Ahmed Sami-Al-Hasan1, Kazi Rakibul Islam2*, Tamanna Mahfuza Tarin3, Nasrin Akter2, Sujana Haque Chowdhury2, Ulfat Ara2, Mohammad Quamruzzaman4, Sarder Mahmud Hossain2, Bilkis Banu2
1National Institute of Cancer Research Hospital, Dhaka, Bangladesh.
2Department of Public Health, Northern University Bangladesh, Dhaka, Bangladesh.
3Directorate General of Health Services, Mohakhali, Dhaka.
4Bangladesh Medical College Hospital, Dhaka, Bangladesh.
*Corresponding Author: Kazi Rakibul Islam, 2Department of Public Health, Northern University Bangladesh, Dhaka, Bangladesh.
Abstract
Bangladesh has been combating COVID-19 successfully since March 2020. Here and now, COVID-19 will persist as a part of our daily life. The epidemiological circumstances of discharge and dead COVID-19 patients will add a new era to building a robust healthcare system in Bangladesh. It was a quantitative type of cross-sectional survey with a retrospective approach. Data were collected from 400 patients (200 discharged and 200 dead cases) case history files from a well-known hospital in Dhaka, Bangladesh. A correlation between the variables was observed through multivariate analysis (Chi-Square test), and to predict the insights of different characteristics of COVID-19 discharged and dead cases, 95 % confidence intervals were considered. Ethical issues were maintained according to the guidance of the Declaration of Helsinki. Here, the majority (64.5 %) of dead patients were from the senior adult group (aged > 60 years) who had more than one co-morbidity. The study revealed that death occurrences among cases were significantly (p <0.01) more observed among patients with comorbid diseases and, before hospitalization, stayed at home for more than 10 days. In addition, it was also observed that malnourished cases were significantly (p < 0.01) found to be the vulnerable group in both discharged (50.5 %) and dead (46.5 %) cases. Elderly malnourished patients who had co-morbidity more than one, especially those who delayed their hospitalization and stayed at home for an extended period significantly reported as death cases. Delayed treatment initiation and hospitalization, nutritional deficiency, and co-morbidity were found to be intensifying factors among the deaths compared to discharge cases.
Keywords: Demographic features, Clinical features, COVID-19, Discharged, Death.
Introduction
COVID-19 pneumonia is a public health emergency of international concern. It causes millions of deaths both in developed and underdeveloped countries. Thousands of researches are going on to assess the risk factors for mortality. In Bangladesh, thousands of people already died due to COVID-19 infection. COVID-19 pneumonia is now a major burning issue and a top priority in public health worldwide due to its devastating impact on human life and the economy. An outbreak of viral pneumonia with an unidentified etiology was announced in Wuhan, China, on December 12, 2019. [1,2] Further research indicated the presence of a novel coronavirus which had been quickly isolated and its genome had been sequenced.[3] The World Health Organization (WHO) named this virus the 2019 novel coronavirus (2019-nCoV) [4] and, subsequently, it was named Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) by the Coronaviridae Study Group (CSG) of the International Committee on Taxonomy of Viruses. [5] Officially, COVID-19 became the name of the disease caused by the virus5 above. SARS-CoV-2 started from a local seafood market in Wuhan of a probable bat origin since it is 96 % gnomically similar to a bat coronavirus (Bat CoV RaTG13), and the infection became hard to control or prevent ever since Chinese health authorities declared a possibility of person to person transmission even if subjects were asymptomatic.[6] On March 11, 2020, WHO announced COVID-19, a global pandemic that appears to be disseminated at an extreme rate; as of April 21, 2020, at least 23,14,621 cases were confirmed and 1,57,847 cases of death. COVID-19 symptoms differ among patients and may include fever, cough, breathing difficulties, and organ failures, and in its severe levels, COVID-19 may lead to death and thus threaten the whole society.[7] Older age, increased D-Dimer, and higher Sequential Organ Failure Assessment score were identified as the risk factors for mortality of COVID-19 in one investigation in China.2 Bangladesh is South Asia's second most affected country, after India. 378,266 cases were detected till October 11, 2020, with 5,524 deaths. Almost 2.2% of the world's population lives in Bangladesh7. COVID-19 is a highly contagious disease transmitted by respiratory droplets. Disease severity and death (1.41 %) due to COVID-19 seem to be lower in a densely populated country like Bangladesh.[8]
This study proposed to show the demographic and clinical features of discharged versus dead patients with COVID-19 and to find any significant association of different predictors with the comorbid disease conditions among the deceased and discharged patients of Covid-19 pneumonia. As the comorbid conditions are established risk factors for case fatality and mortality in Covid-19, their association with other predictors may give us a clue about the other risk factors enhancing the mortality and morbidity rate in Covid-19 pneumonia.
