Melike YAVAŞ ÇELİK1*, Erhan ELMAOĞLU2
1PhD, Kilis 7 Aralık University, Yusuf Şerefoğlu Health Sciences Faculty, Nursing Department, Karataş Campus, Kilis/TURKEY.
2PhD, Kilis 7 Aralık University, Yusuf Şerefoğlu Health Sciences Faculty, Nursing Department, Karataş Campus, Kilis/TURKEY.
*Corresponding Author: Melike YAVAŞ ÇELİK, PhD, Kilis 7 Aralık University, Yusuf Şerefoğlu Health Sciences Faculty, Nursing Department, Karataş Campus, Kilis/TURKEY.
Introduction
The coronavirus (Covid-19) infection that emerged in Wuhan, China in December 2019 has affected the whole world. The spread of the disease by droplets caused it to spread rapidly. The rapid spread has caused the number of infected people to exceed expected. [10,20]. A short while later, in March, the coronavirus (Covid -19) infection was declared as a pandemic epidemic by WHO [20]. Coronavirus (covid-19) belongs to the same group of viruses that cause Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) [11,21]. The virus causes severe acute respiratory infections and progresses asymptomatic, mild or severe symptomatic. [11,22]. The first case was reported on 11 March 2020 Turkey. As the number of cases increased, various measures began to be taken, and protective measures against the virus continue to be taken. As of October 17, 2020, the total number of reported deaths in the world is 1099586, case number, 39,023,292, and the total number of cases reported in Turkey is 2.12 Mn 19.371 deaths (Turkish Ministry of Health, 2020). Pandemics that remind people of the reality of death can affect people's psychological health quite negatively. Factors such as staying at home continuously in order to protect against the epidemic, the decrease in social relations, when the epidemic process will end or the factors affecting this process may be unknown [18].
In addition, children with additional chronic diseases are in danger not only in terms of Covid-19 infection but also with the disruption of the management of their chronic diseases. For this reason, the management of chronic diseases gains importance during the pandemic period. Although there are differences in the reasons for increasing the susceptibility and severity of chronic diseases to Covid-19, the weakening of immunity seems important in common. Although the underlying chronic diseases of children and adults are different, their sensitivity to Covid-19 is similar. Disorders such as cardiovascular diseases, diabetes, chronic lung diseases, hypertension, and cancer increase the death rate in adults. Additional diseases such as diabetes, adrenal insufficiency, chronic lung diseases, cancers, immune deficiencies, chronic kidney failure, and neurological disorders in children can increase the risk of serious disease and death due to Covid-19. In order to protect such children, necessary measures should be taken during the pandemic process and follow-up ways should be determined. For example, diabetes is known to increase the risk of serious illness and death due to Covid-19 by impairing immunity or due to complications such as hypertension, obesity, cardiovascular diseases, and nephropathy. [14,15]. In general, the effects of SARS-CoV-2 on the CNS may be in the form of direct neurological involvement, worsening of the pre-existing neurological picture, and increasing sensitivity to neurological involvement that will occur due to other reasons or immune-mediated. Since scientific evidence has been obtained that this infection may be responsible for neurological involvement and neurodegenerative conditions in children infected with Covid-19, these children should be closely monitored neurologically [7]. In addition, there is no clear information revealing the effect of Covid-19 on children with epilepsy. For this reason, we aim to share up-to-date information that will constitute a source for the literature and to convey the nursing care process of this case with the case presentation we will present.
Patient Information
De-identified patient-specific information
The patient is 5.5 years old, female, mother and father are unrelated, lives in a nuclear family with 3 siblings. The family lives in a village. The patient was diagnosed with epilepsy at the age of 2 and is using Keppra and depakine suspension.
Primary concerns and symptoms of the patient
The patient, who had no seizures for 1.5 years, started to have seizures at frequent intervals in the last week and applied to the emergency department with fever, weakness, difficulty in speaking, sore throat, inability to walk, decreased vision, cough, diarrhea, vomiting, and respiratory complaints.
