Paulina Cyngot1*, Monika Kompa1, Anna Stadnik1, Edyta Maj1, Joanna Furmanek2, Aleksandra Golenia2
12nd Department of Clinical Radiology, University Clinical Centre of Medical University of Warsaw, Poland.
2Department of Neurology, Medical University of Warsaw, Poland.
*Corresponding Author: Paulina Cyngot, 2nd Department of Clinical Radiology, University Clinical Centre of Medical University of Warsaw, Poland.
Abstract
Cerebral venous thrombosis (CVT) is uncommon and may often be underrecognized, as well it can be a rare cause of ischemic stroke. Diverse clinical manifestations of CVT may be easily confused with other medical conditions; therefore, brain imaging, such as magnetic resonance imaging (MRI) and computed tomography venography, plays a primary role in diagnosis.
We report a case of a 58-year-old male patient admitted to the stroke unit because of dizziness, dysarthria, gait, and balance problems whose final diagnosis of ischemic stroke due to sinus and cerebral venous thrombosis was established based on the clinical symptoms and radiological findings.
Keywords: cerebral venous thrombosis, ischemic stroke, magnetic resonance imaging
Case Report
A 58-year-old man with no history of hypertension or smoking was admitted to the stroke unit because of dizziness, dysarthria, gait, and balance problems. There was no history of drug use, like anabolic or steroids. The patient denied a recent head or neck trauma. Neurological examination demonstrated the patient's disorientation to an time and dysmetria on the left side. Besides elevated blood pressure (150/110 mmHg) and BMI of 31 kg/m2, his physical study revealed no abnormalities. Body temperature was average, and ECG showed sinus rhythm.
On an admission, a routine nasopharyngeal swab was negative for COVID-19. Laboratory data showed normal levels of CRP (2.8 mg/l reference range: 0.1-10) and WBC (8.3 reference range: 4-10 103/µl). D-dimer level was elevated (1255 ng/ml, reference range: < 500).
A non-enhanced computed tomography (NECT) scan of the head showed slightly decreased density in thalami (Figure 1A) and revealed mild paranasal sinus inflammatory involvement (Figure 1B).
The next day, the patient's neurological status deteriorated; body temperature and CRP increased to 37.8°C and 12.3 mg/l, respectively. A Broad-spectrum antibiotic therapy was introduced to cease infection. A Brain MRI performed at that time revealed bilateral thalamic and basal ganglia T2WI hyperintensities (Figure 1C), with diffusion restriction in both thalami (Figure 1D), consistent with cytotoxic edema. An Angio-MRI after gadolinium contrast agent injection showed sinus and deep cerebral venous thrombosis (Figure 1E).
The final diagnosis of an ischemic stroke due to sinus and deep cerebral vein thrombosis was established. Based on the clinical symptoms and radiological findings, it was also agreed that local infection - an active phase of sinusitis - might be a predisposing factor. Additionally, chest and abdominal CT scans were performed to screen for potential prothrombotic conditions. These showed no evidence of malignancy.
The patient was treated with low molecular weight heparin. During anticoagulant treatment, a follow-up brain MRI on day 8 showed partial normalization of the signal intensity in the basal ganglia (Figure 1F).
During the hospitalization patient's neurological status improved and he was discharged home in good condition, without neurological sequelaea. A Follow-up MRI 5 months later showed a standard signal in deep brain nuclei (Figure 1G) and recanalization of deep cerebral veins and straight sinus (Figure 1H).
Cerebral venous thrombosis (CVT) is uncommon and may be underrecognized. This potentially life-threatening disease accounts for 0.5% to 1% of all strokes in the adult population [1,2]. The estimated incidence of CVT in adults is 13 cases yearly per million people [2]. At least one risk factor is present in 85% of patients with CVT; local infections, including sinusitis, may be associated with this disease [3], but the cause of venous thrombosis in this patient remained unclear.
A Prompt diagnosis and appropriate medical therapy are crucial since parenchymal changes in the brain and venous thrombus formations are potentially reversible [4]. Diverse clinical manifestations of CVT may need to be assesed against other medical conditions. Therefore, brain imaging plays a primary role in diagnosis. MRI and CT venography are instrumental techniques for detecting and confirming the diagnosis of CVT.