Methods
Study design
This was a descriptive type of cross-sectional study. Structured data were collected retrospectively in this study from September to December 2021. Socio-demographic, lifestyle, and clinical information were extracted from the discharged and dead cases of COVID-19 in Bangladesh.
Study participants, sample size, and sampling
This study included 400 patients with COVID-19 admitted to the Kurmitola General Hospital (KGH) in Dhaka city of Bangladesh. Retrospective information was collected from 200 discharged patients admitted to the KGH due to COVID-19 pneumonia and 200 patients who died from COVID-19 in the same hospital.
The total sample was calculated using the formula "n= 'Z2pq/d2," where p (average infection rate of COVID-19) [9] was considered 0.15, and d was considered 0.05. The calculated sample size was 200. So, 200 respondents were recruited in the study as discharged cases after having COVID-19 infection, and similarly, 200 death cases due to COVID-19 were enrolled in the study. Finally, 400 samples were considered in this study.
A systematic random sampling technique was used for this study. Considering the diversified patients of Dhaka city, the study was conducted in the largest COVID-19 dedicated hospital, i.e., KGH of Dhaka district, under the Dhaka division. 400 samples were selected from the list provided by the hospital authority. Finally, 200 discharged and 200 death cases were selected from the list by systematic random sampling following inclusion criteria. Patients with tested positive for COVID-19 pneumonia by RT-PCR (Reverse transcription polymerase chain reaction) method were included in this study. Moreover, patients who died after admission at KGH were considered death cases, but data were included only from the cases whose legal guardians consented.
Data collection
A structured questionnaire was used to gather data in this study. The objective and nature of the study were explained, and the discharged cases and the legal guardian of deceased subjects carried out written or verbal consent. Data on discharged and dead cases were collected from the patient case history file of KGH using the hospital register book. All authors had access to the collection and preserving participants' information during or after data collection. The study was conducted with the utmost support of the hospital authority.
Ethical considerations
This study was approved by the Ethical Review Committee of the Department of Public Health of Northern University Bangladesh (NUB/DPH/EC/2021/10-b) and conformed to the Declaration of Helsinki. Participation of the respondents was anonymous and voluntary. Informed consent was sought from the respondents at the beginning of the survey, and participants could withdraw from the study at any time.
Questionnaire design
The structured questionnaire was pre-validated by two independent reviewers. The questionnaire comprised several segments:
1. Socio-demographic information of the discharged and dead patients: age, gender, habitat
2. Lifestyle-related information: smoking habit, weight, height, nutritional status
3. Clinical information: duration of home stay after COVID-19 diagnosis, comorbid diseases, previous treatment history, additional treatment
Data analysis
Collected data was checked and analyzed employing the Statistical Package for the Social Sciences (SPSS) software. Study characteristics were subjected to descriptive statistics (frequency and proportions) to summarize the obtained data. A multivariate analysis (Chi-Square test) was performed to observe the correlation between the variables. 95 % confidence intervals were used to visualize the insights of different characteristics of COVID-19 discharge and death cases.