Medical, family, and psycho-social history including relevant genetic information
In the emergency room, chest radiography was taken, when suspected, lung tomography was taken and the PRC swab was sent and the patient was taken to the isolation room. The patient was taken to the intensive care unit with the diagnosis of Covid-19 + Lung involvement and ARDS due to the ground glass image in the lung tomography (Figure 1), tachypnea, diffuse rales in the lung, PCR-test positivity (Table 1), and low saturation value and blood gas values not within normal limits. Oxygen was started to be given immediately by connecting to a high flow oxygen (HFNC) device. The patient was consulted with infection, neurology, and metabolism experts.
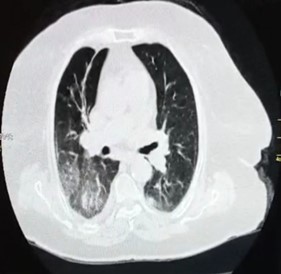
Figure 1: Lung tomography
|
TABLE-1 BLOOD VALUES |
|
|
WBC |
24,88 |
|
RBC |
4,96 |
|
HGB |
8,08g/dL |
|
CREATIN |
0,59 |
|
URIC ACID |
6,34 |
|
AMILASE |
49 |
|
UREA |
39 |
|
PH |
7,20 |
|
CO2 |
58 |
|
PO2 |
80 |
|
HCO3 |
18 |
|
BE |
-5 |
|
CRP |
7,72 |
|
COVİD-19 |
Pozitive |
Relevant past interventions with outcomes
Covid-19 treatment: 0.2 mg/kg Dekort 1x, 2gr / kg IVIG, favipiravir, Kaletra, and clean as well as for the treatment of infection: meropenem, vancomycin, amikacin, fluconazole, Cipro was started, antiepileptics continued as used at home. The patient was started feeding with a nasogastric tube. After the 5th day, the patient's breathing became regular and her fever began to decrease. The PRC test was sent again on the 10th day and when it was negative, the patient was transferred to the neurology service for the continuation of the treatment. The patient stated that he was very scared in the intensive care unit, that the devices made terrible noises all the time, that they did not let him even if he did not want to stay, that the nurses tied his diapers, whereas he wanted to go to the toilet, missed his mother and father very much.
Clinical Findings
1-Perception and Management of Health: The patient applied to the emergency room with symptoms of covid-19 and consecutive seizures. Blood gas values are impaired, the patient's chest X-ray shows a ground glass image. The patient with the impaired gas exchange of the lungs has tachypnea and low saturation. Tomography and PRC test were positive and taken to intensive care. The patient, 1.5 years old, diagnosed with epilepsy, has been using antiepileptics since then. The family does not allow the child to go out because of her chronic illness.
2-Nutrition and Metabolic Status: Height: 110cm, weight: 18kg, the percentile is around 25 % within normal values. There is no problem with growth and development. The child was fed with a nasogastric while in intensive care. She refused to eat the hospital's food when she was taken to the ward and the family started to bring themself the meals. There were wounds in her mouth due to a long-term lack of oral feeding and a high fever.
3-Excretion: She stated that although the child had toilet training while in intensive care, she was troubled by the bonding of the diaper. A urinary catheter is attached to monitor urine output. Since the patient has diarrhea, the diaper is followed up and there is deterioration in the fluid electrolyte values. In addition, they have frequent sweating due to high fever.
4-Activity Exercise: Since the child is very active in intensive care, her hands are tied while receiving treatment with HFNC. When he was taken to the service, the patient was not physically exercised because he was active, but there were problems in his walking due to his last seizure. She is taking HFNC treatment because she has shortness of breath. There is shortness of breath, sweating, and cough increasing with effort. In addition, there are limitations in her movements due to muscle pain and shortness of breath. She does not exercise because she is constantly moving in the service.
5-Cognitive perception: When the sick child came to intensive care, there was a loss of consciousness. He had syncope, serious left-hand trouble. After the treatment period, she started to recover and examine the environment. However, the brain tissues had hallucinations and amnesia due to oxygen loss. He was able to maintain his orientation when he was taken to the service. He communicated with his family and environment.
