István Márton1*, Máté Kövér2, Péter Dudás1
1Department of North Pest Central Hospital - Military Hospital Emergency Care Center
2Department of North Pest Central Hospital Military Hospital Central Radiological Diagnostic Department
*Corresponding Author: István Márton, Department of North Pest Central Hospital - Military Hospital Emergency Care Center
Abstract
Introduction: The authors aim to present the diagnosis of a rare mediastinal cyst causing syncope, identified at the Emergency Department of the NorthPest Centre Hospital, Honvéd Hospital in Budapest. Data collection was performed retrospectively and through follow-up, with the patient's informed consent.
Objectives: The mediastinal widening observed on routine chest Xray, which had not been previously documented, highlights the importance of thorough investigation to determine the underlying cause of such findings. In cases of uncertain thoracic abnormalities, a CT scan is strongly recommended as it may significantly aid in reaching a diagnosis and in planning definitive therapy.
Methods: Data were collected retrospectively and via follow-up. Imaging studies, laboratory results, and surgical reports were retrieved from the hospital’s medical system (MedWoks).
Results: A patient examined due to blunt soft tissue injuries following syncope underwent chest X-ray, which revealed a widened mediastinum. To clarify the etiology, a chest CT angiography was performed, which confirmed the presence of a large anterior mediastinal cyst compressing the aorta, superior vena cava, trachea, and the left thyroid identified as the likely cause of the collapse. Due to elevated inflammatory markers, antibiotic therapy was initiated, followed by a thoracic surgical intervention using VATS technique. Intraoperatively, the suspected István Márton2thyroid involvement indicated by CT imaging could not be definitively confirmed.
Keywords: mediastinal cyst, collapse, syncope, thoracic surgery, emergency care
1. Introduction
This publication does not aim to provide a detailed overview of the various types of cysts that may occur in the mediastinum but merely lists them for reference.
We present the case of an elderly male patient who sustained a blunt head injury following a syncopal episode. In the course of the case presentation, we support our observations regarding mediastinal cysts with relevant references from international literature. Syncope is one of the most commonly encountered clinical conditions, with its initial evaluation typically performed in the emergency department. The primary priority is to rule out potentially lifethreatening causes, such as malignant arrhythmias (ventricular tachycardia, atrioventricular blocks, sinoatrial block, sick sinus syndrome), carotid sinus hypersensitivity, vasovagal reactions (e.g., triggered by stress or the sight of blood), pulmonary embolism, aortic aneurysm, aortic dissection, pericardial tamponade, tension pneumothorax, hemorrhage, acute neurological events, severe fluid and electrolyte imbalances (hyponatremia/hypernatremia, hypokalemia/ hyperkalemia), sepsis, and poisonings (alcohol intoxication, drug or chemical toxicity). During emergency assessment, these commonly occurring conditions are often absent or only partially evident. Occasionally, spaceoccupying lesions (such as tumors, abscesses, or cystic masses) that cause acute symptoms, and clinical manifestations are incidentally discovered. The present report describes one such case.
2. Case Presentation
On April 15, 2025, an 87-year-old male patient was brought to the Emergency Department of ÉPC HK by ambulance. He had not been seen by his family for three days and was found lying prone on the floor at home. He was admitted in a hemodynamically stable condition. The patient reported experiencing a dry cough over the previous few days but denied chest pain, dyspnea, or dizziness. His medical history included diabetes mellitus and hypertension; however, he had not taken his prescribed medications (metformin, glimepiride) due to forgetfulness. The patient denied smoking or alcohol use. On physical examination, hematomas were observed on the face, chest, and knees. Lungs were auscultated as clear bilaterally, without asymmetry. Vital signs were as follows: NIBP: 141/72 mmHg, HR: 100/min, SpO₂: 97%, T: 36.6 °C. The ECG showed mild ST-segment elevation in leads V1–V2.