Results
|
Table 1: Characteristics of the discharged and dead COVID-19 cases (n=400) |
||||
|
Characteristics |
Discharged cases (200) |
Dead cases (200) |
||
|
Number of participants, (n) |
Percent of participants, (%) |
Number of participants, (n) |
Percent of participants, (%) |
|
|
Age (in years) |
|
|
|
|
|
Up to 60 |
60 |
30.0 |
69 |
34.5 |
|
140 |
70.0 |
131 |
64.5 |
|
Gender |
|
|
|
|
|
Male |
144 |
72.0 |
144 |
72.0 |
|
Female |
56 |
28.0 |
56 |
28.0 |
|
Habitat |
|
|
|
|
|
Urban |
155 |
77.5 |
144 |
72 |
|
Rural |
45 |
22.5 |
56 |
28 |
|
Nutritional Status |
|
|
|
|
|
Malnourished |
135 |
67.0 |
132 |
66.0 |
|
Healthy |
65 |
33.0 |
68 |
34.0 |
|
Smoking Habit |
|
|
|
|
|
Smoker |
99 |
49.5 |
99 |
49.5 |
|
Non-smoker |
101 |
50.5 |
101 |
50.5 |
|
Duration of Home stay |
|
|
|
|
|
Up to 10 days |
27 |
13.5 |
27 |
13.5 |
|
> 10 days |
173 |
86.5 |
173 |
86.5 |
|
Previous Treatment History |
|
|
|
|
|
Yes |
60 |
30 |
71 |
35.50 |
|
No |
140 |
70 |
129 |
64.50 |
|
Additional treatment |
|
|
||
|
Yes |
25 |
12.5 |
49 |
24.50 |
|
No |
175 |
87.5 |
151 |
75.50 |
|
Data are presented as frequency (n), percentage (%); |
||||
This study included a total of 400 patients with COVID-19. Retrospectively information was collected from 200 discharged patients admitted to the hospital due to COVID-19 pneumonia and from 200 patients who died from COVID-19 in the same hospital. Among the discharged cases, the majority (70 %) of the respondents were above 60 years, whereas only (30 %) were up to 60 years. In the case of death cases, 64.5 % of respondents were above 60 years, whereas 34.5 % were up to 60 years. Most of the respondents in both death & discharged subjects were male (70 %, n=144/200), and the rest (28 %, n=56/200) were female. Many of the respondents stayed home (86.5 %, n=173/200) for more than 10 days in both death & discharged cases, whereas a significantly fewer number of the respondents were home (13.5 %, n=27/200) for up to 10 days & then went for the hospital. It reflects the respondent's negligence & lack of confidence in the country's health system, even in a capital city. Looking at the additional treatment, it was revealed that 87.5 % of the respondents didn't take any other treatment like dialysis, cardiac stenting, chemotherapy, etc. Among the discharged cases & only 12.5 % of the respondents went for that. In the case of death cases, 75.50 % of the respondents did not take additional treatment, whereas 24.50 % received that.
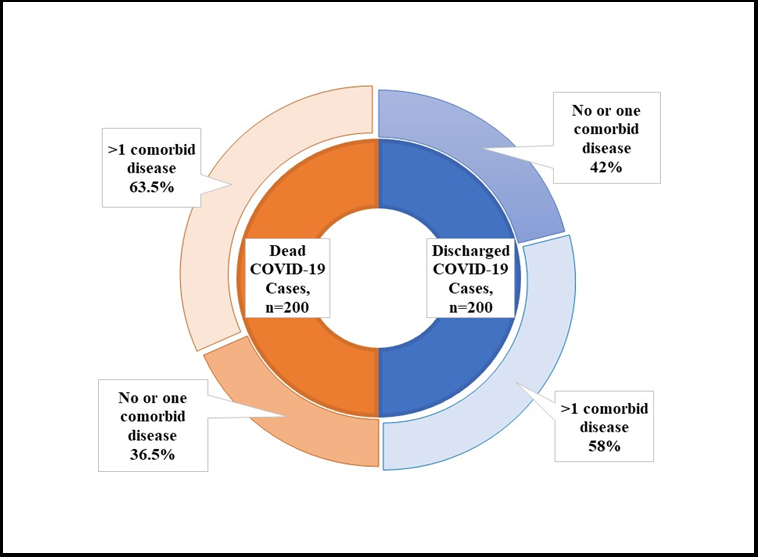
Figure 1: Status of co-morbid diseases among the COVID-19 discharged and dead cases (n=400)
Regarding co-morbid diseases, our study revealed that among the dead cases, 63.5 % suffered from more than one disease, whereas 36.5 % of the respondents had no or only one condition. However, among the discharged instances, 58 % suffered from more than one co-morbid disease, and there was no or one co-morbid disease among 42 % of the respondents.