6-Sleep-rest: She stated that she was disturbed by the sound of the devices and the voices of other patients in the intensive care unit and could not sleep. She also stated that she is used to sleeping with her parents. She stated that she had a hard time crying because they were not. Children in this age range are expected to experience separation-related anxiety, mourning, and longing for them.
7-Self perception: The patient is slightly behind her peers in terms of her development. Ex: No ability to hold tablespoons. However, she is aware of her gender and age. She can comprehend her illness and define more or less what she should do and what she should not do. He gave feedback during the training on methods of protection from Covid-19. He asked questions about the illness.
8-Role and relationship: She had sadness and anxiety as she left her family and home, and the child showed angry and angerful movements due to the painful procedures performed by the nurses and doctors in the intensive care unit. She has not realized that her parents are not with her and is angered by her parents abandoning her. In addition, there were cases when he was afraid of not seeing them again, had nightmares, woke up deliriously as a mother.
9-Sexuality and reproduction: The sick child is sick and aware of his female identity. She also showed shy attitudes while body care was taken. She sees touching her body as a threat. Despite having toilet training due to her diarrhea, she had to be diapered. This situation and the period of illness caused the child to come back and lose his toilet habit.
10-Coping: The child used coping mechanisms such as crying, displaying aggressive behaviors, refusing to speak (speechlessness), thumb sucking, and having nightmares by transferring the fears he suppressed subconsciously to his dreams in response to situations such as intensive care environment and painful procedures, being away from the family. Individuals seek ways to cope with unwanted, anxious, and fearful situations by using defense mechanisms. In our case, he tried to overcome his fears and anxieties by using mechanisms suitable for his age.
11-Beliefs and values: She questions why God makes her sick due to her religious beliefs and feels punished. She kept repeating that she would not do the mischief she did again, but she wanted to heal now. However, since children at this age cannot fully comprehend abstract concepts, the child perceives her situation as a punishment.
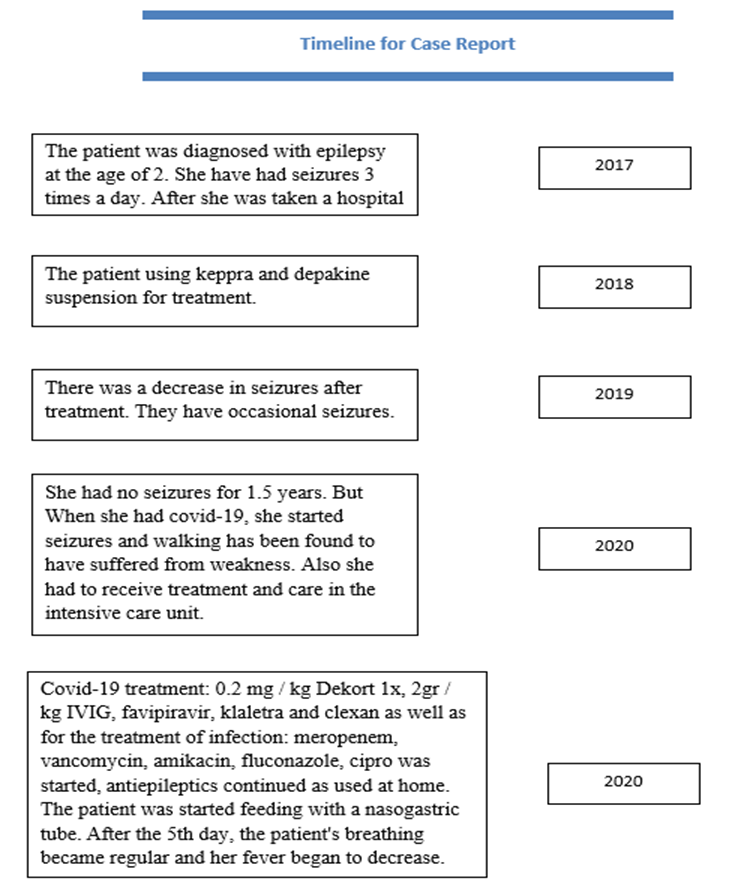
Timeline
Diagnostic Assessment
PCR-test positivity (Table 1) and low saturation value and blood gas values not within normal limits. After the 5th day, the patient's breathing became regular and her fever began to decrease. The PRC test was sent again on the 10th day and when it was negative, the patient was transferred to the neurology service for the continuation of the treatment.
