenate (the form required by organisms that need selenium as a micronutrient), and selenide (a chemical compound containing a selenium anion) in decreasing order of redox status. These undergo conversion into organic forms that are more bioavailable, mainly into two amino acids, selenocysteine, and selenomethionine (Mangiapane, Pessione, & Pessione, 2014). As discussed above, selenium is a rate-limiting precursor for the body’s production of glutathione (Richie Jr et al., 2011). The antioxidant effects of selenium are believed to be channelled through glutathione peroxidases (GPx) that are active in the extracellular space, cell cytosol, and cell membranes (particularly in the gastrointestinal tract) where they are responsible for the removal of hydrogen peroxide and lipid hydroperoxides, with the potential to impact immune processes (Arthur, McKenzie, & Beckett, 2003). The radical scavenging properties of selenium against lipid peroxidation has been found to play a protective role against CVD, though existing evidence does not support the use of selenium supplementation as a primary approach in the prevention of CVD (Lee, Moon, Chung, 2003; Rees et al., 2013). Evidence shows that selenium influences both adaptive and innate immune responses (Kiremidjian-Schumacher & Roy, 1998). In relation to the innate system, selenium deficiency impairs lymphocyte proliferation in response to mitogen, and leukotriene B4 synthesis, which is essential for neutrophil chemotaxis; in relation to the humoral system, various effects may be observed in selenium deficiency, including a decrease in IgM, IgG, and IgA in rats, and a decrease in IgG and IgM titters in humans (Arthur, McKenzie, & Beckett, 2003). Studies conducted on selenium-deficient mice show that neutrophils are able to ingest pathogens but not able to kill them, a defective immune function that has been associated with decreased neutrophil cytosolic GPx activity that allows free radicals produced in a respiratory burst to kill neutrophils, a problem that is corrected through high doses of selenium supplementation (Arthur, McKenzie, & Beckett, 2003). However, high levels of serum selenium are paradoxically associated with a higher prevalence of diabetes in children and adults (Gebre-Medhin et al., 1984; Laclaustra et al., 2009). However, Wang and co-workers found that the positive association between serum selenium levels and Type-2 Diabetes Mellitus (T2DM) existed in populations with both relatively low levels and high levels of serum selenium, indicating a likely U-shaped non-linear dose-response relationship between serum selenium and T2DM (Wang et al., 2015). It has also been demonstrated that the status of selenium in the body diminishes with increasing age in a manner independently associated with HDL- cholesterol levels (Lee, Moon, Chung, 2003). In vivo studies conducted in rat models show that the levels of very-low-density lipoprotein cholesterol (VLDL-Cho) may increase during vitamin E supplementation in selenium deficiency (Stone et al., 1994). Selenium deficiency has been shown to be an important factor in viral pathogenesis, often resulting in altered expression of chemokines and cytokines, which cause virulence through enhanced viral replication as seen in coxsackievirus, HIV, and hepatitis C virus (Beck, 2001). A study conducted by Li and co-workers showed that selenium nanoparticles (SeNPs) functionalized with the antiviral oseltamivir (OTV) enhanced the ability to prevent H1N1 infection and led to lower toxicity (Li et al., 2017).
Magnesium
Magnesium is an essential micronutrient in the human body, which is believed to play a role in approximately 80 % of known metabolic functions (Workinger, Doyle, & Bortiz, 2018). Key processes in which magnesium is involved in include protein synthesis, cellular energy production, and storage, DNA and RNA synthesis, and the stabilization of mitochondrial membranes (Newhouse & Finstad, 2000). Magnesium also plays an important role in the maintenance of muscle and nerve function, maintenance of normal heart rhythm, maintenance of normal blood pressure, bone integrity, and glucose and insulin metabolism (Volpe, 2013). While magnesium content is found to be high in foods such as whole grains; dark, green, and leafy vegetables; and white potatoes, intake is usually below recommendations (310-420 mg/d in adults) and often intake trends worsen as people age (Volpe, 2013). A low magnesium intake is observed in populations that have diets dominated by modern processed foods that include a high percentage of refined grains, fats, and sugars, such as is common in the US population (Rosanoff & Shapses, 2016; Dai et al. 2018). A link between dietary magnesium and various chronic diseases have been established, including CVD, hypertension, and type 2 diabetes mellitus (Workinger, Doyle, & Bortiz, 2018). It has been demonstrated that oral magnesium therapy provides beneficial effects of dietary magnesium in CVD, T2DM, and cancers, though findings from other studies show that a high calcium intake can cause the onset of low magnesium status and vice versa (Dai et al., 2018). Additional evidence-based data on magnesium functions in the body, dietary sources, supplementation, and dosage for different ages is available from the National Institute of Health (NIH 2020).
Olive leaf Extract
Leaves from the olive tree, Olea europaea, are rich in bisphenols (BPs), including oleuropein (Ole), verbascoside, tyrosol, ligstroside, and hydroxytyrosol, compounds that have demonstrated several biological activities, such as antioxidant, antimicrobial, antithrombotic, and even skin photo-protective properties (Micol et al., 2005). The secoiridoid Ole is the major BP of olive leaf ethanolic extract, often constituting between 20 and 25 % (w/w) of the total dry weight (Benavente-Garcia et al., 2001). Evidence indicates that ole possesses a wide range of health-promoting and pharmacologic properties, including antiarrhythmic, spasmolytic, immune-stimulant, cardioprotective, hypotensive, and anti-inflammatory effects (Al-Azzawie & Alhamdani, 2006). Research shows that ole has antiviral activities against herpes mononucleosis, hepatitis virus, rotavirus, bovine rhinovirus, canine parvovirus, and feline leukemia virus, respiratory syncytial virus, and parainfluenza type 3 virus (Micol et al., 2005). Ole can be hydrolyzed to produce other bioactive substances, including elenolic acid and 3, 4-dihydroxy-phenyl ethanol (hydroxytyrosol) (Al-Azzawie & Alhamdani, 2006). The antiviral, anti-inflammatory, and antioxidant properties of Olive leaf extracts, and particularly the secoiridoid Ole, suggest that the extract may be potentially effective against COVID-19 (Elfiky 2020). (Micol et al., (2005) demonstrated the ability for Ole to inhibit the in vitro infectivity of the viral haemorrhagic septicaemia (VHSV), with an average dosage of between 500 and 1000mg.
Fenugreek Seeds
Fenugreek (Trigonella foenum-graecum) is regarded as an important aromatic and spice crop with its dried seeds having a wide application in food, flavoring, medicine, and beverages. The seeds are used as a condiment in many parts of India, and as a supplement to wheat and maize flour in Yemen and Egypt, where they make a key constituent of daily diet (Pandey & Aswasthi, 2015). Fenugreek seeds contain L-tryptophan and lysine rich proteins, mucilaginous fiber, and rare compounds such as saponins, coumarin, sapogenins, and trigonelline, which are thought to account for the numerous therapeutic effects of fenugreek seeds, including inhibition of cholesterol absorption (Bhanger, Bukhari, & Memon, 2008). A study conducted by (Pandey & Aswasthi, (2015) showed that the antioxidant activity of extracts of soaked, germinated, and roasted fenugreek seed flours were 60.7 %, 73.9 %, and 32.0 %, whereas raw fenugreek flour exhibited 18.1 % antioxidant activity. (Dholi, Raparla, & Kannappan (2011), showed that fenugreek seeds exhibited a synergistic activity with neem leaf extracts against rat alloxan-induced diabetic model. (Zhou et al., (2012) also showed that trolling, a constituent of fenugreek seeds, had a therapeutic potential against diabetes and this effect is exerted through inhibition of erythrocyte membrane-bound sodium-potassium adenosine triphosphatase, as investigated by (Anuradha, Kaviarasan, & Vijayalakshmi (2003). Fenugreek is may also reduce the risk of CVD due to the hypoglycemic effects of trigonelline and 4-hydroxy isoleucine, in addition to the effects of its antioxidant properties (Kumar & Zandi, 2014; Chaturvedi et al., 2013). A study conducted by (Balaraman, Dangwal, & Mohan, (2006), showed that methanol extract (ME) of fenugreek seeds significantly reduced blood pressure in salt-induced methanol fraction (MF) in deoxycorticosterone acetate (DOCA) salt hypertensive rats.
Curcumin
Curcumin is the yellow or gold coloring of turmeric, which is derived from the Curcuma longa, a rhizomatous herbaceous perennial plant of the ginger family. Turmeric is commonly used as a spice in the Indian subcontinent and as part of traditional Chinese medicine (Aggarwal et al., 2007; Zhang., et al. 2013). Curcumin was first isolated centuries ago and its structure as a diferuloylmethane was determined in 1910 (Aggarwal et al., 2007). A comprehensive review conducted by (Zhang et al., (2013), reported on the positive effects of curcumin application for glycemia and diabetes-related liver disorders, adipocyte dysfunction, neuropathy, nephropathy, vascular diseases, pancreatic disorders, and other complications, as well as its antioxidant and anti- inflammatory properties. The anti-inflammatory properties of curcumin are mediated through the ability of curcumin to regulate inflammatory cytokines (Abe, Hashimoto, Horie, 1999). The same authors also reviewed studies that showed that supplementation of curcumin with vitamin C, yogurt, and in combination with bone marrow transplantation, reduced the levels of blood glucose, Hb, and HbA1C, findings that were based on streptozotocin rat diabetic models (Zhang et al., (2013). A study conducted by (Tapia et al., (2012) reported on the ability of curcumin to induce NrF2 nuclear translocation, prevent glomerular hypertension, hyper-infiltration, oxidant stress, and the decrease in antioxidant enzymes in 5/6 nephrectomized rats. The study provided evidence of the ability for curcumin to provide a protective effect against glomerular and systemic hypertension, prevention of renal injury associated with nuclear translocation of Nrf2, and the prevention of oxidant stress and the decrease in antioxidant enzymes (Tapia et al., 2012). In relation to CVD, evidence from in vivo rat studies shows that curcumin supplementation reduces the risk of CVD by correcting for the risk associated with atherogenic index (AI) and High Fat Diets (Kim & Kim, 2010; El-Habibi, Wakf, & Mogall, 2013). Curcumin has also been demonstrated to exhibit antiviral effects. A study conducted by Kim et al., (2020), demonstrated that Curcuma Longa Linn (CLL) extract suppressed HBV replication and transcription of HBV genes in HepG cells that produce HBV particles. (Zandi et al., (2010) showed that curcumin derivatives remarkably exhibited antiviral activities against HSV-1, with CC50 values for curcumin, gallium-curcumin and Cu-curcumin found to be 484.2 µg/mL, 255.8µg/mL and 326.6 µg/mL, respectively, and the respective IC50 values 33.0 µg/mL, 13.9 µg/mL and 23.1 µg/mL. The reviewed evidence shows that curcumin may play an important role in COVID-19 due to its anti-inflammatory, antioxidant, and preventive properties against key COVID-19 risk factors, including hypertension, diabetes, and CVD. Curcumin and its derivatives also exhibit antiviral activities and, hence, may potentially reduce COVID-19 viral loads.
Echinacea
Echinacea (Asteraceae) is a genus comprising of a small number of hardy perennial plant species that are native to parts of North America. Three species in the genus, including Echinacea angustigolia, Echinacea pallida and Echinacea purpurea are used for medicinal purposes, though recent studies have shown potential additional species (Binns et al. 2002; Hudson et al., 2006). Differences in phytochemical constituents responsible for medical conditions have been noted across different species and this typically includes alkamides, caffeic acid derivatives, polysaccharides, and alkenes (Barnes et al., 2005). Echinacea has long been used for its medicinal properties, is often indicated for a wide variety of conditions, including septic wounds, syphilis, blood poisoning, and snake bites (Barnes et al., 2005). Other studies show that plants in the Echinacea genus may be effective against additional conditions. (Mishima et al., (2004) showed that E. purpurea eliminates free radicals produced through irradiation due to its radical-scavenging effect, reduces cytotoxicity that is caused by lipid peroxides, suppresses the reduction in white blood cell count due to irradiation, and prevents impairment of immunity. (Binns et al., (2002) found that extracts of 8 taxa of the genus Echinacea had antiviral activity against HSV-1 when exposed to visible and UV-A light. A study conducted by (Hudson et al., (2008) sought to characterize antiviral activities in Echinacea root extracts, with a focus on the effects of E. purpurea., E. pallida. var. angustifolia., and E. pallida. var. pallida three viruses (rhinovirus, HSV-1, and influenza virus) associated with epithelial infections. The findings showed that E. purpurea root exhibited a potent water-soluble antiviral ingredient with the ability to inactivate HSV-1 and influenza virus, but not rhinovirus, E. pallida. var. Angustifolia. root contains a significant anti-rhinovirus activity, which was explained as a possible effect of the higher amount of alkamides; however, E. pallida. var. pallida did not exhibit any antiviral activity because it was devoid of the antiviral compounds (Hudson et al., 2005). A study conducted by (Sharma et al., (2009) established that standardized Echinacea had a potent ability to reverse the induction of multiple pro-inflammatory cytokines by respiratory viruses. On the basis of a background indicating the ability for viruses infecting the upper respiratory system to stimulate the secretion of pro-inflammatory cytokines in the absence of viral cytopathology, the authors evaluated the ability for E. Purpurea root extract to inhibit the induction of a number of cytokines, including IL-6 and IL-8, in line with the human epithelial cells by the following viruses: rhinoviruses 1A and 14, influenza virus, respiratory syncytial virus, adenovirus types 3 and 11, and herpes simplex virus type 1 (Sharma et al., 2009). Besides inhibiting the secretion of pro-inflammatory cytokines, the findings showed that Echinacea preparation had the ability to inhibit the growth of various respiratory viruses (Sharma et al., 2009). A study conducted by (Chiou et al., (2017) on the antioxidant, antidiabetic, and antihypertensive properties of Echinacea purpurea flower found that caffeic acid derivatives (CAD) showed good antioxidant properties, besides inhibiting a-amylase, a-glucosidase, and ACE activities in a concentration-dependent manner and, hence, the conclusion that CAD had a good potential for managing hyperglycemia and hypertension.
Humic Substances
In the past few years, a significant body of research has been dedicated to humic substances, natural substances that are usually part of soil humus, and which play an important role in living organisms. Humic substances have roles in the conversion of dead matter into nutrients, transfer of nutrients, and other roles within living organisms and, therefore, humic substances are used for both medical and agricultural purposes (Klocking & Helbig, 2005). Humic substances include humic acid, which is physiologically active in the form of salts or humates. A key feature of humic substances is the saturation of their molecules into diverse groups, including carboxyl, phenolic, alcoholic hydroxyls, quinoid groups, and methoxy, amino groups (Klocking & Helbig, 2005). Findings from studies conducted in the past decade show that humic substances have pharmacological applications. The scientific literature describes antioxidant, immunostimulatory, anti- inflammatory, and antiviral effects of humic substances (Winker & Ghosh, 2018). Studies have shown that humic substances can inhibit multiple viruses. Preliminary findings of early studies showed that humic substances had the ability to inhibit both enveloped and naked DNA viruses, including Coxsackie A9 virus, influenza A virus, and herpes simplex virus type 1 (HSV-1) viruses (Dewar & Thiel, 1977). Additional investigations conducted over the years have corroborated the findings on the ability for humic substances to selectively inhibit additional viruses, including HIV-1 and HIV-2, cytomegalovirus, and vaccinia viruses (Meerbach et al., 2001). A study conducted by (Zhernov (2018), showed that humic substances had the ability to interfere with multiple stages of the replication cycle of the HIV virus. The author conducted the evaluation using several humic substances, including humic, fulvic acid, and hymatomelanic acids. The findings of the study showed that humic and hymatomelanic acids showed distinct antiviral activity within the concentration range between 0.78 ug/mL and 100 ug/mL in HIV- 1, while much less activity was associated with fulvic acid (Zhernov, 2018). Additional findings showed that the tested humic substances had low cytotoxicity levels, making them suitable treatment agents in HIV-1. The findings show that humic substances may also possess antiviral activity, in addition to the identified anti- inflammatory activity, against beta coronaviruses and, hence, could potentially be used in COVID-19.
Flavonoids
Flavonoids are polyphenolic substances that are mainly found in the edible parts of plants, predominantly in fruits and vegetables. Flavonoids are responsible for the dark blue and red color of berries, as well as the orange and yellow colors of citrus fruits. Flavonoids that possess biological activity are referred to as bioflavonoids and have been shown to play the same roles as vitamins in the human body, including the ability to capture superoxide, hydroxyl, and lipid radicals (Brodowska, 2017). Flavonoids are divided into several groups and sub-groups based on biological and chemical properties, and these include flavonols, flavanones, flavonols, isoflavones, flavones, and anthocyanins. Flavonoids are also characterized based on their anti-inflammatory, anti-allergic, antiviral, anticarcinogenic, therapeutic, and cytotoxic properties (Brodowska, 2017). Several studies have investigated the biological and pharmacological activities of flavonoids in relation to their potential use for therapeutic purposes. (Comalada et al., (2006) investigated the inhibition of pro-inflammatory markers in primary bone marrow- derived mouse macrophages by naturally occurring flavonoids in various common groups (flavonols – quercetin and kaempferol; flavones—diosmetin, apigenin, chrysin, and luteolin; isoflavones— genistein and daidzein and flavanones—hesperetin). The findings of the study showed that most of the flavonoids evaluated were able to reduce macrophage proliferation induced by colony-stimulating factor (M-CSF), without affecting cellular viability. Additionally, (Comalada et al., (2006), showed that some flavonoids had the ability to inhibit TNFa production, iNOS expression and NO production in LPS-activated macrophages, an effect that has been associated with the inhibition of the NF-kB pathway. (Amoros et al., (1992) investigated the in vitro activity of flavonoids identified in propolis (flavones and flavonols) against herpes simplex virus type 1 (HSV-1), with the findings showing the activity of flavonols against HSV-1 to be more active than flavones. Further investigations showed that a combination of flavone and flavonol had higher efficacy as compared to individual compounds and, hence, explaining why the whole propolis extract was more efficacious (Amoros et al.,1992). Different flavonoids have also demonstrated antiviral activity against various viruses, including hepatitis B, enteroviruses, and influenza A and B viruses (Yang & Chen, 2008; Tait et al., 2006; Nagai et al., 1995). In relation to COVID-19 comorbidities, flavonoids have been found to provide several beneficial effects. A study conducted by (Kameda et al., (1987) demonstrated that four flavonoids (astragalin, kaempferol-3-0(2”-0- galloyl)-glucoside, isoquercitrin, and quercetin-3-0(2”-0-galloyl)- glucoside) isolated from the leaves of persimmon (Diospyros Kaki), traditionally used in the treatment of hypertensive diseases in Japan, inhibited angiotensin-converting enzyme activity in a dose- dependent fashion and, hence, exhibiting antihypertensive and cardio-protective effects. A meta-analysis conducted by (Liu et al., (2014) found that the consumption of dietary total flavonoids was associated with a diminished risk of type 2 diabetes.
Oil of Oregano
Oregano (Origanum vulgae L.) is an aromatic plant species that produces essential oils. Oregano essential oils contain phenolic compounds, such as carvacrol, that have been associated with significant biological effects, including anti-inflammatory, antioxidant, and antimicrobial properties (Silva et al., 2012). Studies show that carvacrol, a phenolic monoterpene, possesses significant pronounced antioxidant effect against free radicals generated in vitro and anti-nociceptive properties generated in vivo (Silva et al., 2012). A study conducted by (Han & Parker (2017) showed that oregano essential oils (OEO) significantly inhibited inflammatory biomarkers, including monocyte chemoattractant protein 1 (MCP-1), vascular cell adhesion molecule 1 (ICAM-1) interferon-inducible T- cell alpha chemoattractant (I-TAC), and monokine induced by gamma interferon (MIG, or CXCL-9). The findings of the study also showed that OEO had a significant modulating effect on global gene expression which is critical in inflammation (Han et al., 2017). (Gilling et al., (2014) investigated the efficacy and antiviral efficacy and mechanisms of action of the oregano essential oil and its primary component carvacrol against murine norovirus (MNV), with the findings showing carvacrol’s ability to inactivate MNV within 1 hour of exposure through direct action on the viral capsid, and subsequently, viral RNA. Studies also show that certain monoterpenes and oregano essential oils possess antiviral effects against HSV through the dissolution of the HSV envelope (Siddiqui et al.,1996). (Astani et al., (2010) demonstrated that pretreatment of HSV-1 with essential oils or monoterpenic compounds (alpha- terpinene, gamma-terpinene, alpha-pinene, p-cymene, terpinen-4-ol, alpha-terpineol, thymol, citral, and 1,8-cineole) led to a significant reduction in plaque formation, At maximum non-cytotoxic concentrations of the tested compounds infectivity was reduced by > 96 % for all essential oils as well as for three of the monoterpenes, α-terpinene, γ-terpinene and α-pinene (Astani et al.,2012). A study conducted by (Pilau et al., (2011) evaluated Mexican Oregano (Lippia graveolens) essential oils and its main compound carvacrol against human and animal DNA viruses, such as Human herpesvirus 1 (HHV-1), Acyclovir resistant virus HHV-1 (ACVR-HHV-1), Bovine alphaherpesvirus 1(BoHV-1), Bovine alphaherpesvirus 2 (BoHV-2), Bovine alphaherpesvirus 5 (BoHV-5), and RNA viruses, including Human orthopneumovirus (HRSV), Bovine viral diarrhea (BVDV), and Rotavirus (RV). The findings of the study showed that Mexican oregano essential oils were effective against HHV-1, BoHV-1, BoHV-5, HRSV, and RV, all of which are enveloped viruses (Pilau et al., 2011). Based on these findings there is a possibility that the oil of oregano plant may be effective against COVID-19. In relation to COVID-19 comorbidities, a study conducted by (Talpur et al., (2005) showed that a novel formulation of essential oils, including oil of oregano, cinnamon, cumin, and fenugreek enhanced insulin sensitivity and reduced in blood pressure (Talpur et al., 2005); and though not studied, oil of Oregano may protect against CVD, as it is one of the degenerative diseases in which ROS is involved (da Costa et al., 2012).