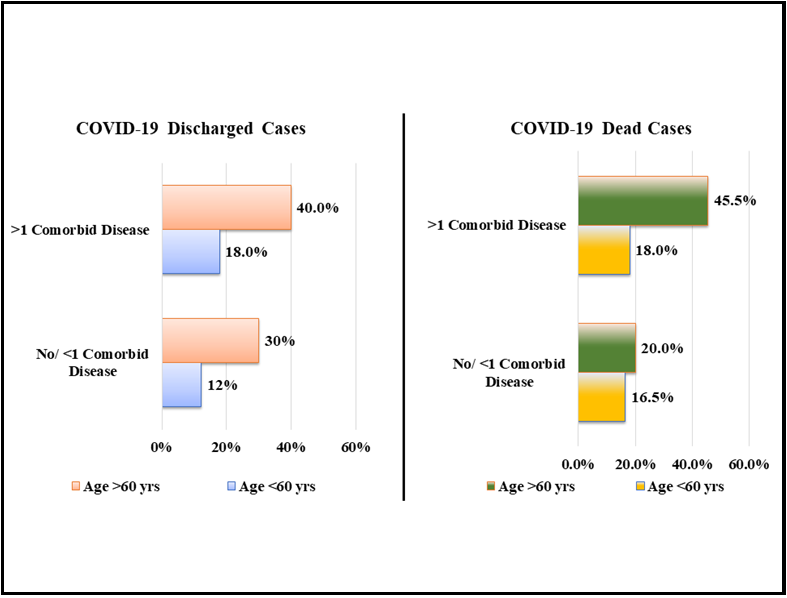
Figure 2: Correlation between age and co-morbidity status among the respective study subjects (n=400)
Highlighting the correlation between age and comorbidity status among both discharged and dead cases, the study found that there is a significant association of age range among COVID-19 patients with co-morbid conditions in both discharged (p=0.03) & dead (p=0.01) cases. Out of 200 terminated points, respondents had more than one co-morbid disease condition (40 %, n=80/200), and belonged to the > 60-year age group, whereas no or one co-morbid need (30 %, n=60/200) was found among the same age group. In the case of death cases, it was significantly found that respondents from the > 60-year age group had more than one co-morbid disease condition (45.5 %, n=91/200) in the highest manner compared to the counters.
Figure 3: Correlation between home stay before hospital admission and co-morbidity status among the respective study subjects (n=400)
The study revealed that the duration of homestays of COVID-19 patients was significantly associated with their co-morbid conditions, both in discharged (p = 0.012) and dead (p = 0.01) cases. COVID-19 discharged cases were staying at home for more than ten days (56 %) with the co-morbid disease more than one, whereas fewer co-morbid groups (3.50 %) found to spend less time (< 10 days) at home compared to those subjects who had more than 1 co-morbid diseases (2.0 %). Among the dead cases, both groups with comorbidity status (No/ <1 co-morbid disease: 34.5%; > 1 co-morbid disease: 52 %) were found to have stayed at home more than 10 days before hospital admission. Moreover, patients with more co-morbid diseases were found higher to stay at home rather than take early hospital treatment. Our study discovered that COVID-19 patients had better outcomes with fewer homestays overall.
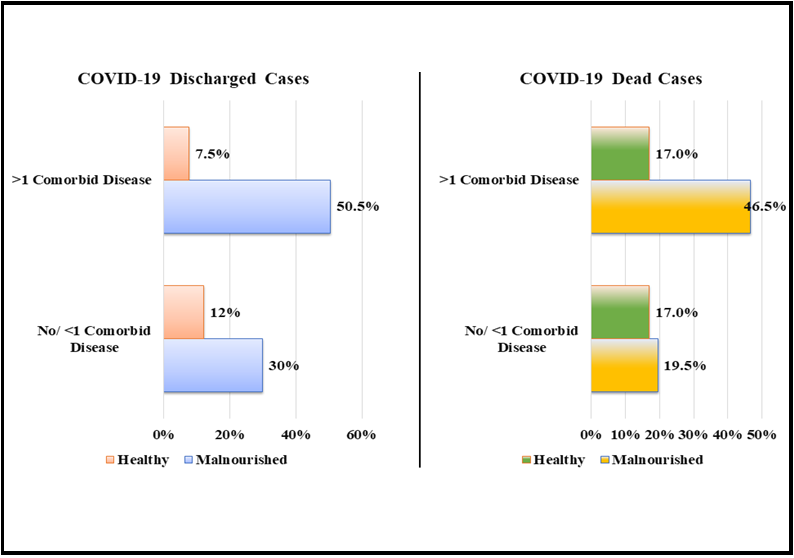
Figure 4: Correlation between nutritional status and co-morbidity status among the respective study subjects (n=400)
Our study analysis also observed a significant association between the nutritional status of COVID-19 patients and their co-morbid conditions in both discharged (p=0.001) and death (p=0.004) cases. To explore the discharged patients, significant respondents 50.5 % found malnourished among the cases with more than one co-morbid disease, whereas among the dead issues, this figure was 46.5 % as underweight. On the other hand, among the discharged instances, 30 % were found malnourished with no or one co-morbid disease, whereas 19.5 % of the respondents were underweight with no co-morbid illness. Illustrating the outcome, we can conclude that skinny people were the most vulnerable group in both discharged and dead cases of COVID-19.