Therapeutic Intervention
1-Perception and Management of Health: Devices were checked to prevent the devices from falling on the patient while the child was in intensive care. The patient was followed closely for the possibility of seizures. The patient does not stop the very mobile nasal high flow cannula in the nose, so his hands are tied. The family is informed about epilepsy and knows what to do during seizures. Even at a young age, the child is partially aware of her illness. She stated that they might faint, so she did not play in the park without her family or someone to accompany her.
2-Nutrition and Metabolic Status: The child was fed with a nasogastric while in intensive care. The height and weight of the patient were followed up. whether the necessary nutrition was provided or not was checked. In order to protect the patient from infections, attention was paid to the cleaning of the feeding catheter. probe changes were made in accordance with antiseptic rules. Before feeding, residue control was made, stomach content was monitored. After the patient left the breathing apparatus, normal nutrition was started. the nutrition of the patient was supported. she could not feed herself yet. Electrolyte values of the patient remained normal.
3-Excretion: the patient was diapered for diarrhea. This situation was explained to the family. The patient's bottom cleaning personal care was done. urine monitoring was done with soda. However, after the catheter, the patient had a problem with incontinence. Kegel exercise was taught to the patient and the patient was followed up. the patient was followed up for a urinary tract infection. fluid intake was supported. In addition, fluid electrolyte values were checked frequently because the patient had frequent sweating.
4-Activity Exercise: The patient's mobility was restricted while in the respiratory support device. Elleir connected. Therefore, extremity controls were observed hourly in terms of circulation. Because of this limitation, the in-bed elevation of the patient was achieved. Follow-up and observations were made in terms of pressure sores.
5-Cognitive perception: The patient was not environmentally-oriented when he first arrived. The consciousness of the patient was monitored. The patient's consciousness started to return to normal after the improvement in blood gas values and breathing. Family visits were increased in order to increase the communication of the patient. They were contacted with their parents in a controlled manner.
6-Sleep-rest: In order to increase the sleep quality of the patient, attention was paid today and night sleep. An environment that is as quiet and less light as possible is created during night shifts. Attempts that could cause pain in the patient were reduced. painful procedures were usually carried out during the day with the support of the family.
7-Self perception: The patient was left behind due to the payoffs of his chronic illness compared to his peers. Therefore, the patient was supported in fulfilling the patient's eating and toilet habits. In addition, she was supported to perform age-specific behaviors on her own and the family was informed about this situation. The family was observed in terms of the perception of fragility. In order to prevent the occurrence of this sensitive situation in the family, the follow-up of the child was shared with the parents, the communication of the child was increased.
8-Role and relationship: The patient could not fully understand the concepts such as separation from the family due to the age period, illness, and death. in this case, it caused him extreme anxiety. Meetings with his family were supported. The family was taken in so that the patient could talk to the family on the phone whenever he wanted and the family was outside, even to calm down the child.
9-Sexuality and reproduction: Despite having toilet training due to her diarrhea, she had to be diapered. This situation and the period of illness caused the child to come back and lose his toilet habit. It is known that there are flashbacks in times of crisis and illness in children. When the patient regained normal values and her diarrhea stopped, toilet training was patiently given without difficulty. The family was informed about this.
10-Coping: The intensive care experience of the child, the concepts of being away from the family, illness, and death have been very difficult for him. The difficult situations he had lived through were explained in a language he could understand by remaining calm, and every question he asked was tried to be answered patiently and the child's concerns were tried to be relieved.
11-Beliefs and values: The child has conceived of his situation as the punishment for him. He wanted his family to abandon him and God back them. In order to support the family, the patient was contacted with the family at any time, and other patients whose disease affected everyone was explained by giving examples.