Probiotics
Probiotics are live microorganisms that, when administered in suitable amounts confer a health benefit on the host, including the gastrointestinal tract. While the benefit attained from probiotics was initially thought to only occur as a result of improvement in the intestinal microbial balance, there is now substantial evidence that probiotics may also play a role in immune modulation (Borchers et al., 2009). Most of the studies on the health promoting the effects of probiotics has been conducted in animal models. In these animal models, probiotic administration protects against chemically induced colitis by down-regulating inflammatory cytokines or promoting regulatory mechanisms specific to the probiotic strain (Gackowska et al.,2006; Morita et al., 2002). A review conducted by (Al Kassaa et al., (2014) reported that lactic acid bacteria (LAB) and their bacteriocins could be used as antiviral agents, where the antiviral effect may be exerted through direct probiotic and virus interaction, production of antiviral inhibitory metabolites, or by stimulation of the immune system. Another review conducted by on 33 clinical trials investigating probiotic use in respiratory virus infections showed that there were clear benefits for outcomes of respiratory tract infections as reported by 85 % (28/33) of the reviewed studies, including significant reductions in viral load. (Martin et al., (2010) established that heat-killed bacteria, most notably among breastmilk strains of Lactobacillus and Pedi coccus, were able to significantly inhibit R5-tropic HIV-1, pointing to the possible use of the probiotic in the mucosal protection against HIV-1 in the breastfeeding infant. Though evidence points to a general antiviral effect, there is a need for confirmatory studies with more specific viruses and a comparison of effects of various probiotic strains, and the mechanisms through which antiviral mechanism is elucidated. Such confirmatory studies may be useful in the treatment or protection against COVID-19.
Summary on Dietary Supplementation in COVID-19 The tabulated summary presents a condensed synthesis of various dietary supplements and their potential role in the prevention and treatment of COVID-19 or amelioration of the adverse role by COVID-19 in related comorbidities. The dietary supplementation summary is focused on the prevention of severe COVID-19 disease. Additional data on dietary sources supplemented products, and dosage is obtained from the National Institute of Health (NIH).
Table: Summary of Findings on Dietary Supplements in COVID-19
|
Dietary Supplement |
Relevant Properties |
Target |
Supplemented Product |
Sources (including dietary, plant, soil, microorganism) |
Approx. Daily Intake |
Use COVID-19 Prevention & Treatment |
Potential role in amelioration of COVID 19 Comorbidity effects |
Substitute (s) |
|
Vitamin C |
Antioxidant, Immune-modulator, antiviral. |
Enhanced levels of vitamin C in Leukocytes and plasma, enhanced immune function, and normal antioxidant function |
Ascorbic Acid, Sodium Ascorbate, calcium ascorbate, dehydroascorbate, calcium threonite, xylonite, and lyxonate. |
Citrus fruits, tomatoes, potatoes, red and green broccoli, strawberries, kiwifruit, and Brussels sprouts |
30-180 mg |
Should be supplemented for both prevention and treatment |
Reduction of high antioxidant levels associated with hypertension, CVD, and diabetes. In CVD, vitamin C may reduce monocyte adhesion to smooth muscles, reduce vascular muscle apoptosis and prevent plaque instability. |
None |
|
Vitamin D |
Antioxidant, Immune-modulator, antiviral |
Protection against COVID-19 infection establishment in respiratory tract, modulation of the expression of pro-inflammatory cytokines, specifically mediation of increased IL-10 production |
D2 (ergocalciferol), Vitamin D3 (cholecalciferol), may be gained from fortified foods. |
Fatty fish (such as mackerel, salmon, and tuna), fish liver oils, mushrooms, small amounts of vitamin D are found cheese, beef liver, and egg yolks. |
10-20 mcg |
Should be supplemented for both prevention and treatment |
Decrease respiratory infections (which are associated with adverse COVID-19 outcomes), reduce oxidative stress associated hypertension, CVD, and diabetes. |
None |
|
Zinc |
Antioxidant, Immune Modulator |
Capturing of ROS (such superoxide, hydroxyl radicals, hydrogen peroxide, and nitric acid), modulation of adaptive and innate immune responses. Stoppage of viral replication through enhanced recognition of major histocompatibility complex (MHC) |
Zinc gluconate, zinc sulfate, zinc picolinate, zinc orotate, zinc citrate, and zinc acetate. |
Oysters, red meat, poultry, beans, nuts, whole grains, crabs, and lobster. |
Dosage depends on type of supplement as each supplement contains different amount of Zinc. Recommended dosage is 15-30 mg of elemental Zinc. For instance, zinc sulfate contains 23% of elemental zinc, hence 220 mg of zinc sulfate contains 50mg of elemental zinc. |
Should be supplemented for treatment and prevention if deficiency is noted. |
Zinc deficiency worsens oxidative stress associated with hypertension, diabetes, and CVD. |
None |
|
Glutathione |
Antioxidant, Immune Modulator |
Cellular protection against ROS, effective Th1/Th2 cytokine response pattern, regulation of T cell effector functions and metabolic activity, improvement of cysteine-mediated regulatory circuit. |
Whey Protein, Cysteine, Glycine, glutamic acid, Omega 3 fatty acids |
Asparagus, Avocado, Banana, Broccoli, Carrot, Cauliflower, Cucumber, Green Beans, Green Squash, Mango, papaya, spinach, tomato |
750 mg for whey protein. |
Should be supplemented in old age and individuals affected with COVID-19 comorbidities |
Limitation of tissue damage associated with increased ROS in diabetes, |
None |
|
Selenium |
Antioxidant, Immune Modulator |
Removal of hydrogen peroxide and lipid hydroperoxides, precursor for glutathione production. |
Selenomethionine, multivitamin, sodium selenite, sodium selenite |
Brazil nuts, seafoods, organ meats, muscle meats, poultry, grains. |
. 300mcg |
Should be supplemented for treatment and prevention if deficiency is noted. |
Enhance immune activity against respiratory infections. |
None |
|
Magnesium |
Protection against CVD, Hypertension, and Diabetes |
Maintenance of muscle and nerve function, maintenance of normal heart rhythm, maintenance of normal blood pressure, bone integrity, and glucose and insulin metabolism |
Multivitamin mineral supplements, magnesium aspartate, magnesium citrate, magnesium lactate, magnesium chloride. |
Whole grains, dark green leafy vegetables, white potatoes |
65-350 mg |
Should be supplemented for treatment and prevention if deficiency is noted. |
Provides beneficial effect in all metabolic COVID-19 comorbidities through muscle and nerve function, maintenance of normal heart rhythm, maintenance of normal blood pressure, bone integrity, and glucose and insulin metabolism |
none |
|
Olive leaf Extract |
Antioxidant, Anti-inflammatory, and Antiviral |
antiarrhythmic, spasmolytic, immune stimulant, cardioprotective, hypotensive, and anti-inflammatory |
secoiridoid Ole, ethanolic extract, oleuropein, verbascoside, tyrosol, ligstroside, and hydroxytyrosol |
Olea europaea |
500-100 mg |
Should be supplemented for prevention. |
Benefits specific to COVID-19 comorbidities include antiarrhythmic, cardioprotective, hypotensive |
Oil of Oregano, Curcumin, Echinacea |
|
Oil of Oregano |
Antioxidant, Anti-inflammatory, antiviral |
Inhibition of inflammatory biomarkers, modulation of global gene expression, action against viral capsid. |
Oregano essential oils extract, carvacrol |
Origanum vulgae, Lippia graveolens |
300mg |
Should be supplemented for both Treatment and prevention. |
enhanced insulin sensitivity, and reduction in blood pressure when combined with other essential oils from cinnamon, cumin, and fenugreek |
Curcumin, Echinacea |
|
Fenugreek Seeds |
Antioxidant, anti-hypertensive, ant-hyperglycemic |
inhibition of cholesterol absorption, inhibition of erythrocyte membrane-bound sodium-potassium adenosine triphosphatase |
Fenugreek seed extract, trigonella, |
Trigonella foenum-graecum |
15-90 grams |
Should be supplemented for prevention. |
Protection against diabetes, high blood pressure, and CVD |
Oil of Oregano, Curcumin, Echinacea, Olive oil extract |
|
Curcumin |
Anti-inflammatory, antioxidant, Antiviral, |
Regulation of inflammatory cytokines, prevention of oxidant stress, correction of the risk associated with atherogenic index (AI) and High Fat Diets, suppression of replication in viruses |
Turmeric, curcumin, |
Curcuma Longa |
500-2000 mg |
Should be supplemented for both treatment and prevention. |
Prevention of CVD, hypertension, and diabetes. |
Echinacea |
|
Echinacea |
Anti-inflammatory, Antiviral, Antioxidant |
Radical scavenging effects, reversing the induction of multiple inflammatory cytokines, inhibition of growth of respiratory viruses, |
Root extract tincture, flower extract, herbal compound tea |
Echinacea angustigolia, Echinacea pallida, and Echinacea purpurea |
20 mg for crude herb extract, 6-9 ml for herb juice, 900 mg for root tincture. |
Should be supplemented for both treatment and prevention. |
Inhibition of a-amylase, a-glucosidase, and ACE activities, and hence the prevention of hyperglycemia and hypertension |
Curcumin |
|
Probiotics |
Anti-inflammatory, immunomodulation, Antiviral |
production of antiviral inhibitory metabolites, stimulation of the immune system, probiotic and virus interaction |
lactic acid bacteria ( of Lactobacillus and Pediococcus |
lactic acid bacteria ( of Lactobacillus and Pediococcus) |
10-20 billion colony forming units. |
Should be supplemented for both treatment and prevention. |
Currently not understood |
Oil of Oregano, Curcumin, Echinacea, Olive oil extract |
|
Humic Substances |
Antioxidant, Anti-inflammatory, antiviral, immunomodulation |
Inhibition of naked and enveloped viruses, |
humic, fulvic, and hymatomelanic acids; carboxyl, phenolic, alcoholic hydroxyls, quinoid groups, and methoxy, amino groups |
Humus |
500-2000 mg/kg |
Should be supplemented for both treatment and prevention. |
Currently not understood. |
Oil of Oregano, Curcumin, Echinacea, Olive oil extract |
|
Flavonoids (Liu et al., 2014) |
Antioxidant, Anti-inflammatory, antiviral, |
The ability to capture superoxide, hydroxyl, and lipid radicals, inhibition of pro-inflammatory markers, induction of colony-stimulating factor (M-CSF) |
astragalin, kaempferol-3-0(2”-0-galloyl)-glucoside, isoquericitin, and quercetin-3-0(2”-0-galloyl)-glucoside |
Fruits and vegetable plants |
500 mg/d |
Should be supplemented for both treatment and prevention. |
Inhibition of angiotensin converting enzyme activity, diminished risk of diabetes following dietary consumption. |
Curcumin, Echinacea |
Pharmacologic Treatments
Natural and Synthetic Cathepsin Inhibitors
The therapeutic potential for natural and synthetic cathepsin inhibitors have been studied in the relation to the functions of cysteine protease cathepsin B or L in the facilitation of the intracellular protein degradation mechanism employed by certain viruses during entry into host cells. Cysteine protease cathepsin B or L are used to achieve S protein cleavage, which is one of the two pathways, the other being cleavage by the host serine protease TMPRSS2, that allow fusion between the SAR-CoV virus and host cells (Simmons et al., 2005). Besides SAR-CoV, a comparable cathepsin was also utilized in the Ebola virus and most recently, SARS-CoV-2 (Vidal-Albalat & Conzalez, 2016; Fang, Karakiulakis, Roth, 2020). Cathepsin L, and to a lesser extent, cathepsin B, lysosomal cysteine proteases are involved in the series of enzymatic cleavages and modifications that S protein undergoes in the facilitation of viral endocytosis in SARS-CoV-2 (Ballout, 2020). A study conducted by Huang et al., (2006) showed that SARS-CoV utilized the enzymatic activity of the cysteine protease cathepsin L to infect ACE2-expressing cells, and inhibitors of cathepsin L blocked infection by SARS-CoV. Cathepsin L and B inhibitors are potential therapeutics for SARS-CoV-2. In the past two decades, an understanding on pharmacokinetic properties and the structural target of the inhibitory complex has led to the discovery of functional groups that have an important cathepsin inhibition effect (Vidal-Albalat & Gonzalez, 2016). Perhaps one of the most important cathepsin inhibitors that should be considered is teicoplanin, an antibiotic used in the treatment of Gram-positive infections, and which has also been established to be a broad spectrum cathepsin L inhibitor that has been found to be effective against MERS-CoV, HIV-1, HCV, Influenza viruses, flaviviruses, FIPV, and SARS- CoVs (Zhou et al., 2016). One of the first isolated natural products that have been identified as a cathepsin inhibitor is a leupeptin, a compound isolated in 1969 from a strain of Streptomyces exfoliates, and which when assessed at 10 μg/ml exhibited a > 95 % inhibition SARS-CoV entry mediated by cathepsin L (Vidal-Albalat & Gonzalez, 2016; (Simmons et al., 2005). A second compound tested inhibitory effect against Cathepsin is the Mir aziridine A, which is naturally present in the Red Sea sponge, Theonella swinhoei (Tabares, et al., 2012). Miraziridine A, whose inhibitory mechanism is largely promoted by the presence of the aziridine ring, includes synthetic versions and truncated analogues that have been shown to have a similar IC50 value that is comparable to that reported in the natural product (Vidal-Albalat & Gonzalez, 2016). Several other cathepsin B and/or L inhibitors have been isolated and structured, including the following: the tokaramide A, a cathepsin B inhibitor, that was isolated from a marine sponge, T. mirabilis, and its structure elucidated by (Fusetani et al., (1999); the gallinamide A/Symplostatin 4, was discovered by (Linington et al., (2009), from Schizothrix cyanobacteria and the natural product has subsequently been studied as an antimalarial agent, as well as its inhibitory activity against human cysteine cathepsin L and B, and high selectivity against other human cysteine proteases, such as cathepsin V (Miller et al., 2014); (Kwan et al, (2010) reported on grassypeptolides, a prolific source of bioactive secondary metabolites, which was isolated by Luesch’s group from Lyngbya cyanobacteria genus, and has been established to be a strong cathepsin L inhibitor, here the inhibition is diminished to 6 % residual activity; according to (Vidal-Albalat & Gonzalez, (2016), other cathepsins L and/or B inhibitors that have been isolated and evaluated include cyclohexenyl inhibitors, benzophenone inhibitors, ursolic acid, flavonoids, and triterpenes. The use of cathepsin L and B inhibitors in the treatment of COVID-19 is not currently emphasized regardless of their immense potential as shown by the evidence.
Antiviral Drugs
Several antiviral drugs used in the preliminary treatment of COVID- 19 were investigated, including remdesivir, favipiravir, interferon α (IFN-α), lopinavir/ritonavir, ribavirin, and arbidol. The criterion used for the tentative selection of various antiviral drugs was based on their activity against respiratory viruses and their broad-spectrum action against RNA viruses. A key antiviral considered for COVID- 19 treatment is Remdesivir, a nucleoside analogue prodrug that acts by inhibiting viral RNA polymerases, and which has been used for many years to treat hepatitis C virus (HCV) infection (Tchesnokov et al., 2019). Most symptoms of the first patient infected with COVID-19 in the United States resolved quickly following the intravenous administration of remdesivir (Holshue et al., 2020). In one study, utilizing subjects from Europe, Japan, and the United States, 68 % of patients that received at least one dose of Remdesivir registered an improvement in oxygen-support class, and 17/30 patients (57 %) on mechanical ventilation were extubated, leading to the preliminary conclusion that a compassionate use of Remdesivir facilitates clinical improvements in severe COVID-19 (Grein et al., 2020). However, a double-blind, randomized, placebo-controlled clinical trial conducted in China by (Wang, Y et al., (2020) did not identify any statistically significant clinical differences between remdesivir and the placebo group. Other nucleotide inhibitors that were approved for use against SARS-CoV-2 and with promising results include Sofosbuvir and Ribavin. Favipiravir (T-705; 6- fluoro-3-hydroxy-2-pyrazine carboxamide) is an antiviral drug that selectively inhibits the RNA-dependent RNA polymerase of influenza A H1N1 viruses, where it induces lethal mutagenesis (Furuta et al., 2013). In addition to anti-influenza virus activity, Favipiravir has also been shown to block replication in flavi-, alpha-, filo-, bunya-, noro-, and other RNA viruses and its effectiveness has been studied in COVID-19 compared to that of arbidol (Delang, Abdelnabi, & Neyts, 2018; Chen et al.., 2020). Favipiravir is one of the drugs that have been proposed for preliminary use in the treatment of COVID-19 because the causative agent, SARS-CoV-2 is an RNA virus. A clinical trial conducted on the use of Favipiravir in the treatment of COVID-19, with preliminary results from a total of 80 patients showed that Favipiravir had more potent anti-viral action compared to other tested antivirals, including lopinavir/ritonavir (Dong, Hu, & Gao, 2020). A study conducted by (Chen et al., (2020) to compare the efficacy of favipiravir and arbidol for COVID-19, confirmed the ability for the favipiravir to improve fever and cough within a short time, besides associating with mild and manageable adverse effects. Type 1 interferons, including IFN-α & IFN-β, are cytokines used as broad-spectrum antivirals in the treatment of hepatitis, though it has been reported to inhibit SARS-CoV reproduction in vitro (Stockman, Bellamy, & Garner, 2006). IFN-α, administered as a vapor inhalation at a dose of 5 million U, is one of the antivirals agents that were tentatively approved for use in the treatment of COVID-19 infections in China (Dong, Hu, & Gao, 2020). A synergistic role between ribavirin and type, I IFN (IFN-β1a or leukocytic IFN-α) was described in two studies performed in human cell lines and Vero cell lines (Morgenstern et al., 2005; Chen, F et al., 2004). Treatments of IFN- α in COVID-19 is used in combination with ribavirin, while additional clinical studies are being conducted to evaluate the effectiveness of IFN-α in the treatment of COVID-19 when combined with lopinavir/ritonavir (Sallard et al., 2020; Dong, Hu, & Gao, 2020). Studies are yet to report on the efficacy of IFN-α in the treatment of COVID-19. A study investigating the effectiveness of ritonavir/lopinavir, an antiviral medication used in the human immunodeficiency virus (HIV), for use in the treatment of patients with severe cases of COVID-19 showed that no benefit was attained beyond standard care (Cao, B. et al., 2020). A new study by (Sheahan et al. (2020) indicates that an orally bioavailable broad- spectrum antiviral, ribonucleoside analogue β-d-N4- hydroxycytidine (NHC; EID D-1931), inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice, resulting in the improvement of pulmonary function. NHC’s broad-spectrum activity is evident in other RNA viruses, including influenza, Ebola, CoV, and Venezuelan equine encephalitis (VEEV. In VEEV, the mechanism of action of NHC has been found to involve lethal mutagenesis where deleterious transition mutations accumulate in viral RNA (Urakova, et al., 2018). The mechanism of the broad spectrum NHC in COVID-19 is not yet clearly understood. In tests conducted in Ebola virus (EBOV) by Reynard et al (2015), NHC was found to interfere with replication and spread at non-cytotoxic concentrations, similarly, (Sheahan et al. (2020) demonstrated that NHC had a high antiviral potency against SARS- CoV-2, MERS-CoV, and SARS-CoV in primary human epithelial cell cultures without cytotoxicity. Another antiviral of interest is Arbidol, a non-nucleoside broad-spectrum antiviral drug with an immune-enhancing effect, and for which the efficacy against COVID-19 is still unknown. Arbidol has however been used for the treatment of influenza in Russia and China where the drug is approved for use (Huang et al., 2015). Even as testing continues for various antiviral agents against COVID-19, at the time of this writing there are no presently verified antivirals that are specific to COVID-19.