Discussion
There are variations in the demographic profiles and clinical features among the deceased and discharged patients of COVID-19. These profiles and clinical characteristics can identify multiple risk factors associated with mortality and fatality of COVID-19 pneumonia. Among the risk factors, co-morbid conditions like HTN, diabetes mellitus, ischemic heart disease, chronic kidney disease, and chronic respiratory disease play a pivotal role in mortality and morbidity incidence in COVID-19 patients. In this study, we try to find a demographic profile with clinical features and the association of other risk factors with the co-morbid disease condition among COVID-19 dead and discharged patients.
The study was done at a COVID-dedicated tertiary hospital – Kurmitola General Hospital. It was a retrospective observational study. It included a total of 400 patients with COVID-19. Retrospectively information was collected from 200 discharged patients admitted to the hospital due to COVID-19 and from 200 patients who died from COVID-19 in the same hospital. Among the discharged cases, the majority (70 %) of the respondents were above 60 years, whereas only (30 %) were up to 60 years. In the case of death cases, 64.5 % of respondents were above 60 years, whereas 34.5 % were up to 60 years. In several previous studies, older age was found as a potential risk factor for death among COVID-19 patients. [10,11] Majority of the respondents in both ends and discharged cases were male (70 %, n=144/200), rest of the respondents (28 %, n=56/200) were female in both cases. Other studies also show that male patients with COVID-19 were more likely to die compared to female patients.12 Majority of the respondents stayed home (86.5 %, n=173/200) for more than 10 days in both death & discharged cases, whereas significantly fewer number of the respondents were home (13.5 %, n=27/200) up to 10 days and then went to the hospital. It reflects the respondent's negligence and lack of confidence in the country's health system, even in a capital city. Looking at the additional treatments, the study revealed that 87.5 % of the respondents didn't take any other medicines like dialysis, cardiac stenting, chemotherapy, etc. Among the discharged cases & only 12.5 % of the respondents went for that. In the case of death cases, 75.50 % of the respondents did not take additional treatment, whereas 24.50 % received that.
Regarding co-morbid diseases, the study revealed that among the dead cases, 63.5 % suffered from more than one disease, whereas 36.5 % of the respondents had no or only one condition. However, among the discharged instances, 58 % suffered from more than one co-morbid disease, and there was no or one co-morbid disease among 42% of the respondents. Several independent studies also found an association between mortality among COVID-19 patients and increased chronic diseases such as (cardiac, renal, liver, kidney, and lung). [13,14]
The study found a significant association of age range among COVID-19 patients with co-morbid conditions in both the discharged (p=0.03) and dead (p=0.01) cases. Out of 200 terminated points, respondents had more than one co-morbid disease condition (40 %, n=80/200) and belonged to the > 60-year age group. In the case of death cases, it was significantly found that respondents from the > 60-year age group had more than one co-morbid disease condition (45.5 %, n=91/200) in the highest manner compared to the counters.