Laboratory Findings:
1. Impaired renal function (eGFR: 45 ml/min/1.73 m²)
2. Markedly elevated C-reactive protein (287 mg/L; ref. 0–8 mg/L)
3. Leukocytosis (12.04 G/L; ref. 4.4–11.3 G/L)
4. Mild hyperglycemia (8.9 mmol/L)
5. Microscopic hematuria (++), ketonuria (++), and normal procalcitonin level
6. D-dimer testing was not performed due to the likelihood of false- positive results resulting from the fall and minor traumatic injuries. The carotid massage was negative, and the Schellong test could not be performed due to the patient's general weakness.
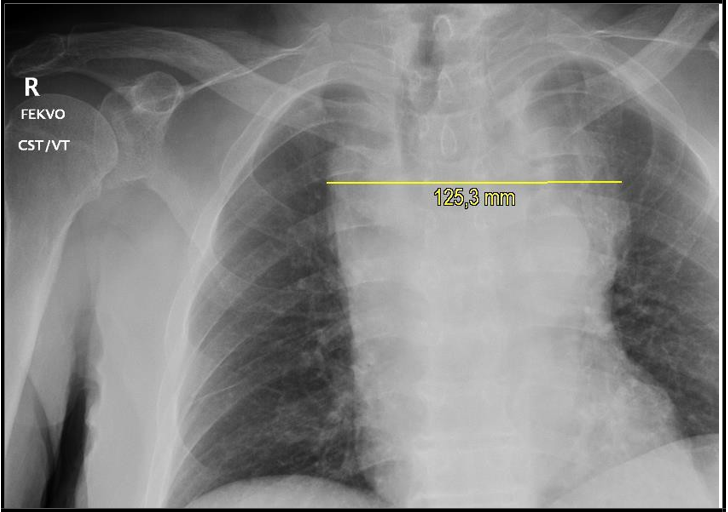
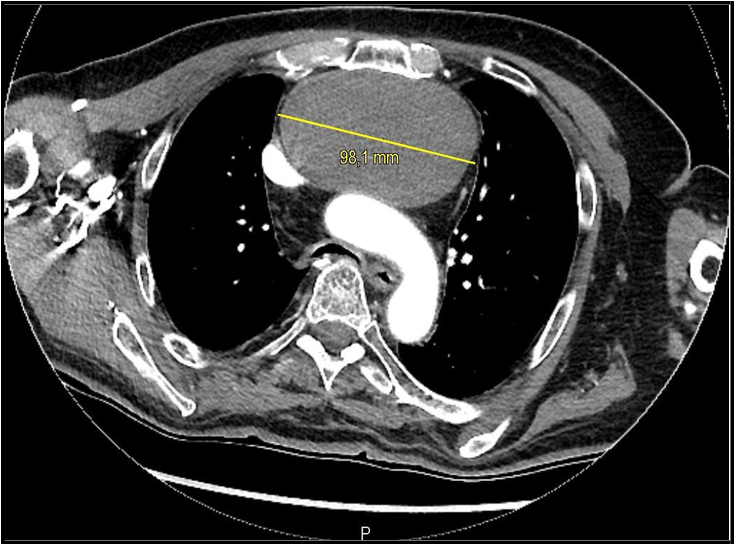
Imaging: Chest X-ray (Figure 1) revealed a markedly widened mediastinum, which appeared around 10 cm (laterolateral diameter). Behind this mass, the aortic notch is and the hilar vessels palely visible, which indicates anterior mediastinal mass. Based on this finding, a chest CT angiography confirmed a space-occupying unilocular cystic lesion in the anterior mediastinum, with a thin non- enhancing wall. CT scan revealed that the cystic lesion compressing the trachea and superior vena cava, displacing the aorta, and appearing in proximity to the left thyroid lobe, though distinctly separate from it (Figures 2–3). When measuring the density of this lesion it revealed low Hounsfield unit (~15-20 HU), without any enhancing part. In the differential of an anterior mediastinal mass, the lymphoid lesions and the thymoma are always on the board, but, this time, the purely cystic lesion brought us toward the mediastinal cyst in the report. 2. Figure. In the anterior mediastinum, an un ilocular cystic lesion was found without a thick enhancing wall with the size of 93 x 60 x 95 mm (LLxAPxCC) causing compression of the superior vena cava and displacing the aorta. Figure The anteroposterior chest X-ray showed extreme mediastinal widening, which indicated further examination.