Table: Antiviral treatments in COVID-19
|
Antiviral Agent |
Therapy Class |
Target |
Affinity/Efficacy in COVID-19 (Kd or IC50, nM |
Adverse Effects and Potential contraindications |
Daily Dosing in Adults (mg) |
Normal Use |
Potential/Preliminary Findings in COVID 19 |
|
Remdesivir (Dong, Hu, & Gao, 2020; Sanders et al., 2020) |
Nucleoside Analogue |
RNA Polymerase Inhibition |
Still under investigation |
Potential kidney injury |
100 mg via IV infusion |
Treatment of Hepatitis C, and Ebola |
Resolution of symptoms, improvement in oxygen support class. |
|
Favipiravir (Dong, Hu, & Gao, 2020; Chen et al., 2020; Delang, Abdelnabi, & Neyts, 2018; Sanders et a., 2020) |
RNA-dependent RNA polymerase (RdRp) inhibitor |
RNA Polymerase inhibition |
Undergoing clinical trials |
Hyperuricemia, diarrhea, elevated transaminases, reduction in neutrophil count |
200 mg |
Influenza |
May potentially alleviate pyrexia, cough, and ARDS. |
|
Type 1 Interferons (IFN-β, IFN-α) (Chen F et al., 2004; Stockman, Bellamy, & Garner, 2006; Dong, Hu, & Gao, 2020; Sallard et al., 2020; Morgenstern et al., 2005; Chen, F et al., 2004) |
Cytokine |
First lines host defense against virus infection, particularly in relation to inflammation, signaling and immunomodulation functions. |
Undergoing Clinical Trials, preliminary findings do not show evidence of efficacious association. |
Hyper-inflammation, cytokine storm |
5 Million U administered as vapor |
Treatment of Hepatitis |
Used in combination with ribavirin and lopinavir/ ritonavir. Testing still ongoing to understand efficacy and effectiveness. |
|
lopinavir/ritonavir (Sanders et al.,2020; Cao B,et al.,2020, Chu et al., 2004) |
Protease Inhibitor |
3XCL Protease |
Still under investigation |
Adverse events observed in COVID-19 treatment, leading to premature discontinuation of treatment |
400 mg/100 mg taken orally |
HIV-1 treatment in pediatric patients MERS-CoV |
May work in synergism with ribavirin. No difference observed from the control group |
|
Ribavin (Dong, Hu, & Gao, 2020; ; Sanders et al., 2020; Sallard et al., 2020) |
Nucleoside Analogue |
Stops viral RNA synthesis, and viral mRNA capping |
Inconclusive data |
Substantial toxicity, Fever, nausea, muscle pain, vomiting, mood changes |
1000 mg administered intravenously |
RSV Infection, and Hepatitis C |
May have a synergistic effect with lopinavir and type 1interferons treatments. |
|
NHC (Reynard et al., 2015; Sheahan et al., (2020) |
Ribonucleoside analog |
Stops viral RNA synthesis |
Aprox IC50 = 0.14 μM |
Cell cytotoxicity may occur at higher concentrations. Body weight loss, lung hemorrhage |
500 mg/kg in experimental mice. |
VEEV, Ebola (experimental) |
Stops viral replication and improves respiratory function |
Antimalarial Drugs
Chloroquine or chloroquine phosphate, and hydroxychloroquine have traditionally been used as antimalarials are now broadly used in the treatment of COVID-19 with positive outcomes. Chloroquine phosphate and hydroxychloroquine sulphate are substituted 4-amino compounds that are differentiated by the hydroxy group (Tanenbaum & Tuffanelli, 1980). Chloroquine phosphate is one of the drugs that was clinically studied for effectiveness against COVID-19 patients during the initial outbreak in China (Gao, Tian, Yang, 2020). Results from over 100 patients showed that chloroquine phosphate was effective in limiting the worsening of pneumonia, improvement in lung imaging findings, promotion of negative conversion of the virus, and shortening of disease progression (Gao, Tian, Yang, 2020). Chloroquine phosphate is orally administered at a dose of 500 mg a day for adults and is taken two times a day by adults (Dong, Hu, Gao, 2020). Several preliminary studies have reported on the efficiency of hydroxychloroquine against COVID-19 (Gautret et al., 2020; Colson et al., 2020; Zhou, D. et al., 2020). Studies on hydroxychloroquine, an analogue of chloroquine, have demonstrated in vitro activity against SARS-CoV (Biot et al., 2006). In a French study involving 36 patients (6 asymptomatic, 22 with upper respiratory tract infections symptoms, and eight with lower respiratory tract infections) it was found that hydroxychloroquine treatment significantly reduced the viral load and was associated with the disappearance of COVID-19 (Gautret et al., 2020). Hydroxychloroquine is administered as a sulphate (200 mg), whereas chloroquine phosphate (500 mg) is administered as a phosphate salt (Dong, Hu, Gao, 2020). According to early observations, the action of hydroxychloroquine was most likely due to the inhibition of cytokine storm by suppressing T cell activation. Zhou states that Chloroquine and hydroxychloroquine can inhibit MHC (major histocompatibility complex) class II expression, inhibit antigen presentation, and down-regulate immune activation mitigating or reducing the cytokine storm associated with severe COVID-19. Thus, chloroquine and hydroxychloroquine can reduce the production of various pro-inflammatory cytokines, such as IL-1, IL-6, interferon-α, and tumor necrosis factor, which are involved in the propagation of the cytokine storm (Zhou D., et al, 2016). Some clinical trials have however disputed the effectiveness of hydroxychloroquine in the treatment of COVID-19, especially in combination with azithromycin. A clinical trial conducted by (Rosenborg et al., (2020) investigated the association between treatment with hydroxychloroquine or azithromycin and in-hospital mortality among patients with COVID-19 in New York, with findings showing that treatment with hydroxychloroquine, azithromycin or both was not significantly associated with reduction of in-hospital mortality. The effectiveness of hydroxychloroquine treatment was observed to depend on whether it was given early (< 7 days of symptoms) or late (> 7 days of symptoms), with findings from one study showing that only 1.17 % of patients provided with early hydroxychloroquine treatment required hospitalization, compared to 3.2 % in late treatment patients (Pagliaro & Meneguzzo, 2020). Zinc synergism is also required to improve the efficacy of hydroxychloroquine in the treatment of COVID-19 and, therefore, zinc supplementation is advised (Shittu & Afolami, 2020); Derwand & Scholz, 2020).
Table: Antimalarial drugs treatments in COVID-19
|
Antimalarial Agent |
Therapy Class |
Target |
Affinity/Efficacy in COVID-19 (Kd or IC50, nM |
Adverse Effects |
Daily Dosing in Adults (mg) |
Normal Use |
Preliminary Findings |
|
Hydroxychloroquine or HCQ (Gautret et al., 2020; Colson et al., 2020; Zhou et al., 2020; Schrezenmeier & Dorner, 2020; Xia et al., 2020; ; Sanders et al., 2020) |
Antimalarial |
Blockage of viral entry, anti-inflammatory activity through suppression of T-cell activity, |
Under investigation |
Retinopathy, known hypersensitivity |
400 |
Treatment for malaria, and Rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and antiphospholid syndrome (APS).
|
Helps reduce/eliminate SARS-CoV-2 viral load, most likely involved in the suppression of cytokine storm through inhibition of T-cell activation, pneumonia treatment, improvement of lung imaging findings, shortening of disease course. HCQ treatment should be started early in order for the benefits to be realized. |
|
Chloroquine Phosphate (Gao et al., 2020; Dong, Hu, & Gao, 2020; ; Sanders et al., 2020) |
Antimalarial |
Same as Hydroxychloroquine |
Under investigation |
Retinopathy, known hypersensitivity |
1000 (Chloroquine phosphate), 600 (chloroquine) |
Treatment for malaria, and Rheumatoid arthritis (RA), systemic lupus erythematosus (SLE) |
Effective against COVID-19-related pneumonia, improvement of lung imaging findings, promoting a virus negative conversion, shortening of disease course. |
Antibiotics
Few antibiotics have been used in the treatment of COVID-19. According to (Gautret et al., (2020), azithromycin reinforces the effect of hydroxychloroquine treatment in the reduction of viral load or elimination of SARS-CoV-2 in COVID-19 patients. The findings were however disputed by (Molina et al., (2020), who reported that there was no evidence to show rapid antiviral clearance or clinical benefit when azithromycin is combined with hydroxychloroquine in the treatment of patients with severe COVID-19 infection. Azithromycin is a broad-spectrum macrolide antibiotic that has demonstrated effectiveness in the treatment of upper respiratory tract infections, lower respiratory tract infections, and infections of the skin and skin structures, and side effects may include mild cardiotoxic effects (Piscitelli, Danziger, Rodvold, 1992; Ray et al., 2012). Previous research shows that azithromycin has shown effectiveness against patients with acute obstructive pulmonary disease (Albert et al., 2011). Against COVID-19, patients receiving combined treatment of hydroxychloroquine and azithromycin may have better clinical improvements, though further studies are required to confirm the effect (Gautret et al., 2020). No additional evidence is available on the effectiveness or role of azithromycin in the treatment of COVID-19.
Table: Antibiotic drugs treatments in COVID-19
|
Agent |
Classification |
Target |
Efficacy |
Adverse Effects |
Daily Dosing in Adults (mg) |
Normal Use |
Preliminary Findings |
|
Azithromycin (Molina et al., 2020; Gautret et al., 2020; Sanders et al., 2020; Ray et al., 2012) |
broad spectrum macrolide antibiotic |
Upper respiratory infection |
Under Investigation |
mild cardiotoxic effects |
500 mg on day 1, 250 mg on day 2 to day 5. |
Acute Pulmonary Disease, general effectiveness against upper and lower respiratory infections, and skin infections. |
May prevent bacterial superinfection, thought to positively affect clinical activity when combined with hydroxychloroquine. Requires more studies to evaluate clinical benefit. |
JAK Inhibitors
The inflammatory response has been identified as a major cause of lung damage and subsequent mortality and, therefore, screening for hyper-inflammation in COVID-19 (using lab trends such as increased ferritin levels decreased platelet counts, and erythrocyte sedimentation) provides a potential for treatment with JAK inhibition (Mehta et al., 2020; Haberman et al., 2020). For instance, the common γ-chain (γc), used by IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21 associated exclusively with JAK3 and is the only receptor subunit that uses JAK3(Hofmann et a., 2002). The pathway plays a role in the ARDS cytokine storm observed in COVID-19 patients with severe symptoms (Guan et al., 2020; Stebbing et al., 2020). It has been noted that respiratory failure due to ARDS is the leading cause of mortality in COVID-19, in addition to the secondary haemophagocytic lymphohistiocytosis (sHLH) (Mehta et al., 2020). Studies show that JAK inhibitors such as Baricitinib could play a role in the prevention of both inflammation and cellular viral entry in COVID-19 (Mehta et al., 2020; Richardson et al., 2020). Baricitinib inhibits JAK1/2 immune pathways, besides inhibiting the AP2-associated protein kinase 1 (AAK1), which may interrupt the passage of virus into cells and the intracellular assembly of virus particles (Richardson et al., 2020). A recent has demonstrated that baraticitinib may not be ideal for the management of CVID-19 because it causes lymphocytopenia, neutropenia, viral reactivation, and may increase the incidence of co- infection (Praveen et al., 2020). Tofacitinib suppresses the production of IFN-α production via plasmacytoid dendritic cells and inhibits atherogenic and antiviral effects of IFN-α (Boor et al., 2017). Other selective JAK inhibitors approved for use in rheumatoid arthritis and myelofibrosis, such as fedratinib and ruxolitinib, possess powerful anti-inflammatory properties and may offer protection against consequences of elevated levels of cytokines as observed in COVID-19 (Stebbing et al., 2020). Fedratinib is specific against JAK-2 compared to other JAK family kinases, while ruxolitinib is specific for JAK1 and JAK2 (Pardanani et al., 2015; Zhou et al., 2014).
Table: JAK Inhibitor drugs for treatments in COVID-19
|
Agent |
Therapy Class |
Target |
Affinity/Efficacy in COVID-19 (Kd or IC50, nM |
Adverse Effects and Potential Contraindications |
Daily Dosing in Adults (mg) |
Normal Use |
Potential/Preliminary Findings in COVID 19 |
|
Baricitinib (Mehta et al,. 2020; Richardson et al., 2020; Sanders et al., 2020; Praveen et al., 2020). |
JAK inhibitor |
AAK1 and cyclin G-associated kinase binding. |
IC50 = cell free (17), Cell (34) |
Sores, Nausea, interaction with probenecid. In COVID-19 may lead to lymphocytopenia, neutropenia, viral reactivation, and and may increase the incidence of co-infection |
2-4 |
Treatment of moderate to severe rheumatoid arthritis |
May work as an inti-inflammatory to prevent cytokine storm lung damage in severe or critically ill COVID-19 patients. Not recommended for COVID-19 management. |
|
Fedratinib (Stebbing et al., 2020; Pardanani et al., 2015; Sanders et al., 2020) |
JAK inhibitor |
JAK2 selective inhibition |
IC50 = cell free (32), Cell (960) |
Anemia, gastrointestinal symptoms |
400 |
Used in the treatment f patients with primary or secondary myelofibrosis. |
Potential anti-inflammatory to prevent cytokine storm lung damage in severe or critically ill. |
|
Ruxolitinib (Zhou et al., 2014; Stebbing et al., 2020; Sanders et al., 2020) |
JAK inhibitor |
JAK 1 and JAK2 Tyrosine kinase inhibitor |
IC50 = cell free (100), cell (700) |
Opportunistic infections, and rare malignant substances |
25 |
Used in the treatment f patients with primary or secondary myelofibrosis. |
Potential anti-inflammatory to prevent cytokine storm lung damage in severe or critically ill. |
|
Tofacitinib (Boor et al., 2017) |
JAK inhibitor |
Suppression of IFN-α production. |
IC50 = cell free (1) |
Blocking of the IFN-α pathway may enhance viral infection |
20 |
Treatment of rheumatoid arthritis/Autoimmune diseases |
Potential anti-inflammatory to prevent cytokine storm or treat hyper-inflammation and prevent lung tissue damage in severe COVID 19 |
Humanized Antibodies (Tocilizumab)
Humanized antibodies refer to antibodies (usually monoclonal) for non-human species whose protein sequences are modified to enhance the similarities with antibody variants that are naturally produced by humans. Monoclonal antibody therapeutics used in COVID-19 are based on the understanding that a significant number of COVID-19 patients with severe disease experience an immune- mediated inflammatory disease (Haberman et al., 2020). Interleukin 6 is a key cytokine that contributes to host defense against infections and tissue injuries, but exaggerated, or excessive production of IL-6 may trigger an acute severe systemic inflammatory response referred to as the “cytokine storm”, due to the fact that enhanced levels of IL- 6 may activate the coagulation pathway and vascular endothelial cells but not inhibit myocardial function (Tanaka, Narazaki, & Kishimoto, 2016). Tocilizumab is a humanized monoclonal antibody against the IL-6 receptor (Zhang et al., 2020). IL-6 is multi-effective cytokine with pro-inflammatory and anti- inflammatory effects plays a central role in a cytokine storm, and IL- 6 is one of the pro-inflammatory cytokines that is remarkably up- regulated in COVID-19 (Zhang et al., 2020; Li et al., 2020). Tocilizumab particularly binds to soluble and membrane-bound IL-6 receptors (sIL-6R and mIL-6R) and inhibits sIL-6R and mIL-6R- mediated signal transduction and, as a result, it has been approved for the treatment of rheumatoid arthritis and systemic juvenile idiopathic arthritis (Zhang et al., 2020; Yokota et al., 2005). A study conducted by (Xu et al., (2020) on the effectiveness of Tocilizumab in the treatment of 20 COVID-19 patients showed that a remarkable improvement in symptoms, with 20 of the patients (75 %) attaining a lowered oxygen intake and one patient requiring no oxygen intake. The authors found no adverse reactions in association with the disease and 19 patients (90.5 %) had been discharged within 13.5 days after treatment with tocilizumab, implying that the humanized monoclonal antibody is effective in the treatment of severe COVID-19 cases (Xu et al., 2020). The findings were corroborated by other studies, including (Zhang, X. et al., (2020), (Zhang, C. et al., (2020) and (Michot et al., (2020). Leronlimab (PRO 140) is a humanized IG4 monoclonal antibody that has recently been demonstrated to show the promising result in the treatment of COVID-19. Leronlimab is a chemokine receptor 5 (CCR5) antagonist whose function is based on the characterization of CCR5 as a co-reception in human deficiency virus (HIV) viral entry into white blood cells, and later in other pathogens, such as Dengue and Staphylococcus aureus (Chary et al., 2020). The drug may be essential in treating a dysregulated immune response characterized by runaway inflammation, including cytokine release syndrome (CRS), which has been identified as a major driver of pathology in severe COVID-19 (Mehta et al., 2020). In a clinical trial conducted by (Patterson et al., (2020), leronlimab was demonstrated to disrupt the CCL5/RANTES-CCR5 Pathway, restoring immune homeostasis and reducing plasma viral load in critical COVID-119 patients. The study involved a selection of 10 patients with severe COVID-19 and who received subcutaneous 700 mg injection of leronlimab, with findings showing a reduction in plasma IL-6 within 3 days, and a complete return to healthy levels of IL-6 within 14 days (Patterson et al, 2020). The findings also showed a marked reduction in plasma viremia of SARS-COV-2, in addition to normalization of the CD4+ and CD8+ T cell ratio in blood was observed (Patterson et al, 2020).
Table: Humanized antibodies for treatment in COVID-19
|
Agent |
Therapy Class |
Target |
Affinity/Efficacy in COVID-19 (Kd or IC50, nM |
Adverse Effects and Potential Contraindications |
Daily Dosing in Adults (mg) |
Normal Use |
Potential/Preliminary Findings in severe COVID 19 |
|
Tocilizumab ( Xu et al., 2020; Zhang et al., 2020; Michot et al., 2020; Yokota et al., 2005) |
Humanized Monoclonal Antibody |
Inhibition of IL-6 receptor |
Still under investigation |
No significant abnormalities have been reported. |
8 mg/kg intravenously, 8 hours apart (24 mg/kg daily). |
treatment of rheumatoid arthritis and systemic juvenile idiopathic arthritis |
Improvement in symptoms, including lowered oxygen intake in respiratory failure |
|
Leronlimab (Chary et al., 2020; Patterson et al., 2020). |
Humanized Monoclonal Antibody |
CCR5 Antagonist |
Still under investigation |
In phase 2a testing, Leronlimab was associated with diarrhea, headache, and swollen lymph nodes. |
700 mg subcutaneous injection |
Is an investigational HIV drug |
A reduction of plasma IL-6 was observed as early as 3 days administration, and to reduction of IL-6 to normal levels by day 14. A decrease in plasma viremia in all patients at day 7. |
Nitric Oxide (Methylprednisolone)
Nitric Oxide (NO) gas has been approved by the Food and Drug Administration for the treatment of pulmonary hypertension of new- borns suffering from hypoxic respiratory failure and is advocated as a rescue treatment in adults with hypoxic ARDS (Lei et al., 2020). The potential use of inhaled NO gas (iNO) in coronaviruses- related SARS was first investigated during the SARS-CoV-1 outbreak in China, with findings showing improved arterial oxygenation and the prevention of lung tissue damage by the disease, or by hyperinflation damage caused by the ventilator treatment (Chen et al., 2004). Due to high similarities between the viruses responsible for SARS and COVID-19, NO has been hypothesized to improve oxygenation in severe cases. (Lie et al., (2020) are evaluating the effectiveness of treatment with iNO at 80 ppm for the first 48 hours and, and subsequent reduced 40 ppm until the resolution of severe hypoxemia. A similar study is being carried out by (Begun et al., (2020) and (Gianni et al., (2020), who are interested in understanding the role of inhaled iNO in lung complications associated with COVID-19. Based on the findings of (Chen et al., (2004), it is hypothesized that iNO will have a positive effect on the treatment of COVID-19. Theoretical risks associated with the therapeutic use of iNO include pulmonary edema, methemoglobinemia, hypoxia, and hypertension (Gianni et al., 2020).