The study revealed that the duration of homestays of COVID-19 patients was significantly associated with their co-morbid conditions, both in discharged (p = 0.012) and dead (p = 0.01) cases. COVID-19 discharged cases were staying at home for more than ten days (56 %) with the co-morbid disease more than one, whereas fewer co-morbid groups (3.50 %) found to spend less time (< 10 days) at home compared to those subjects who had more than 1 co-morbid diseases (2.0 %). Among the dead cases, both groups with co-morbidity status (No/ < 1 co-morbid disease: 34.5 %; > 1 co-morbid disease: 52 %) were found to have stayed at home more than 10 days before hospital admission. Moreover, patients with more co-morbid diseases were found to remain at home rather than take early hospital treatment. Our study discovered that COVID-19 patients had better outcomes with fewer homestays overall. Delayed admission to the hospital is a risk factor for COVID-19 mortality shown in other studies.[15]
Our study analysis also observed a significant association between the nutritional status of COVID-19 patients and their co-morbid conditions in both discharged (p=0.001) and death (p=0.004) cases. To explore the discharged patients, significant respondents, 50.5 % were found malnourished with more than one co-morbid disease, whereas, among the dead cases, 46.5 % were underweight. On the other hand, among the discharged instances, 30 % were found malnourished with no or one co-morbid disease, whereas 19.5 % of the respondents were underweight with no co-morbid illness. Illustrating the outcome, we can conclude that skinny people were the most vulnerable group in both discharged and dead cases of COVID-19. It was found that obese patients with COVID-19 had a higher risk of dying compared to nonobese patients. Consistent results were found in several studies. [15,16]
Conclusion
The study aimed to understand the epidemiological situations of discharged and dead COVID-19 patients, essential for policy making and strengthening the healthcare system. There are distinctions in demographic profiles and clinical features between diseased and discharged patients of Covid -19 were found. The study revealed that the senior adult group, malnourished people, and who had more than one co-morbidity were more vulnerable and sufferers. Moreover, COVID-19 patients with more than one co-morbidities and delayed hospitalization exaggerated the disease's severity, and more deaths occurred among them. So, we concluded from our study results that aged malnourished patients with co-morbidities, who stayed at home for long periods before hospitalization, and obese patients were notably reported as death cases. The outcomes of this study suggest that aged, malnourished COVID-19 patients with co-morbidities should be handled carefully in home and hospital settings with needed facilities. Awareness should be built among people using mass media. Furthermore, health professionals can conduct training highlighting the proper handling of those patients.
Acknowledgment: We firmly acknowledge the study participants and the authority of the study place.
Source of funding: There was no funding for this study.
Conflict of interest statement: The authors declared no conflict of interest.
References
- Ji W, Wang W, Zhao X, Zai J, Li X (2020) Cross‐species transmission of the newly identified coronavirus 2019‐nCoV. J Med Virol. 92(4): 433-440.
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID19 in Wuhan, China: a retrospective cohort study. Lancet. 395(10229): 1054-1062.
- Chan JF, Yuan S, Kok KH, To KK, Chu H, et al. (2020) A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. The lancet. 395(10223): 514-523.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 382(18): 1708-1720.
- Mesev EV, LeDesma RA, Ploss A (2019) Decoding type I and III interferon signalling during viral infection. Nat Microbiol. 4(6): 914-924.
- Fang Y, Nie Y, Penny M (2020) Transmission dynamics of the COVID‐19 outbreak and effectiveness of government interventions: A data‐driven analysis. J Med Virol. 92(6): 645- 659.
- McNicoll G. United nations department of economic and social affairs, population division: Population, resources, environment and development database, version 4.0. Popul Dev Rev. 2006 Dec 1; 32(4):790-1.
- DGHS (2020) Bangladesh Corona virus: Covid-19 infection, death rate increase in Bangladesh. The Business Standard.
- Islam MT, Talukder AK, Siddiqui MN, Islam T (2020) Tackling the COVID-19 pandemic: The Bangladesh perspective. J Public Health Res. 9(4): 1794.
- Imam Z, Odish F, Gill I, O'Connor D, Armstrong J, et al. (2020) Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID‐19 patients in Michigan, United States. J Intern Med. 288(4): 469-476.
- Covino M, De Matteis G, Santoro M, Sabia L, Simeoni B, et al. (2020) Clinical characteristics and prognostic factors in COVID‐ 19 patients aged≥ 80 years. Geriatr Gerontol Int. 20(7): 704-708.
- Chen F, Sun W, Sun S, Li Z, Wang Z, et al. (2020) Clinical characteristics and risk factors for mortality among inpatients with COVID‐19 in Wuhan, China. Clin Transl Med. 10(2): e4.
- Yao Q, Wang P, Wang X, Qie G, Meng M, et al. (2020) Retrospective study of risk factors for severe SARS-Cov-2 infections in hospitalized adult patients. Pol Arch Intern Med. 130(5): 390-399.
- Chen L, Yu J, He W, Chen L, Yuan G, et al. (2020) Risk factors for death in 1859 subjects with COVID-19. Leukemia. 34(8): 2173-2183.
- Laguna-Goya R, Utrero-Rico A, Talayero P, Lasa-Lazaro M, Ramirez-Fernandez A, et al. (2020) Interleukin-6-based mortality risk model for hospitalised COVID-19 patients. J Allergy Clin Immunol. 146(4): 799-807.
- Calvet G, Aguiar RS, Melo ASO, Sampaio SA, de Filippis I, et al. (2016) Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect Dis. 16(6): 653-660.