Figure 1: The anteroposterior chest X-ray showing extreme mediastinal widening.
Figure 2: An approximately 10 cm anterior mediastinal cyst causing compression of the superior vena cava and the aorta.
Figure 3: An anterior mediastinal cyst originating near the location of the left thyroid lobe.
Consultations And Intervention: Due to suspected thyroid involvement, a head and neck surgery consultation were conducted, which excluded a thyroid origin. Cardiology evaluation (echocardiography) showed no signs of pericardial involvement. The patient was referred to thoracic surgery and four days later underwent video-assisted thoracoscopic surgery (VATS). Intraoperatively, ventilation was difficult, requiring intermittent ventilation of the operative lung. A tense, fluctuant lesion bulging into the pleura was identified in the anterior mediastinum. Upon opening the connective tissue layer, a dorsally located vein was injured, managed with tamponade and Prolene sutures. The cyst yielded thick, particulate, gruel-like yellow-green contents, which were aspirated, and the cavity was irrigated. The cyst wall only partially collapsed. Drains were placed in the cyst cavity and posterior thoracic cavity near the hilum. The exact origin of the cyst could not be clearly identified intraoperatively. Post-procedure, the lung expanded well without air leak or secondary bleeding, and surgical closure was completed.
Postoperative Course And Follow-Up: Following VATS surgery and antibiotic therapy, laboratory parameters showed significant improvement: eGFR 71 ml/min/1.73 m², CRP 45 mg/L, leukocyte count 6.9 G/L. The patient was transferred to the pulmonology ward for continued monitoring and treatment.
3. Literature Review
Amar et al. [1] in their 2023 study compared various imaging modalities (contrast-enhanced CT, MRI, F-18 FDG PET-CT) and discussed the advantages and limitations of each technique. They concluded that the imaging diagnosis of cystic mediastinal lesions remains a diagnostic challenge. The location and imaging characteristics of these lesions are often sufficient to establish a diagnosis even without histological confirmation. CT, MRI, and ultrasound each offer specific benefits and limitations. CT is typically the first-choice modality for identifying and characterizing such lesions. MRI (including native and contrast-enhanced T1-weighted, T2-weighted, and diffusion-weighted sequences) is a key problem- solving tool. Ultrasound is useful for real-time characterization and for guiding interventional procedures.
Barrios et al. [2] conducted a retrospective analysis of cases between 1977 and 2022, detailing the different types of cysts and specifying which cases require surgical intervention and which may be adequately managed with radiological follow-up.
Benjamin et al. [3] published findings from a nine-year study conducted in the U.S., analyzing data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) between 1992 and 2000. They used representative weighted estimates to determine the incidence and hospital admission rates for patients presenting to emergency departments, stratified by demographic characteristics. Cardiovascular diagnoses at ED discharge (based on ICD-9 codes) were recorded. Of the 865 million ED visits during the nine-year period, 6.7 million (0.77%; 95% CI: 0.69–0.85%) were attributed to syncope.
Diana et al. [4] described cysts located in the anterior, middle, and posterior mediastinum. Their review included additional case reports comparing surgical techniques such as VATS, robot-assisted thoracoscopy (RATS), and thoracotomy. Minimally invasive approaches (VATS and RATS) have gained prominence due to improved patient outcomes, particularly in terms of reduced hospital stays and chest drain duration.
Frances et al. [5] found that out of 18,898 patients, syncope was diagnosed in 214 cases. Syncope accounted for 1–3% of all ED visits. Their aim was to evaluate the impact of implementing an Integrated Care Plan (ICP) based on the European Society of Cardiology (ESC) guidelines on hospital admission rates and outpatient referrals to the Syncope Management Unit (SMU). They assessed the appropriateness of admissions and referrals, and final diagnoses. Their hypothesis was that introducing the ICP would increase outpatient referrals while ensuring urgent cardiac syncope cases were appropriately admitted.