Immunoglobulins
Convalescent sera have been used to combat major infectious disease outbreaks in history, including poliomyelitis, measles, mumps, and influenza (Casadevall & Pirofski, 2020). At the time, convalescent sera were one of the most useful and efficacious means of stemming outbreaks. Analysis of evidence on the use of convalescent sera during the 1918 H1N1 Spanish flu outbreak shows low mortality rates among those who were treated with the serum (Luke et al., 2006). As opposed to vaccine-mediated immune induction, which may take varying periods to develop depending on the immune status of the recipient, passive antibody administration provides immediate immunity to the recipients (Casadevall & Pirofski, 2020). While not well developed, the use of pooled IgG has been used in the treatment of specific ailments such as measles and hepatitis A (Hemming et al., 2001). Some of the challenges that have made it difficult to develop immunoglobulin-based medication include dosing, efficient analysis of the diversity of proteins in the preparations, and possible contamination with blood- borne infections (Casadevall & Pirofski, 2020). Experience gained from previous outbreaks involving coronaviruses, such as SARS- CoV-1, convalescent sera containing neutralizing antibodies may be effective against SARS-CoV-2, this is particularly possible when they contain sufficient levels of IgG (Zhang et al., 2005; Fischer et al., 1983). The development of humanized monoclonal antibodies has overcome key shortcomings experienced and has led to a reduced focus on immunoglobulin preparations.
Herbal Extracts
Traditional Chinese Medicine
Traditional Chinese medicine (TCM) approaches, including oral administration of preventive herbal formulae, wearing of Chinese Medicine Sachets, indoor herbal fumigation, among others, were recommended for the treatment of COVID-19 when the outbreak started (Luo, H. et al., 2020). TCMs approaches have previously been used in the treatment and prevention of other major outbreaks, including the use against the 2003 SARS outbreak (Liu et al., 2004). Various TCM formulations have been utilized in the treatment of COVID-19, including qingfei paid decoction (QPD), gancaoganjiang decoction, and qingfei touxie fu zheng recipe, among others (Ren, Zhang, & Wang, 2020). (Yang, Y. et al., (2020) reported that more than 85% of COVID-19 patients in China were receiving TCM treatment for the infection. As reported in a press conference on QPD intervene among 701 confirmed cases, the results showing that 130 cases were cured and discharged, clinical symptoms disappeared in 51 cases, symptom improvement in 268 cases, while 212 cases showed stable symptoms without aggravation (Ren, Zhang, & Wang, 2020). The evidence reviewed above suggests that traditional Chinese medicine may be effective in the treatment of COVID-19. Research on the general effectiveness of TCM is relatively high (including animal experiments, in vitro cells, and data mining) but evidence regarding effectiveness in COVID-19 is generally limited.
Discussion
Applying the Findings on Dietary, Prescriptive, and Herbal Remedies on the Prevention, Treatment, and Management of COVID-19
The results obtained from the scoping review are discussed in accordance with the major categories reviewed, with dietary supplements, pharmacologic drugs, and herbal remedies discussed in the same order as they are presented in the results section. The discussed items are also ordered in relation to the level of evidence on potential effectiveness in the prevention, management, or treatment of COVID-19. The key areas of concern in COVID-19, as determined from the analysis of background data on the infection and the role of comorbidities, including inflammation, immune response, and oxidative stress. Analysis of the most effective drugs, supplements and herbal remedies for the identified key concerns will provide the best opportunity for the prevention of severe disease and adverse outcomes associated with COVID-19.
Key Dietary and Herbal Remedies
Based on the findings of the review, key dietary and herbal remedies that may be considered for supplementation for prevention and during treatment in COVID-19 include vitamin C, vitamin D, zinc, selenium, glutathione, oil of oregano, curcumin, flavonoids, and echinacea.
Vitamin C
The importance of vitamin C is underscored by the fact that the nutrient is already utilized in the treatment and prevention of COVID-19. Evidence demonstrates that vitamin C plays an important role in immune function, particularly as an essential component in the production of IFN-α and –β, which facilitate the early immune response to viral infections. The evidence presented also points to the function of vitamin C as an antioxidant. As an antioxidant, vitamin C limits oxidative damage associated with reactive oxygen species produced during respiratory burst or inflammatory response, pointing to a possible beneficial role in COVID-19 associated pneumonia. Vitamin C is water-soluble and requires frequent replenishment through diet or supplementation. The production of cortisol in response to stress or psychological factors may result in further depletion of vitamin C and, therefore, leading to insufficient levels for maintenance of oxidative integrity or optimum immune function in diseases such as COVID-19. A link between psychological factors, such as stress and depression, and comorbidities identified as major risks for severe COVID-19 disease, including diabetes, Hypertension and CVD have been previously established. Psychological factors may impact diabetes and cardiovascular risk in several ways, including the following: influencing lifestyle risk factors for diabetes such as physical activity and adiposity; adversely influencing diabetes directly through inflammation and glucose dysregulation; and developing the processes through which diabetes stimulates cardiovascular complications (Hackett & Steptoe, 2016). The incidence of depression in people suffering from diabetes mellitus (DM) is between two and three times higher than controls, indicating high levels of cortisol and the associated depletion of vitamin C (Badescu et al., 2019). Besides having a causal relationship with psychological stress, hypertension may also cause oxidative stress, which has led to the consideration of antioxidants as possible hypertension therapy (Sparrenberger et al., 2009; Baradaran, Nasri, & Rafieian-Kopaei, 2014). Based on the findings, on the evidence, adequate vitamin C supplementation may be essential for the prevention and may play an important role in the treatment of COVID-19 to exert antioxidant, immunomodulatory, and antiviral effects. As an antioxidant, vitamin C may help address the oxidative stress associated with the anti-inflammatory response, and COVID- 19 comorbidities such as CVD, hypertension, and Diabetes.
Vitamin D
Vitamin D is an essential component of several metabolic pathways in the human body. Most of the vitamin D is processed in the skin during exposure to sunlight, though it can also be sourced through diet from a limited number of foods, including fatty fish, fish liver oils, mushrooms, and to a lesser extent cheese, beef, egg yolks, and liver. Besides its well-known calcium and phosphate regulatory function, evidence reviewed shows that Vitamin D deficiency may have a role in respiratory infections, where supplementation decreases the incidence or severity of both viral and bacterial infections in the respiratory tract. Specific inhibitory effects against replication of rhinovirus or respiratory syncytial virus (RSV) or influenza A virus has already been established, besides modulating the expression and secretion of type 1 interferon, chemokines (CXCL8 and CXCL10), as well as pro-inflammatory cytokines, such as TNF and IL-6, which enhance the inflammatory response and, hence, adequate levels of vitamin D may be critical in early COVID-19 disease. The evidence analyzed shows that vitamin D supplementation may also protect against a dysregulated immune response through enhanced production of Tregs subsets (CD25, Foxp3 (+) Tregs and IL-10 producing Tregs). Vitamin D may therefore play a role in the protection against cytokine storm/hyper- inflammation in COVID-19. As an antioxidant, vitamin D may enhance the antiviral activity of the immune system through the release of ROS. Vitamin D deficiency is also implicated in major COVID-19 comorbidities, including cardiovascular disease, cerebrovascular disease, and hypertension, suggesting that supplementation may protect against the harmful or COVID-19 exacerbating factors of the different comorbidities. Adequate vitamin D supplementation is therefore strongly advised, both for prevention and during COVID-19 treatment.
Zinc
Zinc is an essential mineral that naturally occurs in various foods including oysters, red meat, poultry, beans, nuts, crabs, and whole grains. The evidence reviewed implicates the role of zinc in numerous cellular functions, such as cell proliferation, RNA and DNA synthesis, stabilization of cell structures/membrane, redox regulation, and apoptosis. A notable finding of the evidence reviewed is that zinc ions are bound to Metallothioneins (MTs) and are rapidly released for the regulation of oxidative stress and inflammatory cytokines. The ability for MTs to protect against ROS implicated in ARDS and SARS, and particularly superoxide, as reported by (Kang et al., (2015) and (Jarosz et al., (2017) makes adequate zinc supplementation an important consideration in the treatment of COVID-19. The evidence also points to the role of oxidative stress and the production of pro-inflammatory cytokines in zinc deficiency. Zinc supplementation in COVID-19 therefore may be critical due to the fact that the inflammatory response is heavily associated with disease pathogenesis and that oxidative stress may be the key factor in disease progression, particularly in relation to major COVID-19 comorbidities such as old age, hypertension, diabetes, and CVD. The combination of Zn2+ and pyrithione at low doses were also shown to inhibit SARS-CoV in cell culture, which raises speculation that a similar effect may be observed in SARS- CoV-2.
Selenium
Selenium is a trace element that is naturally present in many foods. Selenium has several critical functions in the human body, which include protection against oxidative stress and infections. Selenium exerts its antiviral effects through glutathione peroxidases and may play a key role in enhancing the antioxidant function of glutathione in the extracellular space, cell cytosol, and cell membranes, particularly in the GIT. Selenium deficiency plays a role in viral pathogenesis, which may be exerted through impaired lymphocyte proliferation, and hence supplementation improves the ability for antiviral therapy to prevent infection. Selenium insufficiency and dysregulation of selenium synthesis cofactors are involved in the pathophysiology of many diseases, including cardiovascular disorders, immune dysfunctions, cancer, muscle and bone disorders, endocrine functions, and neurological disorders. Despite its important roles, evidence shows that high levels of selenium concentration may be associated with diabetes. While selenium may be abundant in many common foods, the deficiency should be investigated in viral infections, including COVID-19, to enhance therapeutic response.
Glutathione
Glutathione is widely known for its antioxidant properties due to its abundance of sulfhydryl groups, which play an essential role in the protection against ROS. GSH deficiency has been associated with increased ROS, depletion of ATP, which lead to alteration of cellular apoptotic response that favour necrosis. Decreased GSH levels are also implicated in several pathological conditions that result from or are exacerbated by oxidative stress, including the major comorbidities associated with COVID-19 such as hypertension, diabetes, CVD, cancer, and general immune dysfunction. Glutathione is also believed to play an important role in the channelling of the antioxidant effects of selenium. Selenium itself is a precursor to glutathione, and glutathione is called the “master antioxidant” as it boosts the utilization and recycling of other antioxidants, such as vitamins C and E, alpha-lipoic acid, and Coenzyme Q10. Evidence also shows that glutathione peroxidases are key enzymatic pathways involved in the clearing of reactive oxygen species (ROS) generated by inflammatory cells.
Herbal Extracts
Various herbal extracts reviewed in the present study showed a capacity to exert health effects that might be useful in the prevention or treatment of COVID-19, and amelioration of contributing roles played by COVID-19 comorbidities in disease progression. Based on the evidence provided, herbal extracts with the most potential benefits in COVID-19 include oil of Oregano, Curcumin, flavonoids, and Echinacea. The table below briefly highlights the various potentially beneficial properties of selected herbal supplements and their likely role in COVID-19.
Table: Selected herbal extracts and potential role in COVID-19
|
Herbal Extract |
Health Properties |
Potential Role in COVID-19 |
|
Curcumin |
|
Regulation of inflammatory cytokines during treatment for severe and critical COVID-19; prevention of oxidative stress; potential suppression of SARS-CoV-2 replication. Potential prevention CVD, hypertension, and diabetes, and limitation of the impact on COVID-19 pathogenesis. Curcumin supplementation prior to active infection may also enhance immune capacity for COVID-19 by limiting role of oxidative stress. |
|
Echinacea |
|
May be used in severe and moderate COVID-19 to achieve radical scavenging; reversal of the induction of inflammatory pathway; and Inhibition of a-amylase, a- glucosidase, and ACE activities. Echinacea supplementation prior to active infection may also enhance immune capacity for COVID-19 through radical scavenging, among other health benefits. |
|
Flavonoids |
|
May be used in COVID-19 treatment to facilitate capturing of superoxide, hydroxyl, and lipid radicals; inhibition of pro-inflammatory markers; inhibition of angiotensin converting enzyme activity; lowering the risk associated with diabetes; and induction of the colony-stimulating factor (M-CSF). Antioxidant properties and ability to inhibit ACE enzymes may also work as a preventive measure against COVID-19. |
|
Oil of Oregano |
|
May be used in COVID-19 treatment to achieve inhibition of inflammatory biomarkers; modulation of global gene expression; possible action against viral capsid; may also enhance insulin sensitivity in patients co-infected with diabetes. |
Areas of Focus to Optimize Prevention and Therapeutic Outcomes in COVID-19
Based on the evidence from the studies reviewed, several compounds/extracts/and formulations may be administered to enhance effectiveness of prevention and treatment strategies in COVID-19. Based on the knowledge gained from existing clinical data on COVID-19, particularly in relation to potential severity and adverse outcomes, and literature on the proximate role of major comorbidities, the main categories of focus in the prevention and treatment of COVID-19 include oxidative stress, the inflammatory response, and antiviral therapy. An evidence-based brief discussion of the key compounds/extracts/and formulations for each category is presented below.
-
Oxidative Stress
While there is no published data on the role of oxidative stress in COVID-19, findings of the literature review show that oxidative stress could have a role, especially in SARS pathogenesis in COVID-19, and it is also a unifying factor in most, if not all, of the comorbidities associate with severe symptoms and adverse outcomes in COVID-19.
Figure: Oxidative Stress in COVID-19 Pathogenesis and Key Comorbidities
It may also play a role in the dysregulated response by pro- inflammatory cytokines or the cytokine storm. Consequently, oxidative stress is suspected to play a major role in the pathogenesis of COVID-19 and, hence, the analysis of the approximate association between oxidative stress in the major comorbidities and COVID-19 should provide a potential basis for therapeutic, dietary supplementation, and herbal application in COVID-19. Based on the findings on the potential application of antioxidant balance in the prevention and treatment of COVID-19, it is hypothesized that antioxidant use with respect to the scavenging efficiency of specific products may facilitate improved outcomes in COVID-19, particularly in those at greater risk due to identified comorbidities. Mainstay antioxidants based on published data include glutathione, vitamin C, vitamin D, and zinc. As shown by the evaluated evidence, vitamin D, in addition to its main roles, including anti- inflammatory response in viral diseases, may boost mucosal defences through the antioxidant pathway, which may explain its effectiveness in common colds (known to increase oxidative stress). Vitamin D has a general impact on respiratory health and a significant impact on COVID-19 infection may be attained through daily supplementation as proposed by the metanalysis conducted by (Bergan et al., (2013). Zinc, a micronutrient that plays an important role as a structural component in proteins is shown to exhibit antioxidant activity by controlling oxidative stress and inflammatory cytokines, roles achieved due to the fact that zinc is bound to metallothionein’s, which act as a potent electrophilic scavenger and cytoprotective agent’s inflammatory injury, with the ability to capture a wide range of ROS, such as superoxide, hydroxyl radicals, nitric acid, and hydrogen peroxide. As reported by (Arthur, McKenzie, & Beckett (2003) the antioxidant effects of selenium may be responsible for the removal of hydrogen peroxide and lipid hydroperoxides, with the potential to impact on immune processes. Glutathione has already been established to be an effective antioxidant for use in COVID-19. Glutathione plays a critical role in the following: cellular protection against ROS, effective Th1/Th2 cytokine response pattern, regulation of T cell effector functions and metabolic activity, and improvement of the cysteine-mediated regulatory circuit. Various herbal extracts have also been shown to possess potent antioxidant properties that may be crucial in the prevention and treatment of COVID-19, including echinacea, curcumin, oil of oregano, and flavonoids. Supplementation with flavonoids, echinacea, curcumin, and oil of oregano may be essential as a preventive measure for severe disease due to the ability to capture free radicals and, hence, lessening the risk associated with various comorbidities and the dysregulation of the inflammatory pathway and possible ARDS. Supplementation with the herbal extracts may also, confer other health benefits that will lead to an overall improvement in health and immune function in individuals.
-
Inflammatory Response in COVID-19
Inflammation plays a crucial role in the resolution of numerous conditions, including viral and bacterial infections. However, in certain circumstances, such as in dysregulated cytokine response, the inflammatory response may contribute to further damage and adverse disease outcomes. A dysregulated response by pro- inflammatory cytokines is a key feature of COVID-19 pathogenesis, particularly in relation to SARS and other outcomes of severe COVID-19 disease. Therefore, inhibition of inflammatory-specific inflammatory mediators may be crucial in the treatment of severe COVID-19. Various dietary supplements and herbal extracts evaluated have potential anti-inflammatory properties that may be beneficial in the treatment, prevention, and management of COVID- 19, and these include vitamin D, zinc, selenium, curcumin, echinacea, humic substances, flavonoids, and oil of oregano, and probiotics. While all these dietary supplements will provide some level of protection to prevent or mitigate COVID-19 infection, only a few of them may be supplemented during treatment for severe COVID-19 disease. Supplements that should be considered for treatment in a cytokine storm or hyper-inflammation include vitamin D, zinc, glutathione, curcumin, Echinacea, flavonoids, and oil of Oregano.
In addition to the dietary supplements described above, hyper- inflammation in COVID-19 may be treated using JAK inhibitors (such as tofacitinib and baricitinib), and adjuvant therapies or humanized antibodies (such as leronlimab and tocilizumab), which have shown promising results in blocking inflammatory mediators, such as IL-6 (tocilizumab) and chemokine receptor 5 (leronlimab). For instance, preliminary findings show that leronlimab effectively disrupts the CCL5/RANTES-CCR5 Pathway, restoring immune homeostasis. Antimalarials such as hydroxychloroquine and chloroquine may offer significant benefit when introduced early in the disease process, especially when combined with zinc, vitamin C and/or the macrolide antibiotic azithromycin.
-
Antiviral Therapy
The use of pharmaceutical compounds that target and inhibit the causative agent of COVID-19 (SARS-CoV-2) provides a potentially curative approach for the disease. There are numerous investigational drugs that have shown promising results in relation to the treatment of COVID-19. Most of the antiviral agents that are still undergoing testing, and which have been provisionally approved for use in COVID-19 are aimed at inhibiting a specific a critical process in the life cycle of the virus, which stops viral replication, and eventual elimination of the virus from the body. Antiviral agents that have shown promising results for use in COVID-19 include Remdesivir, a nucleoside inhibitor with broad- spectrum activity against RNA viruses; and NHC, a ribonucleoside analogue that stops RNA viral synthesis, stopping viral replication and improving respiratory function.
Antiviral therapy may also be augmented with selenium, zinc, magnesium, glutathione, vitamin C, and Vitamin D supplementation, particularly in cases where deficiency is noted. The reviewed evidence has suggested the ability of selenium supplementation to improve the efficacy of antiviral treatment.
While numerous drugs, herbal, and dietary supplements have been hypothesized to confer some level of protection against, the unchecked use of herbal and dietary supplements in ambulatory care are discouraged due to the risk of adverse drug interactions (Graham et al., 2008).
5.0 Conclusion
On December 31, 2019, the World Health Organization (WHO) was formally notified about a strange cluster of cases of pneumonia in Wuhan, a city of 11 million people in central China. Seventy days later, on March 11, 2020, there were more than 118,000 cases of this infection caused by a SARS-CoV-2 virus in 114 countries, 4,291 people had lost their lives and the WHO declared a global pandemic. Viral load in SARS-CoV-2 (or COVID-19) infection predicts mortality (Pujadas E. et al. 2020), and a key characteristic of severe COVID-19 is the cytokine storm or uncontrolled systemic inflammatory the response that results from the release of enormous amounts of pro-inflammatory cytokines which subsequently contribute to severe lung and organ damage and to many of the deadly sequelae of this disease. According to the CDC, descendant’s of 1918 influenza virus (or Spanish Flu) still circulate today-102 years later, and although current seasonal influenza vaccines provide some protection against the 1918 virus, there is currently no vaccine against COVID-19. Without a vaccine, only herd immunity can contain the expansion of the infection, but with strict isolation, only a small percentage of the population has antibodies to the disease. Typically, 80-90 % of the population must be infected and recover to confer herd immunity. Flattening the curve of infection by quarantining the healthy was recommended soon after a pandemic was declared, however, this procedure prevents the overloading of medical facilities, but only draws out the “infection curve” over a longer period. Perhaps months or even years. Complete isolation will prevent infection but cannot be maintained for extensive periods due to economic, educational, and mental health reasons. In the interim, there are numerous vitamins, minerals, supplements, and herbal treatments as well as prescription pharmaceutical interventions which can reduce viral load and address the cytokine storm associated with infection by this disease and lessening the impact on our population. This paper has highlighted how such interventions might work against COVID-19.
References
-
Abe, Y., Hashimoto, S. H. U., & Horie, T. (1999). Curcumin inhibition of inflammatory cytokine production by human peripheral blood monocytes and alveolar macrophages. Pharmacological research, 39(1), 41-47.
-
Aggarwal, B. B., Sundaram, C., Malani, N., & Ichikawa, H. (2007). Curcumin: the Indian solid gold. In The molecular targets and therapeutic uses of curcumin in health and disease (pp. 1-75). Springer, Boston, MA.