Some problems experienced by the patient and her family during this period were identified, and nursing diagnoses were determined for these problems.
Nursing Diagnoses
Diagnoses to be made for the child: risk of infection, risk of pressure sores, risk of falling, ineffectiveness in cleaning the airway, impaired communication, fear, anxiety, impaired oral mucous membrane, impaired social interaction, social isolation, impaired speech, hyperthermia, diarrhea, inability to cope.
Diagnoses to be made for the family; deterioration in family processes, inadequacy in the parental role of parents, lack of information about Covid-19 in the family, risk of deterioration in endurance, ineffective social coping, complex suffering, disturbance to sleep pattern.
Follow-up and Outcomes
The patient's blood gas values, vital signs, and the ground glass appearance in the lungs returned to normal. covid -19 positivity in the patient ended. The patient was discharged after receiving the epilepsy treatment in the neurology service and after the necessary information was provided.
Discussion
Children of all age groups mostly had mild respiratory symptoms such as fever, dry cough, and fatigue or it was determined that the children were asymptomatic. In addition, bronchial thickening and ground-glass opacities were the most common radiological findings, and these findings were also reported in asymptomatic patients. No deaths have been reported in children aged 0-9 [3]. Child cases have been reported in 3 different series in China. In the first series, 20 children did not have low-moderate fever or fever, while those with rhinitis, cough, fatigue, headache, diarrhea and severe clinic had dyspnea, cyanosis, and anorexia [4]. Since the patient has diarrhea, the diaper is followed up and there is deterioration in the fluid electrolyte values. In addition, they have frequent sweating due to high fever. Studies have also reported that diarrhea and fever symptoms in the patient are observed in children with Covid-19. [3,16]. There is shortness of breath, sweating, and cough increasing with effort. In addition, there are limitations in her movements due to muscle pain and shortness of breath. She does not exercise because she is constantly moving in the service. Studies have reported shortness of breath that increases with cough and effort, and muscle pain that causes a restriction in movement. [12,16,5,3].
It is reported that Covid-19 is a factor in the occurrence of neurological problems. In addition, it is stated that nervous system involvement may cause an increase in respiratory failure [13]. When the child came to intensive care, there was a loss of consciousness. He had syncope, serious left-hand trouble. This age period depends on his family in many ways [2].
She also stated that she is used to sleeping with her parents. She stated that she had a hard time crying because they were not. Children in this age range are expected to experience separation-related anxiety, mourning, and longing for them. This age period depends on his family in many ways [2].
The patient is slightly behind her peers in terms of her development. Ex: No ability to hold tablespoons. It is known that such behaviors are observed in children with chronic diseases [2]. As parents perceive their children as vulnerable, they act overly protective and prevent their children from gaining skills. [6]. there were cases when he was afraid of not seeing them again, had nightmares, woke up deliriously as a mother.
It has been reported that crises and illnesses disrupt family
relationships, family processes are interrupted in this process, parental roles are disrupted, and children experience behavioral problems. (Mahoney ve MacDonald, 2004; Mahoney et al., 2007) [8]. This situation and the period of illness caused the child to come back and lose his toilet habit. It is known that there are flashbacks in times of crisis and illness in children [2]. Such a problem was also observed in our patient. Individuals seek ways to cope with unwanted, anxiety, and fearful situations by using defense mechanisms [9]. In our case, he tried to overcome his fears and anxieties by using mechanisms suitable for his age. The patient kept repeating that she would not do the mischief she did again, but she wanted to heal now. Taking shelter in God and asking for help is a very common method of relaxation during illness [1].
In this case, the effects of covid-19 were observed in the epilepsy case, which is a chronic disease. The patient had increased epileptic syncopes and walking problems. In addition, she had to receive intensive care treatment for a long time and had a limited process away from the family. During this period, he experienced intense anxiety and feelings such as hopelessness and fear. The patient had symptoms of covid-19 consistent with the literature (fever, shortness of breath, diarrhea, cough, weakness, tachycardia, hyperthermia, tachypnea, rales in the lung, frosted glass image in the lungs), and an increase in syncope was observed. As a result, covid-19 carries fatal risks for children with chronic diseases, and these children need intensive care treatment. These special children need protection and education in the covid-19 pandemic.