Fuliang et al. [6] highlighted the advantages of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA). According to their study, EUS-FNA offers higher diagnostic accuracy for mediastinal cysts than CT and is safe when combined with prophylactic antibiotics. A single puncture with a 19G needle was sufficient for diagnosis and complete cyst drainage, particularly in cases with thin fluid content. Their key findings included:
1. No infectious complications occurred with prophylactic antibiotic use.
2. EUS-FNA may serve as a palliative option for non-surgical candidates.
3. CT often misinterprets cysts as solid lesions.
4. Surgical excision is often warranted even in asymptomatic cases to prevent complications. In summary, EUS-FNA is a safe and accurate method for diagnosing mediastinal cysts, especially with appropriate antibiotic coverage.
Sathyaprasad et al. [7] reported two male patients (ages 54 and 74) who underwent mediastinoscopic cyst removal. Mediastinoscopy is a minimally invasive procedure with a very low morbidity and mortality rate (<0.5% in large series). Standard cervical mediastinoscopy (SCM), as applied by the authors, allows access to both right and left paratracheal areas, the hila, and the carina — common sites for mediastinal cysts. The authors also described various endoscopic and surgical techniques, including extended cervical mediastinoscopy (ECM), SCM, Chamberlain's anterior mediastinotomy for aorto-pulmonary window lesions, and VATS. Wackerman et al. [8] provided an overview of widened mediastinum as a radiographic sign frequently seen on plain chest X-rays. The mediastinum is considered widened when it exceeds 6–8 cm in width, depending on the reference source. Possible causes include:
1. Ascending and proximal descending aortic aneurysm
2. Aortic dissection (ascending and descending)
3. Aortic unfolding
4. Traumatic aortic rupture
5. Hilar lymphadenopathy (infectious or malignant)
6. Mediastinal tumors (e.g., lymphoma, seminoma, thymoma)
7. Mediastinitis
8. Cardiac tamponade
9. Rib or thoracic vertebral fractures
Major syncope studies [3, 5] did not mention mediastinal cysts as a cause, underscoring the rarity of this condition.
According to the publication by Hayder et al. [9] in the Chest Journal, thymic lesions are commonly found in the anterior mediastinum, accounting for approximately 13% of all mediastinal masses. Thymic cysts represent 5% of mediastinal cysts and 1% of all mediastinal lesions. They presented the case of a 64-year-old woman with a history of asthma who was admitted to the hospital following a syncopal episode. Physical examination, neurological assessment, and initial laboratory and imaging studies revealed no abnormalities. A contrast-enhanced chest CT confirmed the presence of a cyst, after which a right-sided video-assisted thoracoscopic surgery (VATS) was performed. During the procedure, the cystic fluid was aspirated, and the cyst wall was deroofed. The authors hypothesized that, during intrauterine development, aberrant migration of accessory thymic lobes may result in thymic tissue being located in ectopic sites.
Vidushi et al. [10] described the case of a 34-year-old female patient in the Chest Journal in 2012. The patient underwent an evaluation for a two-year history of palpitations, dizziness, and a single syncopal episode. Non-sustained ventricular tachycardia was identified. Pacemaker implantation was initially considered. As part of a second opinion, cardiac magnetic resonance imaging (MRI) was performed to rule out arrhythmogenic right ventricular dysplasia. The MRI revealed a small circumferential pericardial effusion and an anterior mediastinal mass compressing the right ventricular outflow tract. A CT-guided biopsy confirmed a type A thymoma. Surgical resection via median sternotomy was performed, during which an 8–9 cm × 4– 5 cm thymoma infiltrating the pericardium was successfully removed. The postoperative course was uneventful, and the patient was discharged home.
4. Conclusions
Mediastinal cysts are rare but clinically significant findings, especially when syncope is the presenting symptom. In cases where mediastinal widening is detected in the emergency department, rapid and accurate diagnosis can be life-saving, as several life-threatening conditions—such as aortic dissection, aneurysm, or abscess—may present with similar radiological features. The observation presented in this report highlights the crucial role of imaging and multidisciplinary collaboration in the identification and differential diagnosis of mediastinal cysts.
