Akmez Latona MBBS, FACEM1*, Reza Reyaldeen MBBS, FRACP2
1Emergency Department, Princess Alexandra Hospital, Queensland, Australia.
2Department of Cardiology, Princess Alexandra Hospital, Brisbane, Queensland, Australia.
*Corresponding Author: Akmez Latona, MBBS FACEM, Emergency Department, Princess Alexandra Hospital, Queensland, Australia.
Abstract
A 24-year-old presented to the emergency department with chest pain. His cardiovascular risk factors were smoking and a family history of ischemic heart disease. An electrocardiogram showed ST depression at the J point in anterolateral leads and marked down-sloping ST depression. A bedside echocardiogram showed apical wall motion abnormalities and he was taken for coronary angiography which revealed two 90 % left anterior descending artery lesions and treated with drug-eluting stents.
The ECG pattern was suspicious for ‘De Winter T wave’– an under-recognized ECG presentation of acute LAD occlusion. It is characterized by upsloping ST-segment depression by 0.1 mV at V1-V6 leads and tall symmetrical T waves. It is considered by several authors as an anterior ST-elevation myocardial Infarct equivalent, with early cardiac catheter lab activation for percutaneous coronary intervention; however, it is not included in the American Heart Association (AHA) guidelines for urgent reperfusion like STEMI patterns. This may be due to a lack of familiarity with this uncommon ECG manifestation which may reflect a different stage in the ischaemic cascade compared to the classical findings of complete LAD occlusion.
De Winter sign is rare; it is reported only in 2 % of anterior myocardial infarcts. It may be missed by physicians, leading to less aggressive initial management, especially in the young population. This case represents the youngest patient in the literature presenting with this uncommon ECG sign. Early discussion between emergency physicians and cardiologists is imperative in achieving early revascularisation and optimal patient outcome.
Introduction
A 24-year-old male presented to our emergency department with sudden onset, persistent chest pain of 2 hours duration. His cardiovascular risk factors included smoking for 5 years and a family history of ischemic heart disease where his father suffered from a myocardial infarct at the age of 50. His Body Mass Index was 21 kg/m2 and denied any recreational drug use. Further review of symptoms was non-contributory. He was triaged as a category 2 under the Australasian Triage Scale (ATS).
Initial vital signs were temperature 37 °C, blood pressure 137/37, pulse 75, oxygen saturation 99% on room air, and a respiratory rate of 18. He showed no signs of heart failure.
His electrocardiogram (ECG) was grossly abnormal with ST depression at the J-point in V3-V6 continuing into peaked T waves and marked down-sloping inferior ST depression (figure 1 and 2). He was treated for presumed acute coronary syndrome with dual antiplatelet therapy and started on a heparin infusion. Given that his pain persisted, a glyceryl trinitrate infusion was initiated, and he received intravenous opiates.
Urgent bedside echo showed apical wall motion abnormalities. His troponin came back as 25 ug/L He was taken for emergent coronary angiography which revealed two thrombotic 90% mid-left anterior descending artery (LAD) lesions, subsequently treated with 3 drug- eluting stents (figure 3). He was discharged uneventfully from the hospital with aggressive medical therapy and received intensive smoking cessation counselling.