Patient Perspective
The patient returned to his normal routine and was discharged. While the patient and his family were being discharged, he said goodbye and thanked his nurse and medical team. During the discharge, the patient was celebrated with applause for defeating covid-19. The smiling face of the patient encouraged the medical team in this war. the routine follow-up of the patient continues and continues to communicate with the healthcare team.
Informed Consent
Because a child is young for approval, we were made approval from her relatives. A case report was made by obtaining approval from the relatives of the patient who was positive for Covid-19. The data were collected through the statements of the family, the information given by the specialist doctor and nurses working in the intensive care unit about the treatment, care process, and observation.
Conflıct of Interest Statement: The authors report no actual or potential conflicts of interest.
References
- Aydın C (2019) Kader İnancinin Savunma Mekanizmasi Ve Dini Başa Çikma Kavramlari Açisindan Değerlendirilmesi. Hitit Üniversitesi İlahiyat Fakültesi Dergisi / Journal of Divinity Faculty of Hitit University. 18(35): 105-126.
- Büyükgönenenç L., Törüner EK. Çocuk Sağlığı Temel Hemşirelik Yaklaşımları. Göktuğ Yayıncılık.Ankara.2015
- Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, et al. (2020) Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review. JAMA Pediatr. 174(9): 882-889.
- Chen ZM, Fu JF, Shu Q, Chen YH, Hua CZ, et al. (2020) Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 16(3): 240-246.
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, et al. (2020) Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics.
- De Ocampo AC, Macias MM, Saylor CF, Katikanemi LD (2003) Caretaker Perception of Child Vulnerability Predicts Behavioral Problems in NICU Graduates. Child Psychiatr Hum Dev. 34(2): 83-96.
- Erdoğan FF. COVID-19 ve çocuk nörolojisi. Uludüz D, Özge A, editörler. Nörolojik Bilimler ve COVID-19. 1. Baskı. Ankara: Türkiye Klinikleri; 2020. p.61-4.
- Gentzler AL, Contreras‐Grau JM, Kern KA, Weimer BL (2005) Parent–Child Emotional Communication and Children's Coping in Middle Childhood. Social Development. 14(4): 599-621.
- Gürhan N. Ruh Sağlığı ve Psikiyatri Hemşireliği. 1. Baskı.2016.Ankara.Nobel Tıp Kitapevi. ISBN: 9786059215145
- Ho CS, Chee CY, Ho RC (2020) Mental Health Strategiesto Combat the Psychological Impact of COVID-19 Beyond Paranoia and Panic. Ann Acad Med Singapore. 16;49(3): 155-160.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 395(10223): 497-506.
- Lu X, Zhang L, Du H, Zhang J, Li YY, et al. (2020) SARS-CoV-2 Infection in Children. N Engl J Med. 382(17): 1663–1665.
- Öztürk Ş (2020) Covid-19 ve Nöroloji. Turk J Neurol. 26: 109-111.
- Remuzzi A, Remuzzi G (2020) COVID-19 and Italy: what next? Lancet. 395(10231): 1225–1228.
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, et al. (2020) Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 323(20): 2052–2059.
- Tezer H, Beder Demirbağ T (2020) Novel coronavirus disease (COVID-19) in children. Turk J Med Sci. 50(SI-1): 592-603.
- Türkiye Cumhuriyeti Sağlık Bakanlığı.2020.
- Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A (2020) The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry. 66(4): 317-320.
- World Health Organization. Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: interim guidance. 2020.
- WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020.
- Zhonghua liu xing bing xue za zhi.= Zhonghua liuxingbingxue zazhi. Novel CPERE. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases(Covid-19) in China. 2020; 41(2): 145-151.
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al. (2020) A novel coronavirus from patients with pneumonia in China. N Engl J Med. 382(8): 727-733.