-
Al Kassaa, I., Hober, D., Hamze, M., Chihib, N. E., & Drider, D. (2014). Antiviral potential of lactic acid bacteria and their bacteriocins. Probiotics and antimicrobial proteins, 6(3-4), 177-185.
-
Al-Azzawie, H. F., & Alhamdani, M. S. S. (2006). Hypoglycemic and antioxidant effect of oleuropein in alloxan-diabetic rabbits. Life sciences, 78(12), 1371-1377.
-
Abdel-Aziem, S. H., Hassan, A. M., & Abdel-Wahhab, M. A. (2011). Dietary supplementation with whey protein and ginseng extract counteracts oxidative stress and DNA damage in rats fed an aflatoxin-contaminated diet. Mutation Research/Genetic Toxicology and Environmental Mutagenesis, 723(1), 65-71.
-
Albert, R. K., Connett, J., Bailey, W. C., Casaburi, R., Cooper Jr, J. A. D., Criner, G. J., ... & Make, B. (2011). Azithromycin for prevention of exacerbations of COPD. New England Journal of Medicine, 365(8), 689-698.
-
Amoros, M., Simõs, C. M. O., Girre, L., Sauvager, F., & Cormier, M. (1992). Synergistic effect of flavones and flavonols against herpes simplex virus type 1 in cell culture. Comparison with the antiviral activity of propolis. Journal of Natural Products, 55(12), 1732-1740.
-
Andersen, K. G., Rambaut, A., Lipkin, W. I., Holmes, E. C., & Garry, R. F. (2020). The proximal origin of SARS-CoV-2. Nature medicine, 26(4), 450-452.
-
Angeletti, S., Benvenuto, D., Bianchi, M., Giovanetti, M., Pascarella, S., & Ciccozzi, M. (2020). COVID‐2019: The role of the nsp2 and nsp3 in its pathogenesis. Journal of Medical Virology.
-
Antoine, T. E., Mishra, Y. K., Trigilio, J., Tiwari, V., Adelung, R., & Shukla, D. (2012). Prophylactic, therapeutic and neutralizing effects of zinc oxide tetrapod structures against herpes simplex virus type-2 infection. Antiviral research, 96(3), 363-375.
-
Anuradha, C. V., Kaviarasan, S., & Vijayalakshmi, K. (2003). Fenugreek seed polyphenols inhibit RBC membrane Na+/K+-ATPase activity. Oriental Pharmacy and Experimental Medicine, 3(3), 129-132.
-
Associated Press. (2020). China didn’t warn public of likely pandemic for 6 key days. Retrieved from https://apnews.com/68a9e1b91de4ffc166acd6012d82c2f9
-
Asmat, U., Abad, K., & Ismail, K. (2016). Diabetes mellitus and oxidative stress—A concise review. Saudi Pharmaceutical Journal, 24(5), 547-553.
-
Astani, A., Reichling, J., & Schnitzler, P. (2010). Comparative study on the antiviral activity of selected monoterpenes derived from essential oils. Phytotherapy Research: An International Journal Devoted to Pharmacological and Toxicological Evaluation of Natural Product Derivatives, 24(5), 673-679.
-
Arthur, J. R., McKenzie, R. C., & Beckett, G. J. (2003). Selenium in the immune system. The Journal of nutrition, 133(5), 1457S-1459S.
-
Bădescu, S. V., Tătaru, C., Kobylinska, L., Georgescu, E. L., Zahiu, D. M., Zăgrean, A. M., & Zăgrean, L. (2016). The association between diabetes mellitus and depression. Journal of medicine and life, 9(2), 120.
-
Badr, G., Ramadan, N. K., Sayed, L. H., Badr, B. M., Omar, H. M., & Selamoglu, Z. (2017). Why whey? Camel whey protein as a new dietary approach to the management of free radicals and for the treatment of different health disorders. Iranian journal of basic medical sciences, 20(4), 338.
-
Baker, M. (2020). When Did the Coronavirus Arrive in the U.S.? Here’s a Review of the Evidence. Retrieved from https://www.nytimes.com/2020/05/15/us/coronavirus-first-case-snohomish-antibodies.html
-
Balaraman, R., Dangwal, S., & Mohan, M. (2006). Antihypertensive effect of trigonella foenum-greacum. seeds in experimentally induced hypertension in rats. Pharmaceutical biology, 44(8), 568-575.
-
Ballout, R. (2020). The Lysosome: A Potential Therapeutic Juncture between the COVID-19 Pandemic and Niemann-Pick Type C Disease.
-
Banerjee, S., Biehl, A., Gadina, M., Hasni, S., & Schwartz, D. M. (2017). JAK–STAT signaling as a target for inflammatory and autoimmune diseases: current and future prospects. Drugs, 77(5), 521-546.
-
Baradaran, A., Nasri, H., & Rafieian-Kopaei, M. (2014). Oxidative stress and hypertension: Possibility of hypertension therapy with antioxidants. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences, 19(4), 358.
-
Barbaro, M. F., Carpagnano, G. E., Spanevello, A., Cagnazzo, M. G., & Barnes, P. J. (2007). Inflammation, oxidative stress and systemic effects in mild chronic obstructive pulmonary disease. International journal of immunopathology and pharmacology, 20(4), 753-763.
-
Barnes, J., Anderson, L. A., Gibbons, S., & Phillipson, J. D. (2005). Echinacea species (Echinacea angustifolia (DC.) Hell., Echinacea pallida (Nutt.) Nutt., Echinacea purpurea (L.) Moench): a review of their chemistry, pharmacology and clinical properties. Journal of Pharmacy and Pharmacology, 57(8), 929-954.
-
Batlle, D., Soler, M. J., Sparks, M. A., Hiremath, S., South, A. M., Welling, P. A., & Swaminathan, S. (2020). Acute Kidney Injury in COVID-19: Emerging Evidence of a Distinct Pathophysiology. Journal of the American Society of Nephrology.
-
BBC News. (2020). “Coronavirus: Trump Suspends Travel From Europe to US.” BBC. Retrieved from https://www.bbc.com/news/world-us-canada-51846923
-
Beard, J. A., Bearden, A., & Striker, R. (2011). Vitamin D and the anti-viral state. Journal of Clinical Virology, 50(3), 194-200.
-
Beck, M. A. (2001). Selenium as an antiviral agent. In Selenium (pp. 235-245). Springer, Boston, MA.
-
Benavente-Garcıa, O., Castillo, J., Lorente, J., Ortuño, A. D. R. J., & Del Rio, J. A. (2000). Antioxidant activity of phenolics extracted from Olea europaea L. leaves. Food chemistry, 68(4), 457-462.
-
Bergman, P., Lindh, Å. U., Björkhem-Bergman, L., & Lindh, J. D. (2013). Vitamin D and respiratory tract infections: a systematic review and meta-analysis of randomized controlled trials. PloS one, 8(6).
-
Bhatia, M., & Moochhala, S. (2004). Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. The Journal of Pathology: A Journal of the Pathological Society of Great Britain and Ireland, 202(2), 145-156.
-
Bernheim, A., Mei, X., Huang, M., Yang, Y., Fayad, Z. A., Zhang, N., ... & Li, S. (2020). Chest ct findings in coronavirus disease-19 (covid-19): Relationship to duration of infection. Radiology, 200463.
-
Bhanger, M. I., Bukhari, S. B., & Memon, S. (2008). Antioxidative activity of extracts from a Fenugreek seeds (Trigonella foenum-graecum). Pakistan Journal of Analytical & Environmental Chemistry, 9(2), 6.
-
Bhatia, M., & Moochhala, S. (2004). Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. The Journal of Pathology: A Journal of the Pathological Society of Great Britain and Ireland, 202(2), 145-156.
-
Binns, S. E., Hudson, J., Merali, S., & Arnason, J. T. (2002). Antiviral activity of characterized extracts from Echinacea spp.(Heliantheae: Asteraceae) against herpes simplex virus (HSV-I). Planta Medica, 68(09), 780-783.
-
Biot, C., Daher, W., Chavain, N., Fandeur, T., Khalife, J., Dive, D., & De Clercq, E. (2006). Design and synthesis of hydroxyferroquine derivatives with antimalarial and antiviral activities. Journal of medicinal chemistry, 49(9), 2845-2849.
-
Bitetto, D., Fabris, C., Fornasiere, E., Pipan, C., Fumolo, E., Cussigh, A., ... & Martinella, R. (2011). Vitamin D supplementation improves response to antiviral treatment for recurrent hepatitis C. Transplant International, 24(1), 43-50.
-
Black, P. H. (2002). Stress and the inflammatory response: a review of neurogenic inflammation. Brain, behavior, and immunity, 16(6), 622-653.
-
Bonaventura, P., Benedetti, G., Albarède, F., & Miossec, P. (2015). Zinc and its role in immunity and inflammation. Autoimmunity reviews, 14(4), 277-285.
-
Boor, P. P., De Ruiter, P. E., Asmawidjaja, P. S., Lubberts, E., van der Laan, L. J., & Kwekkeboom, J. (2017). JAK-inhibitor tofacitinib suppresses interferon alfa production by plasmacytoid dendritic cells and inhibits arthrogenic and antiviral effects of interferon alfa. Translational Research, 188, 67-79.
-
Borchers, A. T., Selmi, C., Meyers, F. J., Keen, C. L., & Gershwin, M. E. (2009). Probiotics and immunity. Journal of gastroenterology, 44(1), 26-46.
-
Boyera, N., Galey, I., & Bernard, B. A. (1998). Effect of vitamin C and its derivatives on collagen synthesis and cross‐linking by normal human fibroblasts. International journal of cosmetic science, 20(3), 151-158.
-
Brodowska, K. M. (2017). Natural flavonoids: classification, potential role, and application of flavonoid analogues. European Journal of Biological Research, 7(2), 108-123.
-
Buckley, C. (2020). Chinese Doctor, Silenced After Warning of Outbreak, Dies From Coronavirus. Retrieved from https://www.nytimes.com/2020/02/06/world/asia/chinese-doctor-Li-Wenliang-coronavirus.html
-
Buijsse, B., Lee, D. H., Steffen, L., Erickson, R. R., Luepker, R. V., Jacobs Jr, D. R., & Holtzman, J. L. (2012). Low serum glutathione peroxidase activity is associated with increased cardiovascular mortality in individuals with low HDLc’s. PloS one, 7(6).
-
Cairns, R. A., Harris, I. S., & Mak, T. W. (2011). Regulation of cancer cell metabolism. Nature Reviews Cancer, 11(2), 85-95.
-
Cao, B., Wang, Y., Wen, D., Liu, W., Wang, J., Fan, G., ... & Li, X. (2020). A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. New England Journal of Medicine.
-
Cao, W., Shi,L.,Xu, X., & Wu, Z. (2020). Clinical features and laboratory inspection of novel coronavirus pneumonia (COVID-19) in Xiangyang, Hubei. medRxiv.
-
Casadevall, A., & Pirofski, L. A. (2020). The convalescent sera option for containing COVID-19. The Journal of clinical investigation, 130(4), 1545-1548.
-
Cascella, M., Rajnik, M., Cuomo, A., Dulebohn, S. C., & Di Napoli, R. (2020). Features, Evaluation and Treatment Coronavirus (COVID-19). In StatPearls [Internet]. StatPearls Publishing.
-
Centers for Disease Prevention and Control. (March 18, 2020). Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020. Early Release,69.
-
CDC. (2020). Coronavirus Disease 2019 (COVID-19): Cases in U.S. CDC. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
-
Channappanavar, R., Fehr, A. R., Vijay, R., Mack, M., Zhao, J., Meyerholz, D. K., & Perlman, S. (2016). Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell host & microbe, 19(2), 181-193.
-
Charan, J., Goyal, J. P., Saxena, D., & Yadav, P. (2012). Vitamin D for prevention of respiratory tract infections: A systematic review and meta-analysis. Journal of pharmacology & pharmacotherapeutics, 3(4), 300.
-
Chary, M. A., Barbuto, A. F., Izadmehr, S., Hayes, B. D., & Burns, M. M. (2020). COVID-19: therapeutics and their toxicities. J Med Toxicol, 16(3), 10-1007.
-
Chasapis, C. T., Loutsidou, A. C., Spiliopoulou, C. A., & Stefanidou, M. E. (2012). Zinc and human health: an update. Archives of toxicology, 86(4), 521-534.
-
Chaturvedi, P., Ramalingam, N., & Singh, A. (2020). Is COVID-19 man-made?. Cancer Research, Statistics, and Treatment, 3(2), 284.
-
Chen, F., Chan, K. H., Jiang, Y., Kao, R. Y. T., Lu, H. T., Fan, K. W., ... & Guan, Y. (2004). In vitro susceptibility of 10 clinical isolates of SARS coronavirus to selected antiviral compounds. Journal of Clinical Virology, 31(1), 69-75.
-
Chen, C., Huang, J., Cheng, Z., Wu, J., Chen, S., Zhang, Y., ... & Yin, P. (2020). Favipiravir versus Arbidol for COVID-19: a randomized clinical trial. medRxiv.
-
Chen, L., Liu, P., Gao, H., Sun, B., Chao, D., Wang, F., ... & Wang, C. G. (2004). Inhalation of nitric oxide in the treatment of severe acute respiratory syndrome: a rescue trial in Beijing. Clinical infectious diseases, 39(10), 1531-1535.
-
Cheng, Y., Luo, R., Wang, K., Zhang, M., Wang, Z., Dong, L., ... & Xu, G. (2020). Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney International.
-
Chiou, S. Y., Sung, J. M., Huang, P. W., & Lin, S. D. (2017). Antioxidant, antidiabetic, and antihypertensive properties of Echinacea purpurea flower extract and caffeic acid derivatives using in vitro models. Journal of medicinal food, 20(2), 171-179.
-
Chu, C. M., Cheng, V. C. C., Hung, I. F. N., Wong, M. M. L., Chan, K. H., Chan, K. S., ... & Peiris, J. S. M. (2004). Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax, 59(3), 252-256.
-
Chaturvedi, U., Shrivastava, A., Bhadauria, S., Saxena, J. K., & Bhatia, G. (2013). A mechanism-based pharmacological evaluation of efficacy of Trigonella foenum graecum (fenugreek) seeds in regulation of dyslipidemia and oxidative stress in hyperlipidemic rats. Journal of cardiovascular pharmacology, 61(6), 505-512.
-
Clark, J. D., Flanagan, M. E., & Telliez, J. B. (2014). Discovery and development of Janus Kinase (JAK) inhibitors for inflammatory diseases: Miniperspective. Journal of medicinal chemistry, 57(12), 5023-5038.
-
Comalada, M., Ballester, I., Bailon, E., Sierra, S., Xaus, J., Gálvez, J., ... & Zarzuelo, A. (2006). Inhibition of pro-inflammatory markers in primary bone marrow-derived mouse macrophages by naturally occurring flavonoids: analysis of the structure–activity relationship. Biochemical pharmacology, 72(8), 1010-1021.
-
Colson, P., Rolain, J. M., Lagier, J. C., Brouqui, P., & Raoult, D. (2020). Chloroquine and hydroxychloroquine as available weapons to fight COVID-19. Int J Antimicrob Agents, 105932.
-
CRN. (2020). Dietary Supplement Use Reaches All Time High. CRN. Retrieved from https://www.crnusa.org/newsroom/dietary-supplement-use-reaches-all-time-high
-
Corkery, M. & Karni A. (2020). Trump Administration Restricts Entry Into U.S. From China. Retrieved from https://www.nytimes.com/2020/01/31/business/china-travel-coronavirus.html
-
da Costa, S. B., Duarte, C., Bourbon, A. I., Pinheiro, A. C., Serra, A. T., Martins, M. M., ... & da Costa, M. L. B. (2012). Effect of the matrix system in the delivery and in vitro bioactivity of microencapsulated Oregano essential oil. Journal of Food Engineering, 110(2), 190-199.
-
Dai, Q., Zhu, X., Manson, J. E., Song, Y., Li, X., Franke, A. A., ... & Murff, H. (2018). Magnesium status and supplementation influence vitamin D status and metabolism: results from a randomized trial. The American journal of clinical nutrition, 108(6), 1249-1258.
-
Dalton, C. B., Corbett, S. J., & Katelaris, A. L. (2020). Pre-emptive low cost social distancing and enhanced hygiene implemented before local COVID-19 transmission could decrease the number and severity of cases. The Medical Journal of Australia, 212(10), 1.
-
del Rio, C., & Malani, P. N. (2020). COVID-19—new insights on a rapidly changing epidemic. Jama.
-
Dayal, D., & Gupta, S. (2020). Connecting BCG vaccination and COVID-19: additional data. medRxiv.
-
Delang, L., Abdelnabi, R., & Neyts, J. (2018). Favipiravir as a potential countermeasure against neglected and emerging RNA viruses. Antiviral research, 153, 85-94.
-
Deng, X., Yu, X., & Pei, J. (2020). Regulation of interferon production as a potential strategy for COVID-19 treatment. arXiv preprint arXiv:2003.00751.
-
Gates, B. (2020). Responding to Covid-19—A Once-in-a-Century Pandemic?. New England Journal of Medicine.
-
Dewar, M. J. S., & Thiel, W. (1977). J Am Chem Soc 99: 4899;(b) Dewar MJS. Thiel W (1977) J Am Chem Soc, 99, 4907.
-
Derwand, R., & Scholz, M. (2020). Does zinc supplementation enhance the clinical efficacy of chloroquine/hydroxychloroquine to win todays battle against COVID-19?. Medical Hypotheses, 109815.
-
Dholi, S. K., Raparla, R., & Kannappan, S. (2011). Synergic activity of fenugreek seeds and neem leaf extracts against alloxan induced diabetic rats. Int. J. PharmTech Res, 3(4), 1963-1970.
-
Di Liberto, D., Scazzone, C., La Rocca, G., Cipriani, P., Lo Pizzo, M., Ruscitti, P., ... & Triolo, G. (2019). Vitamin D increases the production of IL-10 by regulatory T cells in patients with systemic sclerosis. Clin Exp Rheumatol, 37(119), S76-S81.
-
Dietz, L., Horve, P. F., Coil, D., Fretz, M., & Van Den Wymelenberg, K. (2020). 2019 Novel Coronavirus (COVID-19) Outbreak: A Review of the Current Literature and Built Environment (BE) Considerations to Reduce Transmission.
-
Dong, L., Hu, S., & Gao, J. (2020). Discovering drugs to treat coronavirus disease 2019 (COVID-19). Drug discoveries & therapeutics, 14(1), 58-60.
-
Droge, W. (2002). Free radicals in the physiological control of cell function. Physiological reviews, 82(1), 47-95.
-
Dröge, W., & Holm, E. (1997). Role of cysteine and glutathione in HIV infection and other diseases associated with muscle wasting and immunological dysfunction. The FASEB journal, 11(13), 1077-1089.
-
Ďuračková, Z. (2010). Some current insights into oxidative stress. Physiological research, 59(4).
-
Ebaid, H., Ahmed, O. M., Mahmoud, A. M., & Ahmed, R. R. (2013). Limiting prolonged inflammation during proliferation and remodeling phases of wound healing in streptozotocin-induced diabetic rats supplemented with camel undenatured whey protein. BMC immunology, 14(1), 31.
-
El-Habibi, E. M., El-Wakf, A. M., & Mogall, A. (2013). Efficacy of curcumin in reducing risk of cardiovascular disease in high fat diet-fed rats. Journal of Bioanalysis and Biomedicine, 5, 66-70.
-
Elegant, N. X. (2020). China locks down 3 cities and suspends flights: The latest on the deadly Wuhan virus outbreak. Retrieved from https://fortune.com/2020/01/23/china-wuhan-lockdown-flights-suspended-virus-outbreak/
-
Elfiky, A. A. (2020). Natural products may interfere with SARS-CoV-2 attachment to the host cell. Journal of Biomolecular Structure and Dynamics, (just-accepted), 1-16.
-
Elfiky, A. A. (2020). Anti-HCV, nucleotide inhibitors, repurposing against COVID-19. Life sciences, 117477.
-
Enns, G. M., Moore, T., Le, A., Atkuri, K., Shah, M. K., Cusmano-Ozog, K., ... & Cowan, T. M. (2014). Degree of glutathione deficiency and redox imbalance depend on subtype of mitochondrial disease and clinical status. PloS one, 9(6).
-
Fan, Y. Y., Huang, Z. T., Li, L., Wu, M. H., Yu, T., Koup, R. A., ... & Wu, C. Y. (2009). Characterization of SARS-CoV-specific memory T cells from recovered individuals 4 years after infection. Archives of virology, 154(7), 1093-1099.
-
Esposito, K., Nappo, F., Marfella, R., Giugliano, G., Giugliano, F., Ciotola, M., ... & Giugliano, D. (2002). Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation, 106(16), 2067-2072.
-
Fang, L., Karakiulakis, G., & Roth, M. (2020). Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?. The Lancet Respiratory Medicine.