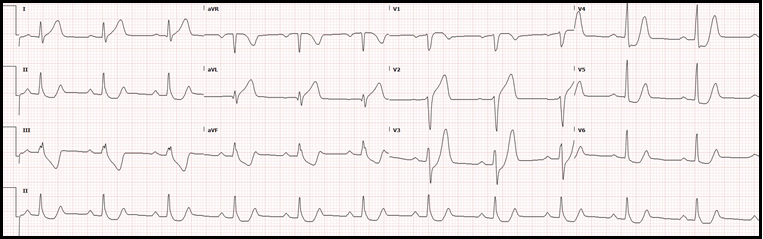
Figure 1: Upsloping ST depression with peaked T waves in anterior leads (De Winter T sign)
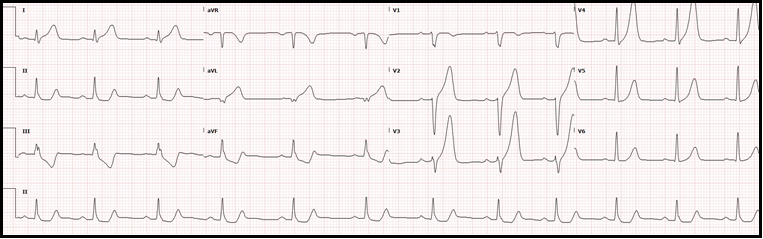
Figure 2: anteroseptal leads – q wave formation with prominent hyperacute T waves
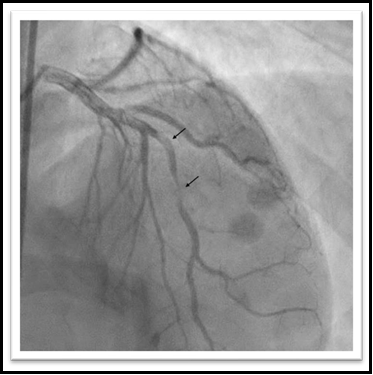
Figure 3: two 90 % mid LAD lesions
Discussion
The ECG pattern in this patient was highly suspicious for ‘De Winter’s sign’ – an uncommon and under-recognized ECG presentation of acute LAD occlusion. It was first reported by de Winter et al 2008 and is considered by several authors as an anterior ST-elevation myocardial infarct equivalent [1]. The main criteria for De Winter sign are upsloping ST-segment depression by 0.1 mV at V1-V6 leads and tall symmetrical T waves [2].
Ideally, De Winter's sign-on electrocardiography should be treated as an ST-elevation myocardial infarct (STEMI) equivalent with early cardiac catheter lab activation for percutaneous coronary intervention [2]. However, despite having a positive predictive value of > 95 % in multiple retrospective cohort studies [1], it is not included in the American Heart Association (AHA) or European Society of Cardiology (ESC) guidelines for urgent reperfusion like traditional STEMI patterns. This may be in part due to a lack of familiarity with this uncommon ECG manifestation which may reflect a different or transient stage in the ischaemic cascade compared to the classical findings of complete LAD occlusion [3]. Whether the De Winter T wave pattern represents a part of the spectrum in the evolution of an anterior STEMI remains debatable. Indeed, it may even be similar to hyperacute T waves which often can be part of the presentation [4], as in our case. Early recognition is essential to reduce total ischemic time and subsequent myocardial damage.
The mean age reported for the De Winter sign-on ECG is 52, compared to that of typical anterior STEMI is 61 [1]. It may be missed by physicians, leading to less aggressive initial management [5]. Thus, in the young population, like our case, a 24-year-old, this sign can be overlooked resulting in suboptimal treatment in a time-sensitive pathology. Serial ECG, frequent clinical assessment, and bedside echocardiography are important in facilitating early coronary angiography.
Conclusion
De Winter sign is rare (~2 % of anterior myocardial infarcts) [1] and is even rarer in the younger population. It should be promptly recognized and treated aggressively to reduce morbidity and mortality. Our case represents the youngest patient in the literature presenting with this uncommon ECG sign. An early discussion between emergency physicians and cardiologists is imperative in achieving early revascularisation and optimal patient outcomes.
Conflict of Interest: None
Funding: None
References
- Raja J, Nanda A, Pour-Ghaz I, Khouzam R (2019) Is early invasive management as ST elevation myocardial infarction warranted in de Winter’s sign? —a “peak” into the widow-maker. Annals of Translational Medicine. 7(17): 412-412.
- Lin Y, Wen Y, Wu G, Xu X (2019) De Winter syndrome, and ST- segment elevation myocardial infarction can evolve into one another: Report of two cases. World Journal of Clinical Cases. 7(20): 3296-3302.
- Alahmad Y, Sardar S, Swehli H (2020) De winter t-wave electrocardiogram pattern due to thromboembolic event: A rare phenomenon. Heart Views. 21(1): 40-44.
- Pranata R, Huang I, Damay V (2018) Should de Winter T-Wave Electrocardiography Pattern Be Treated as ST-Segment Elevation Myocardial Infarction Equivalent with Consequent Reperfusion? A Dilemmatic Experience in Rural Area of Indonesia. Case Reports in Cardiology. 2018: 6868204.
- Zhao Y, Huang Y, Yi Z (2016) de winters ECG changes and anterior myocardial infarction. QJM. 109(4): 269-271.