5. Summary
The case presented in this report highlights that, in rare instances, syncope may be caused by uncommon yet readily identifiable conditions. Beyond the standard diagnostic protocols, it is essential for clinicians to consider the possibility of atypical and rare etiologies. Fundamental diagnostic tools—such as abdominal and cardiac ultrasound, as well as chest X-ray—play a guiding role in the diagnostic algorithm and may support the indication for further targeted imaging studies (e.g., CT or MRI). These decisions should always be made in conjunction with a comprehensive assessment of the patient’s current vital signs and laboratory findings.
6. Research Location, Brief Hospital Overview
The North Pest Centrum Hospital is a highly progressive (Level III progressivity), multidisciplinary, world-class, and exceptionally well- equipped medical institution. It encompasses all major medical specialties and offers a wide range of advanced imaging diagnostic modalities, including X-ray, ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography–computed tomography (PET-CT). Both outpatient and inpatient care services are available within the hospital.
Key departments include the emergency department, internal medicine, cardiology, general surgery, thoracic surgery, cardiac surgery, vascular surgery, neurosurgery, gynecology, ophthalmology, otorhinolaryngology and head and neck surgery, urology, diabetology, hematology, angiology, neurology, nephrology, and psychiatry. Additionally, the hospital features a state-of-the-art central laboratory department, where all essential laboratory tests are performed.
7. Acknowledgments
I would like to express my sincere gratitude to my co-authors for their dedicated contributions. Two of my colleagues provided invaluable assistance in preparing this case report: Dr. Máté Kövér, radiology specialist, and medical student Péter Dudás. Dr. Kövér supported the interpretation of radiological findings and the description of anatomical structures, while Péter Dudás contributed significantly to the collection of relevant literature, which greatly facilitated the writing of this article.
References
- Shah A, Rojas CA (2022) Imaging modalities (MRI, CT, PET/CT), indications, differential diagnosis and imaging characteristics of cystic medias masses: a review. Mediastinum. 7: 3.
- Barrios P, Avella Patino D (2022) Surgical indications for mediastinal cysts—a narrative review. Mediastinum. 6: 31.
- Sun BC, Emond JA, Camargo CA Jr (2004) Characteristics and admission patterns of patients presenting with syncope to U.S. emergency departments, 1992-2000. Acad Emerg Med. 11(10): 1029-34.
- Hsu DS, Banks KC, Velotta JB (2022) Surgical approaches to mediastinal cysts: clinical practice review. Mediastinum. 6: 32.
- McCarthy F, McMahon CG, Geary U, Plunkett PK, Kenny RA, et al. (2008) Management of syncope in the Emergency Department: a single hospital observational case series based on the application of European Society of Cardiology Guidelines. Europace. 11(2): 216–224.
- Cao F, Zhang S, Dai Z, Fu Q, Guo F, et al. (2022) Diagnosis of mediastinal cysts: the role and safety of EUS–FNA with 19-gauge needle: a retrospective cohort study. J Thorac Dis. 14(9): 3544- 3551.
- Burjonrappa SC, Taddeucci R, Arcidi J (2005) Mediastinoscopy in the Treatment of Mediastinal Cysts. J The Society of Laparoscopic & Robotic Surgeons. 9(2): 142–148.
- Wackerman L, Gnugnoli DM (2023) National Library of Medicine. StatPearls.
- Hashim H, Al-Khalili R, Maher J (2012) Posterior Mediastinal Thymic Cyst: A Case of a 64-Year-Old Woman With Syncope. Chest Journal. 142(4): 1020A.
- Sharma V, Rohr C, Sallach S, Paidipaty BB, Haupt M (2012) Anterior Mediastinal Thymoma Compressing the Right Ventricular Outflow Tract (RVOT) Causing Syncope. Chest Journal. 142(4): 580A.