-
Fankhauser, G. (2020). Delivering High-Quality Vascular Care via Telehealth during the COVID-19 Pandemic. Journal of Vascular Surgery.
-
Fauci, A. S., Lane, H. C., & Redfield, R. R. (2020). Covid-19—navigating the uncharted. The New England Journal of Medicine.
-
Fischer, G. W., Hunter, K. W., Hemming, V. G., & Wilson, S. R. (1983). Functional antibacterial activity of a human intravenous immunoglobulin preparation: in vitro and in vivo studies. Vox sanguinis, 44(5), 296-299.
-
Fosbøl, E. L., Butt, J. H., Østergaard, L., Andersson, C., Selmer, C., Kragholm, K., ... & Torp-Pedersen, C. (2020). Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with COVID-19 diagnosis and mortality. Jama, 324(2), 168-177.
-
Foster, M., & Samman, S. (2010). Zinc and redox signaling: perturbations associated with cardiovascular disease and diabetes mellitus. Antioxidants & redox signaling, 13(10), 1549-1573.
-
Furuta, Y., Gowen, B. B., Takahashi, K., Shiraki, K., Smee, D. F., & Barnard, D. L. (2013). Favipiravir (T-705), a novel viral RNA polymerase inhibitor. Antiviral research, 100(2), 446-454.
-
Fraternale, A., Paoletti, M. F., Casabianca, A., Oiry, J., Clayette, P., Vogel, J. U., ... & Millo, E. (2006). Antiviral and immunomodulatory properties of new pro-glutathione (GSH) molecules. Current medicinal chemistry, 13(15), 1749-1755.
-
Fraternale, A., Paoletti, M. F., Casabianca, A., Nencioni, L., Garaci, E., Palamara, A. T., & Magnani, M. (2009). GSH and analogs in antiviral therapy. Molecular aspects of medicine, 30(1-2), 99-110.
-
Freeman, M. L., Sheridan, B. S., Bonneau, R. H., & Hendricks, R. L. (2007). Psychological stress compromises CD8+ T cell control of latent herpes simplex virus type 1 infections. The Journal of Immunology, 179(1), 322-328.
-
Fusetani, N., Fujita, M., Nakao, Y., Matsunaga, S., & van Soest, R. W. (1999). Tokaramide A, a new cathepsin B inhibitor from the marine sponge Theonella aff. mirabilis. Bioorganic & medicinal chemistry letters, 9(24), 3397-3402.
-
Gackowska, L., Michalkiewicz, J., Krotkiewski, M., Helmin-Basa, A., Kubiszewska, I., & Dzierzanowska, D. (2006). Combined effect of different lactic acid bacteria strains on the mode of cytokines pattern expression in human peripheral blood mononuclear cells. J Physiol Pharmacol, 57(Suppl 9), 13-21.
-
Gammoh, N. Z., & Rink, L. (2017). Zinc in infection and inflammation. Nutrients, 9(6), 624.
-
Gao, J., Tian, Z., & Yang, X. (2020). Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. BioScience Trends.
-
García, C. C., Djavani, M., Topisirovic, I., Borden, K. L., Salvato, M. S., & Damonte, E. B. (2006). Arenavirus Z protein as an antiviral target: virus inactivation and protein oligomerization by zinc finger-reactive compounds. The Journal of general virology, 87(Pt 5), 1217.
-
Garcia‐Ruiz, C., & Fernández‐Checa, J. C. (2007). Redox regulation of hepatocyte apoptosis. Journal of gastroenterology and hepatology, 22, S38-S42.
-
Gautret, P., Lagier, J. C., Parola, P., Meddeb, L., Mailhe, M., Doudier, B., ... & Honoré, S. (2020). Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. International journal of antimicrobial agents, 105949.
-
Gebre‐Medhin, M. E. H. A. R. I., Ewald, U. W. E., Plantin, L. O., & Tuvemo, T. (1984). Elevated serum selenium in diabetic children. Acta Paediatrica, 73(1), 109-114.
-
Giacco, F., & Brownlee, M. (2010). Oxidative stress and diabetic complications. Circulation research, 107(9), 1058-1070.
-
Gilling, D. H., Kitajima, M., Torrey, J. R., & Bright, K. R. (2014). Antiviral efficacy and mechanisms of action of oregano essential oil and its primary component carvacrol against murine norovirus. Journal of applied microbiology, 116(5), 1149-1163.
-
Giustarini, D., Tsikas, D., Colombo, G., Milzani, A., Dalle-Donne, I., Fanti, P., & Rossi, R. (2016). Pitfalls in the analysis of the physiological antioxidant glutathione (GSH) and its disulfide (GSSG) in biological samples: An elephant in the room. Journal of Chromatography B, 1019, 21-28.
-
Gorrini, C., Harris, I. S., & Mak, T. W. (2013). Modulation of oxidative stress as an anticancer strategy. Nature reviews Drug discovery, 12(12), 931-947.
-
Graham, R. E., Gandhi, T. K., Borus, J., Seger, A. C., Burdick, E., Bates, D. W., ... & Weingart, S. N. (2008). Risk of concurrent use of prescription drugs with herbal and dietary supplements in ambulatory care. In Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 4: Technology and Medication Safety). Agency for Healthcare Research and Quality (US).
-
Greiller, C. L., & Martineau, A. R. (2015). Modulation of the immune response to respiratory viruses by vitamin D. Nutrients, 7(6), 4240-4270.
-
Greiwe, J. (2020). Telemedicine in a post-COVID world: How eConsults can be used to augment an allergy practice. The Journal of Allergy and Clinical Immunology. in Practice.
-
Grein, J., Ohmagari, N.,Shin, D., Diaz, G., Asperges, E., Castagna., A., Feldt,T., Green, G., Green., M., Lescure, F., Nicastr, E., & Oda, R. (2020). Compassionate Use of Remdesivir for Patients with Severe Covid-19. New England Journal of Medicine.
-
Griffith, O. W. (1999). Biologic and pharmacologic regulation of mammalian glutathione synthesis. Free Radical Biology and Medicine, 27(9-10), 922-935.
-
Gu, J., & Korteweg, C. (2007). Pathology and pathogenesis of severe acute respiratory syndrome. The American journal of pathology, 170(4), 1136-1147.
-
Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., ... & Du, B. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine.
-
Haberman, R., Axelrad, J., Chen, A., Castillo, R., Yan, D., Izmirly, P., ... & Scher, J. U. (2020). Covid-19 in Immune-Mediated Inflammatory Diseases—Case Series from New York. New England Journal of Medicine.
-
Hackett, R. A., & Steptoe, A. (2016). Psychosocial factors in diabetes and cardiovascular risk. Current cardiology reports, 18(10), 95.
-
Han, X., & Parker, T. L. (2017). Anti-inflammatory, tissue remodeling, immunomodulatory, and anticancer activities of oregano (Origanum vulgare) essential oil in a human skin disease model. Biochimie open, 4, 73-77.
-
Hegarty, P. K., Kamat, A. M., Zafirakis, H., & Dinardo, A. (2020). BCG vaccination may be protective against Covid-19. preprint.
-
Hemming, V. G. (2001). Use of intravenous immunoglobulins for prophylaxis or treatment of infectious diseases. Clin. Diagn. Lab. Immunol., 8(5), 859-863.
-
Heuser, G., & Vojdani, A. (1997). Enhancement of natural killer cell activity and T and B cell function by buffered vitamin C in patients exposed to toxic chemicals: the role of protein kinase-C. Immunopharmacology and immunotoxicology, 19(3), 291-312.
-
Hofmann, S. R., Ettinger, R., Zhou, Y. J., Gadina, M., Lipsky, P., Siegel, R., ... & O'Shea, J. J. (2002). Cytokines and their role in lymphoid development, differentiation and homeostasis. Current opinion in allergy and clinical immunology, 2(6), 495-506.
-
Holshue, M. L., DeBolt, C., Lindquist, S., Lofy, K. H., Wiesman, J., Bruce, H., ... & Diaz, G. (2020). First case of 2019 novel coronavirus in the United States. New England Journal of Medicine.
-
Huang, I. C., Bosch, B. J., Li, F., Li, W., Lee, K. H., Ghiran, S., ... & Farzan, M. (2006). SARS coronavirus, but not human coronavirus NL63, utilizes cathepsin L to infect ACE2-expressing cells. Journal of Biological Chemistry, 281(6), 3198-3203.
-
Huang, L., Zhang, L., Liu, Y., Luo, R., Zeng, L., Telegina, I., & Vlassov, V. V. (2015). Arbidol for preventing and treating influenza in adults and children. Cochrane Database of Systematic Reviews, (1).
-
Hudson, J., Vimalanathan, S., Kang, L., Amiguet, V. T., Livesey, J., & Arnason, J. T. (2005). Characterization of antiviral activities in Echinacea. root preparations. Pharmaceutical biology, 43(9), 790-796.
-
Jarosz, M., Olbert, M., Wyszogrodzka, G., Młyniec, K., & Librowski, T. (2017). Antioxidant and anti-inflammatory effects of zinc. Zinc-dependent NF-κB signaling. Inflammopharmacology, 25(1), 11-24.
-
Johansen, J. S., Harris, A. K., Rychly, D. J., & Ergul, A. (2005). Oxidative stress and the use of antioxidants in diabetes: linking basic science to clinical practice. Cardiovascular diabetology, 4(1), 5.
-
Judge, S., Jang, Y. M., Smith, A., Hagen, T., & Leeuwenburgh, C. (2005). Age-associated increases in oxidative stress and antioxidant enzyme activities in cardiac interfibrillar mitochondria: implications for the mitochondrial theory of aging. The FASEB journal, 19(3), 419-421.
-
Kam, K. Q., Yung, C. F., Cui, L., Lin Tzer Pin, R., Mak, T. M., Maiwald, M., ... & Thoon, K. C. (2020). A well infant with coronavirus disease 2019 (COVID-19) with high viral load. Clinical Infectious Diseases.
-
Kameda, K., Takaku, T., Okuda, H., Kimura, Y., Okuda, T., Hatano, T., ... & Arichi, S. (1987). Inhibitory effects of various flavonoids isolated from leaves of persimmon on angiotensin-converting enzyme activity. Journal of Natural Products, 50(4), 680-683.
-
Kang, M., Zhao, L., Ren, M., Deng, M., & Li, C. (2015). Reduced metallothionein expression induced by zinc deficiency results in apoptosis in hepatic stellate cell line LX-2. International journal of clinical and experimental medicine, 8(11), 20603.
-
Kesic, M. J., Meyer, M., Bauer, R., & Jaspers, I. (2012). Exposure to ozone modulates human airway protease/antiprotease balance contributing to increased influenza A infection. PloS one, 7(4).
-
Khadka, S., Hashmi, F. K., & Usman, M. (2020). Preventing COVID-19 in low-and middle-income countries. Drugs & Therapy Perspectives, 1-3.
-
Kim, H. J., Yoo, H. S., Kim, J. C., Park, C. S., Choi, M. S., Kim, M., ... & Ahn, J. K. (2009). Antiviral effect of Curcuma longa Linn extract against hepatitis B virus replication. Journal of ethnopharmacology, 124(2), 189-196.
-
Kim, M., & Kim, Y. (2010). Hypocholesterolemic effects of curcumin via up-regulation of cholesterol 7a-hydroxylase in rats fed a high fat diet. Nutrition research and practice, 4(3), 191-195.
-
Kim, Y., Kim, H., Bae, S., Choi, J., Lim, S. Y., Lee, N., ... & Lee, W. J. (2013). Vitamin C is an essential factor on the anti-viral immune responses through the production of interferon-α/β at the initial stage of influenza A virus (H3N2) infection. Immune network, 13(2), 70-74.
-
Kinnula, V. L., & Crapo, J. D. (2003). Superoxide dismutases in the lung and human lung diseases. American journal of respiratory and critical care medicine, 167(12), 1600-1619.
-
Kiremidjian-Schumacher, L., & Roy, M. (1998). Selenium and immune function. Zeitschrift fur Ernahrungswissenschaft, 37, 50-56.
-
Khot, W. Y., & Nadkar, M. Y. (2020). The 2019 Novel Coronavirus Outbreak–A Global Threat. Journal of The Association of Physicians of India, 68, 67.
-
Klöcking, R., & Helbig, B. (2005). Humic substances, medical aspects and applications of. Biopolymers Online: Biology• Chemistry• Biotechnology• Applications, 1.
-
Kodama, M., Kodama, T., & Murakami, M. (1994). Vitamin C infusion treatment enhances cortisol production of the adrenal via the pituitary ACTH route. In vivo, 8(6), 1079-1085.
-
Korber, B., Fischer, W., Gnanakaran, S. G., Yoon, H., Theiler, J., Abfalterer, W., ... & Partridge, D. G. (2020). Spike mutation pipeline reveals the emergence of a more transmissible form of SARS-CoV-2. bioRxiv.
-
Krenn, B. M., Gaudernak, E., Holzer, B., Lanke, K., Van Kuppeveld, F. J. M., & Seipelt, J. (2009). Antiviral activity of the zinc ionophores pyrithione and hinokitiol against picornavirus infections. Journal of virology, 83(1), 58-64.
-
Kugelman, A., Choy, H. A., Liu, R., Shi, M. M., Gozal, E., & Forman, H. J. (1994). gamma-Glutamyl transpeptidase is increased by oxidative stress in rat alveolar L2 epithelial cells. American journal of respiratory cell and molecular biology, 11(5), 586-592.
-
Kumar, A., & Zandi, P. (2014). Plant nutraceuticals for cardiovascular diseases with special emphasis to the medicinal herb fenugreek (Trigonella foenum-graecum L.). American Journal of Social Issues and Humanities, 4(3), 177-89.
-
Kwan, J. C., Ratnayake, R., Abboud, K. A., Paul, V. J., & Luesch, H. (2010). Grassypeptolides A− C, cytotoxic bis-thiazoline containing marine cyclodepsipeptides. The Journal of organic chemistry, 75(23), 8012-8023.
-
Lai, A. C. K., Nunayon, S. S., Tan, T. F., & Li, W. S. (2018). A pilot study on the disinfection efficacy of localized UV on the flushing-generated spread of pathogens. Journal of hazardous materials, 358, 389-396.
-
Lee, O., Moon, J., & Chung, Y. (2003). The relationship between serum selenium levels and lipid profiles in adult women. Journal of nutritional science and vitaminology, 49(6), 397-404.
-
Lei, C., Su, B., Dong, H., Bellavia, A., Di Fenza, R., Fakhr, B. S., ... & Pinciroli, R. (2020). Protocol of a randomized controlled trial testing inhaled Nitric Oxide in mechanically ventilated patients with severe acute respiratory syndrome in COVID-19 (SARS-CoV-2). medRxiv.
-
Levy, R., Shriker, O., Porath, A., Riesenberg, K., & Schlaeffer, F. (1996). Vitamin C for the treatment of recurrent furunculosis in patients with impaired neutrophil functions. Journal of Infectious Diseases, 173(6), 1502-1505.
-
Li, M., Yan, K., Wei, L., Yang, J., Lu, C., Xiong, F., ... & Xu, W. (2015). Zinc finger antiviral protein inhibits coxsackievirus B3 virus replication and protects against viral myocarditis. Antiviral research, 123, 50-61.
-
Li, Y., Lin, Z., Guo, M., Xia, Y., Zhao, M., Wang, C., ... & Zhu, B. (2017). Inhibitory activity of selenium nanoparticles functionalized with oseltamivir on H1N1 influenza virus. International journal of nanomedicine, 12, 5733.
-
Li, X., Geng, M., Peng, Y., Meng, L., & Lu, S. (2020). Molecular immune pathogenesis and diagnosis of COVID-19. Journal of Pharmaceutical Analysis.
-
Lippi, G., & Plebani, M. (2020). Laboratory abnormalities in patients with COVID-2019 infection. Clinical Chemistry and Laboratory Medicine (CCLM).
-
Liang, W., Guan, W., Chen, R., Wang, W., Li, J., Xu, K., ... & Li, S. (2020). Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. The Lancet Oncology, 21(3), 335-337.
-
Linington, R. G., Clark, B. R., Trimble, E. E., Almanza, A., Ureña, L. D., Kyle, D. E., & Gerwick, W. H. (2009). Antimalarial peptides from marine cyanobacteria: isolation and structural elucidation of gallinamide A. Journal of natural products, 72(1), 14-17.
-
Liu, J., Manheimer, E., Shi, Y., & Gluud, C. (2004). Chinese herbal medicine for severe acute respiratory syndrome: a systematic review and meta-analysis. Journal of Alternative & Complementary Medicine, 10(6), 1041-1051.
-
Liu, Y. J., Zhan, J., Liu, X. L., Wang, Y., Ji, J., & He, Q. Q. (2014). Dietary flavonoids intake and risk of type 2 diabetes: a meta-analysis of prospective cohort studies. Clinical Nutrition, 33(1), 59-63.
-
Liu, W., & Li, H. (2020). COVID-19 Disease: ORF8 and Surface Glycoprotein Inhibit Heme Metabolism by Binding to Porphyrin.
-
Liu, Y., Gayle, A. A., Wilder-Smith, A., & Rocklöv, J. (2020). The reproductive number of COVID-19 is higher compared to SARS coronavirus. Journal of travel medicine.
-
Luke TC, Kilbane EM, Jackson JL, Hoffman SL. Meta-analysis: convalescent blood products for Spanish influenza pneumonia: a future H5N1 treatment? Ann Intern Med. 2006;145(8):599–609.
-
Luo, H., Tang, Q. L., Shang, Y. X., Liang, S. B., Yang, M., Robinson, N., & Liu, J. P. (2020). Can Chinese medicine be used for prevention of corona virus disease 2019 (COVID-19)? A review of historical classics, research evidence and current prevention programs. Chinese Journal of Integrative Medicine, 1-8.
-
Mak, T. W., Grusdat, M., Duncan, G. S., Dostert, C., Nonnenmacher, Y., Cox, M., ... & Jäger, C. (2017). Glutathione primes T cell metabolism for inflammation. Immunity, 46(4), 675-689.
-
Mangiapane, E., Pessione, A., & Pessione, E. (2014). Selenium and selenoproteins: an overview on different biological systems. Current Protein and Peptide Science, 15(6), 598-607.
-
Mantay, L. (2020). SARS CoV. Researchgate. Retrieved from https://www.researchgate.net/profile/Ludwig_Mantay/publication/340006593_SARS_CoV_2_FV/links/5e72aa8692851c93e0ad4815/SARS-CoV-2-FV.pdf. Accessed 2 April 2020.
-
Maras, D. (2019). Adverse childhood experiences: Traumas that set the framework for life. Clinical Corner Time2Track Blog Post.
-
Maret, W. (1995). Metallothionein/disulfide interactions, oxidative stress, and the mobilization of cellular zinc. Neurochemistry international, 27(1), 111-117.
-
Marik, P. E. (2020). Vitamin C: an essential “stress hormone” during sepsis. Journal of Thoracic Disease, 12(Suppl 1), S84.
-
Martineau, A. R., Jolliffe, D. A., Hooper, R. L., Greenberg, L., Aloia, J. F., Bergman, P., ... & Goodall, E. C. (2017). Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. bmj, 356, i6583.
-
Maywald, M., Wessels, I., & Rink, L. (2017). Zinc signals and immunity. International journal of molecular sciences, 18(10), 2222.
-
McCord, J. M., & Fridovich, I. (1969). Superoxide dismutase an enzymic function for erythrocuprein (hemocuprein). Journal of Biological chemistry, 244(22), 6049-6055.
-
Mclntosh, K., Hirsch,M.S., & Bloom, A. (2020). Coronavirus disease 2019 (COVID-19). UpToDate. Retrieved from https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19
-
Meerbach, A., Neyts, J., Balzarini, J., Helbig, B., De Clercq, E., & Wutzler, P. (2001). In vitro activity of polyhydroxycarboxylates against herpesviruses and HIV. Antiviral Chemistry and Chemotherapy, 12(6), 337-345.
-
Mehta, P., McAuley, D. F., Brown, M., Sanchez, E., Tattersall, R. S., & Manson, J. J. (2020). COVID-19: consider cytokine storm syndromes and immunosuppression. The Lancet.
-
Memısoğullari, R., Taysı, S., Bakan, E., & Capoglu, I. (2003). Antioxidant status and lipid peroxidation in type II diabetes mellitus. Cell Biochemistry and Function: Cellular biochemistry and its modulation by active agents or disease, 21(3), 291-296.
-
Michot, J. M., Albiges, L., Chaput, N., Saada, V., Pommeret, F., Griscelli, F., ... & Merad, M. (2020). Tocilizumab, an anti-IL6 receptor antibody, to treat Covid-19-related respiratory failure: a case report. Annals of Oncology.