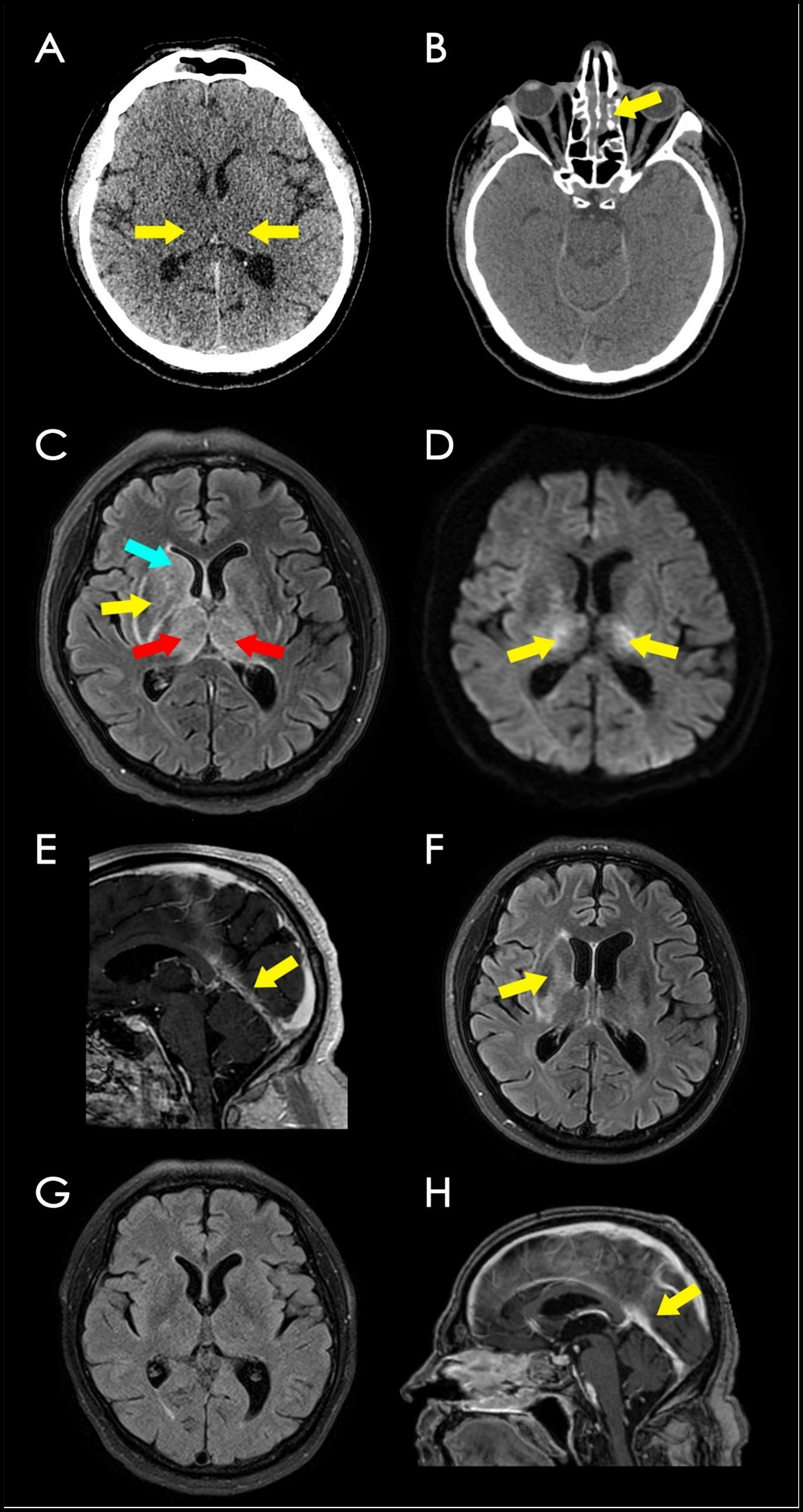
Figure 1.
A. Axial NECT of the brain at the basal ganglia level shows that thalami (yellow arrows) appear isodense to adjacent white matter (early parenchymal changes); no hemorrhage was observed.
B. Axial NECT of the brain shows mucosal thickening in the ethmoidal air cells (yellow arrow).
C. Axial MRI of the brain T2/FLAIR sequence shows the increased signal in both thalami (red arrows) as well as caudate (blue arrow) and lentiform nuclei (yellow arrow) on the right; there is slightly increased signal intensity of the basal ganglia on the left.
D. Axial DWI MR (b1500) reveals diffusion restriction of the thalami, consistent with cytotoxic edema (yellow arrows).
E. Gadolinium-enhanced axial 3D T1WI brain MR shows a filling defect in the internal cerebral veins, vein of Galen, and straight sinus (yellow arrow), corresponding to sinus thrombosis.
F. Axial MRI of the brain T2/FLAIR follow-up on day 8 after anticoagulant treatment shows only slightly increased signal intensity surrounding the right lentiform nucleus (yellow arrow).
G. Axial MRI of the brain T1WI post gadolinium injection after 5 months revealed average signal in basal ganglia.
H. Axial MRI of the brain T1WI post gadolinium injection after 5 months shows no filling defect within the straight sinus (yellow arrow).
List of Abbreviations
BMI - body mass index
ECG - electrocardiogram
CRP - C Reactive Protein
BC - white blood cells
NECT - non-enhanced computed tomography
MRI – Magnetic resonance imaging
CT – Computed tomography
CVT - Cerebral venous thrombosis
Declarations
Ethics approval: Not applicable to this study.
Consent for publication: Not applicable.
Availability of data and materials: Not applicable.
Funding: Our research did not receive grants from internal or external funding agencies.
Conflicts of Interest: All authors declare no conflict of interest
Author's contribution: All authors contributed to this work and read and approved the final version of the manuscript.
References
- Bousser MG, Ferro JM (2007) Cerebral venous thrombosis: an update. The Lancet Neurology. 6(2): 162–70.
- Dmytriw AA, Song JSA, Yu E, Poon CS (2018) Cerebral venous thrombosis: state of the art diagnosis and management. Neuroradiology. 60(7): 669–685.
- Long B, Koyfman A, Runyon MS (2017) Cerebral Venous Thrombosis. Emergency Medicine Clinics of North America. 35(4): 869–878.
- Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF (2006) Imaging of Cerebral Venous Thrombosis: Current Techniques, Spectrum of Findings, and Diagnostic Pitfalls. RadioGraphics. 26(suppl_1): S19–41.