-
Micol, V., Caturla, N., Pérez-Fons, L., Más, V., Pérez, L., & Estepa, A. (2005). The olive leaf extract exhibits antiviral activity against viral haemorrhagic septicaemia rhabdovirus (VHSV). Antiviral research, 66(2-3), 129-136.
-
Miller, A., Reandelar, M. J., Fasciglione, K., Roumenova, V., Li, Y., & Otazu, G. H. (2020). Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiological study. MedRxiv.
-
Miller, B., Friedman, A. J., Choi, H., Hogan, J., McCammon, J. A., Hook, V., & Gerwick, W. H. (2014). The marine cyanobacterial metabolite gallinamide A is a potent and selective inhibitor of human cathepsin L. Journal of natural products, 77(1), 92-99.
-
Minelli, A., Bellezza, I., Conte, C., & Culig, Z. (2009). Oxidative stress-related aging: a role for prostate cancer?. Biochimica et Biophysica Acta (BBA)-Reviews on Cancer, 1795(2), 83-91.
-
Minich, D. M., & Brown, B. I. (2019). A review of dietary (Phyto) nutrients for glutathione support. Nutrients, 11(9), 2073.
-
Mishima, S., Saito, K., Maruyama, H., Inoue, M., Yamashita, T., Ishida, T., & Gu, Y. (2004). Antioxidant and immuno-enhancing effects of Echinacea purpurea. Biological and Pharmaceutical Bulletin, 27(7), 1004-1009.
-
Miyara, M., Tubach, F., Pourcher, V., Morelot-Panzini, C., Pernet, J., & Haroche, J. (2020). Low incidence of daily active tobacco smoking in patients with symptomatic COVID-19. Q eios.
-
Modestou, M. A., Manzel, L. J., El-Mahdy, S., & Look, D. C. (2010). Inhibition of IFN-γ-dependent antiviral airway epithelial defense by cigarette smoke. Respiratory research, 11(1), 64.
-
Molina, J. M., Delaugerre, C., Goff, J. L., Mela-Lima, B., Ponscarme, D., Goldwirt, L., & de Castro, N. (2020). No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine and azithromycin in patients with severe COVID-19 infection. Med Mal Infect, 30085-8.
-
Morera, L. P. P., Marchiori, G. N., Medrano, L. A., & Defagó, M. D. (2019). Stress, dietary patterns and cardiovascular disease: a Mini-Review. Frontiers in neuroscience, 13, 1226.
-
Morgenstern, B., Michaelis, M., Baer, P. C., Doerr, H. W., & Cinatl Jr, J. (2005). Ribavirin and interferon-β synergistically inhibit SARS-associated coronavirus replication in animal and human cell lines. Biochemical and biophysical research communications, 326(4), 905-908.
-
Morita, H., He, F., Fuse, T., Ouwehand, A. C., Hashimoto, H., Hosoda, M., ... & Kurisaki, J. I. (2002). Adhesion of lactic acid bacteria to Caco‐2 cells and their effect on cytokine secretion. Microbiology and immunology, 46(4), 293-297.
-
Mousavi, S., Bereswill, S., & Heimesaat, M. M. (2019). Immunomodulatory and antimicrobial effects of vitamin C. European Journal of Microbiology and Immunology, 9(3), 73-79.
-
Muda, P., Kampus, P., Zilmer, M., Zilmer, K., Kairane, C., Ristimäe, T., ... & Teesalu, R. (2003). Homocysteine and red blood cell glutathione as indices for middle-aged untreated essential hypertension patients. Journal of hypertension, 21(12), 2329-2333.
-
Muller, U., Steinhoff, U., Reis, L. F., Hemmi, S., Pavlovic, J., Zinkernagel, R. M., & Aguet, M. (1994). Functional role of type I and type II interferons in antiviral defense. Science, 264(5167), 1918-1921.
-
Nabirotchkin, S., Peluffo, A. E., Bouaziz, J., & Cohen, D. (2020). Focusing on the unfolded protein response and autophagy related pathways to reposition common approved drugs against COVID-19.
-
Nagai, T., Suzuki, Y., Tomimori, T., & Yamada, H. (1995). Antiviral activity of plant flavonoid, 5, 7, 4'-trihydroxy-8-methoxyflavone, from the roots of Scutellaria baicalensis against influenza A (H3N2) and B viruses. Biological and Pharmaceutical Bulletin, 18(2), 295-299.
-
Nagata, M. (2005). Inflammatory cells and oxygen radicals. Current Drug Targets-Inflammation & Allergy, 4(4), 503-504.
-
Nasser, E. H., Judd, A. K., Sanchez, A., Anastasiou, D., & Bucher, D. J. (1996). Antiviral activity of influenza virus M1 zinc finger peptides. Journal of virology, 70(12), 8639-8644.
-
National Institute of Health. (2020). Magnesium: Fact Sheet for Health Professionals. NIH. Retrieved from https://ods.od.nih.gov/factsheets/Magnesium-Consumer/
-
National Institute of Health. (2020). Vitamin C: Fact Sheet for Health Professionals. NIH. Retrieved from https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/#en19
-
National Institute of Health. (2020). Vitamin D: Fact Sheet for Health Professionals. NIH. Retrieved from https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
-
National Institute of Health. (2020). Zinc: Fact Sheet for Health Professionals. NIH. Retrieved from https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/
-
National Institute of Health. (2020). Selenium: Fact Sheet for Health Professionals. NIH. Retrieved from https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/#en51
-
Netea, M. G., Domínguez-Andrés, J., Barreiro, L. B., Chavakis, T., Divangahi, M., Fuchs, E., ... & Riksen, N. P. (2020). Defining trained immunity and its role in health and disease. Nature Reviews Immunology, 1-14.
-
Newhouse, I. J., & Finstad, E. W. (2000). The effects of magnesium supplementation on exercise performance. Clinical Journal of Sport Medicine, 10(3), 195-200.
-
Ni, L., Zhou, L., Zhou, M., Zhao, J., & Wang, D. W. (2020). Combination of western medicine and Chinese traditional patent medicine in treating a family case of COVID-19 in Wuhan. Frontiers of Medicine, 1-5.
-
Niemeyer, D., Zillinger, T., Muth, D., Zielecki, F., Horvath, G., Suliman, T., ... & Müller, M. A. (2013). Middle East respiratory syndrome coronavirus accessory protein 4a is a type I interferon antagonist. Journal of virology, 87(22), 12489-12495.
-
Padayatty, S. J., Katz, A., Wang, Y., Eck, P., Kwon, O., Lee, J. H., ... & Levine, M. (2003). Vitamin C as an antioxidant: evaluation of its role in disease prevention. Journal of the American college of Nutrition, 22(1), 18-35.
-
Pandey, H., & Awasthi, P. (2015). Effect of processing techniques on nutritional composition and antioxidant activity of fenugreek (Trigonella foenum-graecum) seed flour. Journal of food science and technology, 52(2), 1054-1060.
-
Patel, S. (2015). Emerging trends in nutraceutical applications of whey protein and its derivatives. Journal of food science and technology, 52(11), 6847-6858.
-
Pardanani, A., Harrison, C., Cortes, J. E., Cervantes, F., Mesa, R. A., Milligan, D., ... & Drummond, M. W. (2015). Safety and efficacy of fedratinib in patients with primary or secondary myelofibrosis: a randomized clinical trial. JAMA oncology, 1(5), 643-651.
-
Pastori, G. M., & Trippi, V. S. (1992). Oxidative stress induces high rate of glutathione reductase synthesis in a drought-resistant maize strain. Plant and cell Physiology, 33(7), 957-961.
-
Pfeffer, P. E., & Hawrylowicz, C. M. (2012). Vitamin D and lung disease. Thorax, 67(11), 1018-1020.
-
Patterson, B. K., Seethamraju, H., Dhody, K., Corley, M. J., Kazempour, K., Lalezari, J. P., ... & Rodrigues, H. (2020). Disruption of the CCL5/RANTES-CCR5 Pathway Restores Immune Homeostasis and Reduces Plasma Viral Load in Critical COVID-19. medRxiv.
-
Peterson, P. K., Chao, C. C., Molitor, T., Murtaugh, M., Strgar, F., & Sharp, B. M. (1991). Stress and pathogenesis of infectious disease. Reviews of infectious diseases, 13(4), 710-720.
-
Piscitelli, S. C., Danziger, L. H., & Rodvold, K. A. (1992). Clarithromycin and azithromycin: new macrolide antibiotics. Clinical pharmacy, 11(2), 137-152.
-
Pizzino, G., Irrera, N., Cucinotta, M., Pallio, G., Mannino, F., Arcoraci, V., ... & Bitto, A. (2017). Oxidative stress: harms and benefits for human health. Oxidative medicine and cellular longevity, 2017.
-
Poyton, R. O., Ball, K. A., & Castello, P. R. (2009). Mitochondrial generation of free radicals and hypoxic signaling. Trends in Endocrinology & Metabolism, 20(7), 332-340.
-
Prajapat, M., Sarma, P., Shekhar, N., Avti, P., Sinha, S., Kaur, H., ... & Medhi, B. (2020). Drug targets for corona virus: A systematic review. Indian Journal of Pharmacology, 52(1), 56.
-
Prompetchara, E., Ketloy, C., & Palaga, T. (2020). Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pacific J. allergy Immunol, 10.
-
Praveen, D., Chowdary, P. R., & Aanandhi, M. V. (2020). Baricitinib-a Januase Kinase Inhibitor-Not an Ideal Option for Management of Covid 19. International Journal of Antimicrobial Agents.
-
Pryor, W. A., & Squadrito, G. L. (1995). The chemistry of peroxynitrite: a product from the reaction of nitric oxide with superoxide. American Journal of Physiology-Lung Cellular and Molecular Physiology, 268(5), L699-L722.
-
Pujadas, E., Chaudhry, F., McBride, R., Richter, F., Zhao, S., Wajnberg, A., ... & Cordon-Cardo, C. (2020). SARS-CoV-2 Viral Load Predicts COVID-19 Mortality. medRxiv.
Qin, A. & Wang, V. (2020). Wuhan, Center of Coronavirus Outbreak, Is Being Cut Off by Chinese Authorities. Retrieved from https://www.nytimes.com/2020/01/22/world/asia/china-coronavirus-travel.html -
Rains, J. L., & Jain, S. K. (2011). Oxidative stress, insulin signaling, and diabetes. Free Radical Biology and Medicine, 50(5), 567-575.
-
Rees, K., Hartley, L., Day, C., Flowers, N., Clarke, A., & Stranges, S. (2013). Selenium supplementation for the primary prevention of cardiovascular disease. Cochrane Database of Systematic Reviews, (1).
-
Ren, J. L., Zhang, A. H., & Wang, X. J. (2020). Traditional Chinese medicine for COVID-19 treatment. Pharmacological research, 155, 104743.
-
Reuter, S., Gupta, S. C., Chaturvedi, M. M., & Aggarwal, B. B. (2010). Oxidative stress, inflammation, and cancer: how are they linked?. Free radical biology and medicine, 49(11), 1603-1616.
-
Reynard, O., Nguyen, X. N., Alazard-Dany, N., Barateau, V., Cimarelli, A., & Volchkov, V. E. (2015). Identification of a new ribonucleoside inhibitor of Ebola virus replication. Viruses, 7(12), 6233-6240.
-
Richardson, P., Griffin, I., Tucker, C., Smith, D., Oechsle, O., Phelan, A., & Stebbing, J. (2020). Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet (London, England), 395(10223), e30.
-
Richie Jr, J. P., Muscat, J. E., Ellison, I., Calcagnotto, A., Kleinman, W., & El-Bayoumy, K. (2011). Association of selenium status and blood glutathione concentrations in blacks and whites. Nutrition and cancer, 63(3), 367-375.
-
Robaczewska, J., Kedziora-Kornatowska, K., Kozakiewicz, M., Zary-Sikorska, E., Pawluk, H., Pawliszak, W., & Kedziora, J. (2016). Role of glutathione metabolism and glutathione-related antioxidant defense systems in hypertension. J Physiol Pharmacol, 67(3), 331-337.
-
Romero, J. C., & Reckelhoff, J. F. (1999). Role of angiotensin and oxidative stress in essential hypertension. Hypertension, 34(4), 943-949.
-
Rondanelli, M., Miccono, A., Lamburghini, S., Avanzato, I., Riva, A., Allegrini, P., ... & Perna, S. (2018). Self-care for common colds: the pivotal role of vitamin D, vitamin C, zinc, and Echinacea in three main immune interactive clusters (physical barriers, innate and adaptive immunity) involved during an episode of common colds—Practical advice on dosages and on the time to take these nutrients/botanicals in order to prevent or treat common colds. Evidence-Based Complementary and Alternative Medicine, 2018.
-
Rosanoff, A., Dai, Q., & Shapses, S. A. (2016). Essential nutrient interactions: does low or suboptimal magnesium status interact with vitamin D and/or calcium status?. Advances in nutrition, 7(1), 25-43.
-
Rosenberg, E. S., Dufort, E. M., Udo, T., Wilberschied, L. A., Kumar, J., Tesoriero, J., ... & Blog, D. S. (2020). Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA.
-
Rothe, C., Schunk, M., Sothmann, P., Bretzel, G., Froeschl, G., Wallrauch, C., ... & Seilmaier, M. (2020). Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. New England Journal of Medicine.
-
Russel, T., Hellewell, J., & Abbot, S. (2020). Using a delay-adjusted case fatality ratio to estimate under-reporting. Available at the Centre for Mathematical Modelling of Infectious Diseases Repository, here.
-
Sato, M., Yanagisawa, H., Nojima, Y., Tamura, J., & Wada, O. (2002). Zn deficiency aggravates hypertension in spontaneously hypertensive rats: possible role of Cu/Zn-superoxide dismutase. Clinical and experimental hypertension, 24(5), 355-370.
-
Schito, M. L., Goel, A., Song, Y., Inman, J. K., Fattah, R. J., Rice, W. G., ... & Appella, E. (2003). In vivo antiviral activity of novel human immunodeficiency virus type 1 nucleocapsid p7 zinc finger inhibitors in a transgenic murine model. AIDS research and human retroviruses, 19(2), 91-101.
-
Schrezenmeier, E., & Dörner, T. (2020). Mechanisms of action of hydroxychloroquine and chloroquine: implications for rheumatology. Nature Reviews Rheumatology, 1-12.
-
Sekhar, R. V., McKay, S. V., Patel, S. G., Guthikonda, A. P., Reddy, V. T., Balasubramanyam, A., & Jahoor, F. (2011). Glutathione synthesis is diminished in patients with uncontrolled diabetes and restored by dietary supplementation with cysteine and glycine. Diabetes care, 34(1), 162-167.
-
Shaik-Dasthagirisaheb, Y. B., Varvara, G., Murmura, G., Saggini, A., Caraffa, A., Antinolfi, P., ... & Toniato, E. (2013). Role of vitamins D, E and C in immunity and inflammation. J Biol Regul Homeost Agents, 27(2), 291-295.
-
Sharma, M., Anderson, S. A., Schoop, R., & Hudson, J. B. (2009). Induction of multiple pro-inflammatory cytokines by respiratory viruses and reversal by standardized Echinacea, a potent antiviral herbal extract. Antiviral Research, 83(2), 165-170.
-
Sheahan, T. P., Sims, A. C., Zhou, S., Graham, R. L., Pruijssers, A. J., Agostini, M. L., ... & Chappell, J. D. (2020). An orally bioavailable broad-spectrum antiviral inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice. Science translational medicine, 12(541).
-
Shittu, M. O., & Afolami, O. I. (2020). Improving the efficacy of chloroquine and hydroxychloroquine against SARS-CoV-2 may require zinc additives-A better synergy for future COVID-19 clinical trials. Le Infezioni in Medicina, 28(2), 192-197.
-
Silva, F. V., Guimaraes, A. G., Silva, E. R., Sousa-Neto, B. P., Machado, F. D., Quintans-Júnior, L. J., ... & Oliveira, R. C. (2012). Anti-inflammatory and anti-ulcer activities of carvacrol, a monoterpene present in the essential oil of oregano. Journal of medicinal food, 15(11), 984-991.
-
Simmons, G., Gosalia, D. N., Rennekamp, A. J., Reeves, J. D., Diamond, S. L., & Bates, P. (2005). Inhibitors of cathepsin L prevent severe acute respiratory syndrome coronavirus entry. Proceedings of the National Academy of Sciences, 102(33), 11876-11881.
-
Shi, Y., Tan, M., Chen, X., Liu, Y., Huang, J., Ou, J., & Deng, X. (2020). Immunopathological characteristics of coronavirus disease 2019 cases in Guangzhou, China. medRxiv.
-
Shamseer, L., Moher, D., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., ... & Stewart, L. A. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj, 349.
-
Shanley, P. F. (1996, January). The pathology of chronic renal ischemia. In Seminars in nephrology (Vol. 16, No. 1, pp. 21-32).
-
Siddiqui, Y. M., Ettayebi, M., Haddad, M. D. L., Ahdal, M. N., & Haddad, A. E. (1996). Effect of essential oils on the enveloped viruses: antiviral activity of oregano and clove oils on herpes simplex virus type 1 and Newcastle disease virus.
-
Singh, S., Sharma, N., Singh, U., Singh, T., Mangal, D. K., & Singh, V. (2020). Nasopharyngeal wash in preventing and treating upper respiratory tract infections: Could it prevent COVID-19?. Lung India, 37(3), 246.
-
Simon, A. K., Hollander, G. A., & McMichael, A. (2015). Evolution of the immune system in humans from infancy to old age. Proceedings of the Royal Society B: Biological Sciences, 282(1821), 20143085.
-
Simmons, G., Gosalia, D. N., Rennekamp, A. J., Reeves, J. D., Diamond, S. L., & Bates, P. (2005). Inhibitors of cathepsin L prevent severe acute respiratory syndrome coronavirus entry. Proceedings of the National Academy of Sciences, 102(33), 11876-11881.
-
Snijder, E. J., Van Der Meer, Y., Zevenhoven-Dobbe, J., Onderwater, J. J., van der Meulen, J., Koerten, H. K., & Mommaas, A. M. (2006). Ultrastructure and origin of membrane vesicles associated with the severe acute respiratory syndrome coronavirus replication complex. Journal of virology, 80(12), 5927-5940.
-
Song, J. Y., Cheong, H. J., Hwang, I. S., Choi, W. S., Jo, Y. M., Park, D. W., ... & Kim, W. J. (2010). Long-term immunogenicity of influenza vaccine among the elderly: risk factors for poor immune response and persistence. Vaccine, 28(23), 3929-3935.
-
Sousa, G. T., Lira, F. S., Rosa, J. C., de Oliveira, E. P., Oyama, L. M., Santos, R. V., & Pimentel, G. D. (2012). Dietary whey protein lessens several risk factors for metabolic diseases: a review. Lipids in health and disease, 11(1), 67.
-
Sparrenberger, F., Cichelero, F. T., Ascoli, A. M., Fonseca, F. P., Weiss, G., Berwanger, O., ... & Fuchs, F. D. (2009). Does psychosocial stress cause hypertension? A systematic review of observational studies. Journal of human hypertension, 23(1), 12-19.
-
Stacey, F. G., James, E. L., Chapman, K., Courneya, K. S., & Lubans, D. R. (2015). A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. Journal of Cancer Survivorship, 9(2), 305-338.
-
Stebbing, J., Phelan, A., Griffin, I., Tucker, C., Oechsle, O., Smith, D., & Richardson, P. (2020). COVID-19: combining antiviral and anti-inflammatory treatments. The Lancet Infectious Diseases.
-
Zinc: a multipurpose trace element.
-
Stefanidou, M., Maravelias, C., Dona, A., & Spiliopoulou, C. (2006). Zinc: a multipurpose trace element. Archives of toxicology, 80(1), 1.
-
Stockman, L. J., Bellamy, R., & Garner, P. (2006). SARS: systematic review of treatment effects. PLoS medicine, 3(9).
-
Stone, W. L., Scott, R. L., Stewart, E. M., & Kheshti, A. (1994). Lipoprotein alterations in the spontaneously hypertensive rat fed diets deficient in selenium and vitamin E. Proceedings of the Society for Experimental Biology and Medicine, 206(2), 130-137.
-
Strohle, A., Wolters, M., & Hahn, A. (2011). Micronutrients at the interface between inflammation and infection ascorbic acid and calciferol. Part 1: general overview with a focus on ascorbic acid. Inflammation & Allergy-Drug Targets (Formerly Current Drug Targets-Inflammation & Allergy), 10(1), 54-63.
-
Swanson, C. M., Nielson, C. M., Shrestha, S., Lee, C. G., Barrett-Connor, E., Jans, I., ... & Orwoll, E. S. (2014). Higher 25 (OH) D2 is associated with lower 25 (OH) D3 and 1, 25 (OH) 2D3. The Journal of Clinical Endocrinology & Metabolism, 99(8), 2736-2744.
-
Tabares, P., Degel, B., Schaschke, N., Hentschel, U., & Schirmeister, T. (2012). Identification of the protease inhibitor miraziridine A in the Red sea sponge Theonella swinhoei. Pharmacognosy research, 4(1), 63.
-
Tait, S., Salvati, A. L., Desideri, N., & Fiore, L. (2006). Antiviral activity of substituted homoisoflavonoids on enteroviruses. Antiviral research, 72(3), 252-255.
-
Talpur, N., Echard, B., Ingram, C., Bagchi, D., & Preuss, H. (2005). Effects of a novel formulation of essential oils on glucose–insulin metabolism in diabetic and hypertensive rats: a pilot study. Diabetes, Obesity and Metabolism, 7(2), 193-199.
-
Tanaka, T., Narazaki, M., & Kishimoto, T. (2016). Immunotherapeutic implications of IL-6 blockade for cytokine storm. Immunotherapy, 8(8), 959-970.
-
Tanenbaum, L., & Tuffanelli, D. L. (1980). Antimalarial agents: chloroquine, hydroxychloroquine, and quinacrine. Archives of dermatology, 116(5), 587-591.
-
Tchesnokov, E. P., Feng, J. Y., Porter, D. P., & Götte, M. (2019). Mechanism of inhibition of Ebola virus RNA-dependent RNA polymerase by remdesivir. Viruses, 11(4), 326.
-
Te Velthuis, A. J., van den Worm, S. H., Sims, A. C., Baric, R. S., Snijder, E. J., & van Hemert, M. J. (2010). Zn2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS pathogens, 6(11).
-
Teskey, G., Abrahem, R., Cao, R., Gyurjian, K., Islamoglu, H., Lucero, M., ... & Venketaraman, V. (2018). Glutathione as a marker for human disease. In Advances in clinical chemistry (Vol. 87, pp. 141-159). Elsevier.
-
Touret, F., & de Lamballerie, X. (2020). Of chloroquine and COVID-19. Antiviral Research, 104762.
-
van Doremalen, N., Bushmaker, T., Morris, D. H., Holbrook, M. G., Gamble, A., Williamson, B. N., ... & Lloyd-Smith, J. O. (2020). Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine.
-
Touyz, R. M., & Briones, A. M. (2011). Reactive oxygen species and vascular biology: implications in human hypertension. Hypertension research, 34(1), 5-14.
-
Urakova, N., Kuznetsova, V., Crossman, D. K., Sokratian, A., Guthrie, D. B., Kolykhalov, A. A., ... & Frolova, E. I. (2018). β-D-N4-Hydroxycytidine is a potent anti-alphavirus compound that induces a high level of mutations in the viral genome. Journal of virology, 92(3), e01965-17.
-
Vaira, L. A., Salzano, G., Deiana, G., & De Riu, G. (2020). Anosmia and ageusia: common findings in COVID-19 patients. The Laryngoscope.
-
Vardavas, C. I., & Nikitara, K. (2020). COVID-19 and smoking: A systematic review of the evidence. Tobacco induced diseases, 18.
-
Vidal-Albalat, A., & González, F. V. (2016). Natural Products as Cathepsin Inhibitors. In Studies in Natural Products Chemistry (Vol. 50, pp. 179-213). Elsevier.
-
Volpe, S. L. (2013). Magnesium in disease prevention and overall health. Advances in nutrition, 4(3), 378S-383S.
-
Wan, Y., Shang, J., Graham, R., Baric, R. S., & Li, F. (2020). Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. Journal of virology, 94(7).
-
Wang, D., Hu, B., Hu, C., Zhu, F., Liu, X., Zhang, J., ... & Zhao, Y. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama.
-
Wang, J., Luo, Q., Chen, R., Chen, T., & Li, J. (2020). Susceptibility Analysis of COVID-19 in Smokers Based on ACE2.
-
Wang, H., Yang, P., Liu, K., Guo, F., Zhang, Y., Zhang, G., & Jiang, C. (2008). SARS coronavirus entry into host cells through a novel clathrin-and caveolae-independent endocytic pathway. Cell research, 18(2), 290-301.
-
Wang, M., Cao, R., Zhang, L., Yang, X., Liu, J., Xu, M., ... & Xiao, G. (2020). Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell research, 30(3), 269-271.
-
Wang, X. L., Yang, T. B., Wei, J., Lei, G. H., & Zeng, C. (2015). Association between serum selenium level and type 2 diabetes mellitus: a non-linear dose–response meta-analysis of observational studies. Nutrition journal, 15(1), 48.
-
Wang, X., Dhindsa, R., Povysil, G., Zoghbi, A., Motelow, J., Hostyk, J., & Goldstein, D. (2020). Transcriptional Inhibition of Host Viral Entry Proteins as a Therapeutic Strategy for SARS-CoV-2.
-
Wang, Z., Li, L., Yan, J., & Yao, Y. (2020). Evaluating the Traditional Chinese Medicine (TCM) Officially Recommended in China for COVID-19 Using Ontology-Based Side-Effect Prediction Framework (OSPF) and Deep Learning.
-
Weinkove, R., McQuilten, Z., Adler, J., Agar, M., Blyth, E., Cheng, A., ... & Lane, S. (2020). Managing haematology and oncology patients during the COVID-19 pandemic: interim consensus guidance. The Medical Journal of Australia, 212(10), 1.
-
Winkler, J., & Ghosh, S. (2018). Therapeutic potential of fulvic acid in chronic inflammatory diseases and diabetes. Journal of diabetes research, 2018.
-
Wintergerst, E. S., Maggini, S., & Hornig, D. H. (2006). Immune-enhancing role of vitamin C and zinc and effect on clinical conditions. Annals of Nutrition and Metabolism, 50(2), 85-94.
-
WHO. (2019). Naming the Coronavirus Disease (COVID-19) and the Virus that Causes it. World Health Organization. Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it
-
WHO. (2020). “Updated WHO Advice for in Relation to the Outbreak of the Novel Coronavirus 2019-nCoV”. Retrieved from https://www.who.int/news-room/articles-detail/updated-who-advice-for-international-traffic-in-relation-to-the-outbreak-of-the-novel-coronavirus-2019-ncov-24-jan/
-
WHO. (2020). “Who Advice for International Travel And Trade in Relation To The Outbreak of Pneumonia caused by a new Coronavirus In China.” Retrieved from https://www.who.int/news-room/articles-detail/who-advice-for-international-travel-and-trade-in-relation-to-the-outbreak-of-pneumonia-caused-by-a-new-coronavirus-in-china
-
Wong, T. Y., Klein, R., Klein, B. E., Tielsch, J. M., Hubbard, L., & Nieto, F. J. (2001). Retinal microvascular abnormalities and their relationship with hypertension, cardiovascular disease, and mortality. Survey of ophthalmology, 46(1), 59-80.
-
Workinger, J. L., Doyle, R., & Bortz, J. (2018). Challenges in the diagnosis of magnesium status. Nutrients, 10(9), 1202.
-
Wu, D., & Cederbaum, A. I. (2003). Alcohol, oxidative stress, and free radical damage. Alcohol Research & Health, 27(4), 277.
-
Wu, G., Fang, Y. Z., Yang, S., Lupton, J. R., & Turner, N. D. (2004). Glutathione metabolism and its implications for health. The Journal of nutrition, 134(3), 489-492.
-
Wu, Y. C., Chen, C. S., & Chan, Y. J. (2020). The outbreak of COVID-19: An overview. Journal of the Chinese Medical Association, 83(3), 217.
-
Xia, J., Liu, X., Chen, H., Shang, Y., Zhu, H., Chen, G., ... & Hong, Z. (2020). Efficacy of Chloroquine and Lopinavir/Ritonavir in mild/general COVID-2019: a prospective, open-label, multicenter randomized controlled clinical study.
-
Xia, Y., Jin, R., Zhao, J., Li, W., & Shen, H. (2020). Risk of COVID-19 for cancer patients. The Lancet Oncology.
-
Xu, X., Han, M., Li, T., Sun, W., Wang, D., Fu, B., ... & Zhang, X. (2020). Effective treatment of severe COVID-19 patients with tocilizumab. ChinaXiv, 202003(00026), V1.
-
Yamamoto, M., Matsuyama, S., Li, X., Takeda, M., Kawaguchi, Y., Inoue, J. I., & Matsuda, Z. (2016). Identification of nafamostat as a potent inhibitor of Middle East respiratory syndrome coronavirus S protein-mediated membrane fusion using the split-protein-based cell-cell fusion assay. Antimicrobial agents and chemotherapy, 60(11), 6532-6539.
-
Yan, T., Li, S., Jiang, X., & Oberley, L. W. (1999). Altered levels of primary antioxidant enzymes in progeria skin fibroblasts. Biochemical and biophysical research communications, 257(1), 163-167.
-
Yang, G., & Chen, D. (2008). Biflavanones, flavonoids, and coumarins from the roots of Stellera chamaejasme and their antiviral effect on hepatitis B virus. Chemistry & biodiversity, 5(7), 1419-1424.
-
Yang, J., Zheng, Y., Gou, X., Pu, K., Chen, Z., Guo, Q., ... & Zhou, Y. (2020). Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. International Journal of Infectious Diseases, 94, 91.
-
Yang, X., Yu, Y., Xu, J., Shu, H., Liu, H., Wu, Y., ... & Wang, Y. (2020). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. The Lancet Respiratory Medicine.
-
Yang, Y., Islam, M. S., Wang, J., Li, Y., & Chen, X. (2020). Traditional Chinese medicine in the treatment of patients infected with 2019-new coronavirus (SARS-CoV-2): a review and perspective. International journal of biological sciences, 16(10), 1708.
-
Yang, Y., Zhang, L., Geng, H., Deng, Y., Huang, B., Guo, Y., ... & Tan, W. (2013). The structural and accessory proteins M, ORF 4a, ORF 4b, and ORF 5 of Middle East respiratory syndrome coronavirus (MERS-CoV) are potent interferon antagonists. Protein & cell, 4(12), 951-961.
-
Yokota, S., Miyamae, T., Imagawa, T., Iwata, N., Katakura, S., Mori, M., ... & Kishimoto, T. (2005). Therapeutic efficacy of humanized recombinant anti–interleukin‐6 receptor antibody in children with systemic‐onset juvenile idiopathic arthritis. Arthritis & Rheumatism, 52(3), 818-825.
-
Zandi, K., Ramedani, E., Mohammadi, K., Tajbakhsh, S., Deilami, I., Rastian, Z., ... & Farshadpour, F. (2010). Evaluation of antiviral activities of curcumin derivatives against HSV-1 in Vero cell line. Natural product communications, 5(12), 1934578X1000501220.
-
Zar, A. R., Malik, A., Mahmood, A., Naseer, Q. A., & Yumei, L. (2019). Pathogenesis and the emerging Therapy of Vitiligo. Archives of Clinical and Biomedical Research, 3, 361-373.
-
Zhang, C., Wu, Z., Li, J. W., Zhao, H., & Wang, G. Q. (2020). The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. International Journal of Antimicrobial Agents, 105954.
-
Zhang, D. W., Fu, M., Gao, S. H., & Liu, J. L. (2013). Curcumin and diabetes: a systematic review. Evidence-Based Complementary and Alternative Medicine, 2013.
-
Zhang, J. S., Chen, J. T., Liu, Y. X., Zhang, Z. S., Gao, H., Liu, Y., ... & Xu, J. G. (2005). A serological survey on neutralizing antibody titer of SARS convalescent sera. Journal of medical virology, 77(2), 147-150.
-
Zhang, X., Song, K., Tong, F., Fei, M., Guo, H., Lu, Z., ... & Zheng, C. (2020). First case of COVID-19 in a patient with multiple myeloma successfully treated with tocilizumab. Blood advances, 4(7), 1307.
-
Zhao, Y., Tan, Y., Dai, J., Li, B., Guo, L., Cui, J., ... & Li, W. (2011). Exacerbation of diabetes-induced testicular apoptosis by zinc deficiency is most likely associated with oxidative stress, p38 MAPK activation, and p53 activation in mice. Toxicology letters, 200(1-2), 100-106.
-
Zhou, D., Dai, S. M., & Tong, Q. (2020). COVID-19: a recommendation to examine the effect of hydroxychloroquine in preventing infection and progression. Journal of Antimicrobial Chemotherapy.
-
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., ... & Guan, L. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet.
-
Zhou, J., Chan, L., & Zhou, S. (2012). Trigonelline: a plant alkaloid with therapeutic potential for diabetes and central nervous system disease. Current medicinal chemistry, 19(21), 3523-3531.
-
Zhou, N., Pan, T., Zhang, J., Li, Q., Zhang, X., Bai, C., ... & Tao, L. (2016). Glycopeptide antibiotics potently inhibit cathepsin L in the late endosome/lysosome and block the entry of Ebola virus, Middle East respiratory syndrome coronavirus (MERS-CoV), and severe acute respiratory syndrome coronavirus (SARS-CoV). Journal of Biological Chemistry, 291(17), 9218-9232.
-
Zhernov, Y. (2018). Natural humic substances interfere with multiple stages of the replication cycle of human immunodeficiency virus. Journal of Allergy and Clinical Immunology, 141(2), AB233.
-
Ziegler, C., Allon, S. J., Nyquist, S. K., Mbano, I., Miao, V. N., Cao, Y., ... & Muus, C. SARS-CoV-2 Receptor ACE2 is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Enriched in Specific Cell Subsets Across Tissues.
-
Zu, Z. Y., Jiang, M. D., Xu, P. P., Chen, W., Ni, Q. Q., Lu, G. M., & Zhang, L. J. (2020). Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology, 200490.
APPENDIX: SUPPLEMANTARY COVID-19 INFORMATION OUTSIDE THE PURVIEW OF THE PRESENT REVIEW
-
Appendix 1: Ozone, Air Pollution, and Viral Replication
Oxidants such as ozone may be used to kill SAR-CoV-2 that hangs in the air and, thereby limiting the role However, a number of findings point to the possible role of ozone oxidant exposure to viral replication in the human airway. Based on the findings that high levels of environmental pollution in Mexico City coincided with the outbreak of H1N1 influenza pandemic in 2009, Kesic et al., (2012) investigated whether ozone pollution contributed to an increase in Influenza A infection, with their findings showing that ozone may contribute to the cleavage, entry, and replication of influenza A through mechanisms such as disruption of protease/antiprotease balance within the airway liquid, and the potential role in altering the expression of human airway trypsin-like protease (HAT) and transmembrane protease, serine 2 (TMPRSS2). Therefore, exposure to ozone may also be playing a role in the spread and severity of COVID-19. A study conducted by Wu et al., (2020) revealed that exposure to air pollution in the form of fine particulate matter (PM2.5) may be playing a role in increased risk to COVID-19. The findings of the study showed that an increase in an increase of only 1 휇 g/m3 in PM2.5 is associated with an 8% increase in the COVID-19 death rate (95% confidence interval [CI]: 2%, 15%), which was however influenced by numerous confounding factors, such as age, population density, and population size (Wu et al.,2020). Therefore, while oxidants such as ozone might be help to control COVID-19 environmental contamination, reduction in exposure to oxidants such as ozone and environmental pollutants may decrease the risk of COVID-19 infection.
-
Appendix 2: Stress and COVID-19
Historically, psychological stress has been established to play a role in susceptibility and pathogenesis of infectious diseases. The importance of stress is underscored by its potential role in the impairment of the immune system. Early investigations carried out on the role of stress in viral infections conducted in both human and animal models have provided evidence to show that stress promotes such infections (Peterson et al., 1991). Findings from numerous studies have shown that a variety of psychological stressors, such as bereavement, academic pressure, and loss of self-esteem can result in laboratory evidence of immunologic impairment ((Peterson et al., 1991). Various stress-responsive neuropeptides and neurotransmitters interact with immune cells in vitro, leading to the suggestion of their possible role in immunosuppression (Black, 2002; Morera et al., 2019). Neuropeptides such as substance P (SP) have also been shown to mediate the inflammatory response by activating mast cells or other inflammatory cells, besides, central neuropeptides, mainly the corticosteroid releasing factor (CRF), and possibly SP, activate a systemic stress response through the activation of neuroendocrinological pathways such as the sympathetic nervous system, the renin angiotensin system, and the hypothalamic pituitary axis, which result into the release of stress hormones (catecholamines, corticosteroids, growth hormone, glucagons, and renin), contributing to the induction of the inflammatory response (Black, 2002). A study conducted by Freeman et al., (2007) showed that psychological stress compromises CD8+ T cell control of latent herpes simplex virus type 1 infections and, hence, underscoring the need to control physical stress to limit their role in immunosuppression. Vitamin C plays an essential role in stress response as it is an essential component of the production of cortisol and attenuation of blood pressure (Marik, 2020). The utilization of vitamin C in dietary response may impact on its availability for immune modulation and antioxidant injury (Marik, 2020). Based on the presented evidence, stress may compromise the control and management of COVID-19, which has led to increase in stressful situations, such as loss of jobs and change in lifestyles. Besides direct effects on the immune response, and particularly inflammatory cytokines, psychological stress may contribute to the depletion of vitamin C, which would compromise the immune response against COVID-19.
-
Appendix 3: Ultraviolet robots
A new medical technology that emits ultraviolet (UV) rays promises to improve the fight against respiratory infections, including viruses and bacteria, and most importantly SARS-CoV-2. The new technology emits UV light into the body could be used as a therapeutic to eradicate many viruses and bacteria, and works using the same principle employed by sunlight (Lai et al., 2018). Using the device, intermittent ultraviolet light can be administered into the trachea of a patient, and has a potential for positive outcomes in critically ill patients. The technology may play an important role in the prevention and treatment of COVID-19
Appendix 4: BCG Vaccination
Bacillus Calmette-Guerine (BCG) is a live attenuated strain derived from an isolate of Mycobacterium bovis that is used in many countries as a vaccine for Tuberculosis (TB). Across the world, countries such as Japan and China have a universal BCG vaccination policy in newborns; countries such as Spain, France, and Switzerland have discontinued universal BCG vaccination requirements due to comparatively low risk of developing M.bovis; while countries such as the United States, Netherlands, and Italy have not adopted vaccine policies due to similarly low risks M.bovis (Miller et al., 2020). Because the severity of COVID-19 takes a comparable pattern in countries with near-universal or mandatory vaccination policies, some studies have suggested the variation in morbidity and mortality outcomes in COVID-19 may be related to the BCG vaccination policy (Miller et al., 2020; Hegarty et al., 2020; Dayal & Gupta, 2020). The mechanism underlying the off-target effects of BCG vaccine is the induction of metabolic and epigenetic changes that enhance the innate immune response in subsequent infections, a process identified as trained immunity (Netea et al., 2020). A BCG-exposed immune system may therefore be more effective in the reduction of viremia following SARS-CoV- 2 exposure, consequently impacting on the severity and recovery time of COVID-19.
-
Appendix 5: Telemedicine
A key outcome of the COVID-19 pandemic has been limited movement of persons due to the need for “social distance” and “staying at home” so as to limit the chances of infection. The pandemic has also led to financial consequences that have negatively impacted on normal clinical services. As a result, there has been an increased use of technology-enabled remote patient care. In the United States, the relaxation of many requirements by the Centers for Medicare & Medicaid Services, and insurance companies, has necessitated the increased utilization of remote patient care services (Greiwe, 2020). Telemedicine is viewed as one of the approaches through which community transmission of COVID-19 can be prevented (Maras, 2020). Through the use of applications such as eConsults, patients are able to virtually meet their physicians and be provided with care for other ailments in a safe, cost-effective, and convenient manner (Greiwe, 2020). Besides the benefits achieved in preventing transmission of COVID-19, the utilization of telemedicine is a promising healthcare area that might facilitate improved efficiency, reduction in costs, and time saving in relation to health care.
-
Appendix 6: Hot Warm Saline Water Gargling
The rapid transmission of COVID-19 and the continued lack of an effective cure have led to the use of various techniques in a bid to prevent transmission or infection. Besides the consumption of vitamin C, other dietary supplements, and herbal remedies, boiled saline water gargling has been proposed as one of the ways through which the infection could be prevented or controlled (Khadka, Hashmi, & Usman, 2020). Warm saline water gargling or nasopharyngeal wash has been suggested as an effective method of preventing SARS-CoV-2 from inhabiting and replicating in the nasal and pharyngeal mucosa and, therefore, useful in controlling symptoms, viral shedding, and transmission (Singh et al., 2020). Though the effectiveness of nasopharyngeal wash has not been proved in COVID-19, its effectiveness in similar respiratory infections shows that it may work against COVID-19 (Singh et al., 2020; Khadka, Hashmi, & Usman, 2020).



