Thierry Sibomana1*, Désiré Nisubire2, Benny Field Kimana1, Jean Claude Mbonicura3, Tharcisse Gasogo4, Thierry Ingabire5, Jean Claude Nkurunziza6
1Internal Medicine-Pulmonology department, University of Burundi, faculty of Medicine
2Laboratory department, University of Burundi, faculty of Medicine
3General Surgery department, University of Burundi, faculty of Medicine
4Medical Biology department, University of Burundi, faculty of Medicine
5Internal Medicine-Infectiology department, University of Burundi, faculty of Medicine
6Public Health department, University of Burundi, faculty of Medicine
*Corresponding Author: Thierry Sibomana; Internal Medicine-Pulmonology department, University of Burundi, faculty of Medicine. Orcid Number: 0000-0001-7042-1546.
Abstract
Background: Tuberculosis (TB), a transmissible disease caused by Mycobacterium tuberculosis, remains a major public health problem with nearly 8 million new cases each year and more than 1 million deaths per year. The WHO recommends the use of rapid molecular tests for the initial diagnosis of all people presenting signs and symptoms of tuberculosis. These tests are highly reliable and will enable considerable progress to be made in the early detection of cases of tuberculosis and drug-resistant tuberculosis.
Aims: Our study aimed to evaluate the contribution of the Xpert MTB/RIF test in the diagnosis of pleuropulmonary tuberculosis at Kamenge University Hospital (CHUK).
Methods: This was a retrospective descriptive and analytical study conducted from 1 March 2018 to 31 December 2021 in the Mycobacteriology Department of the Kamenge University Hospital in Bujumbura. All pleuropulmonary specimens for which an Xpert MTB/RIF test was requested were included in the study, regardless of the patient's age.
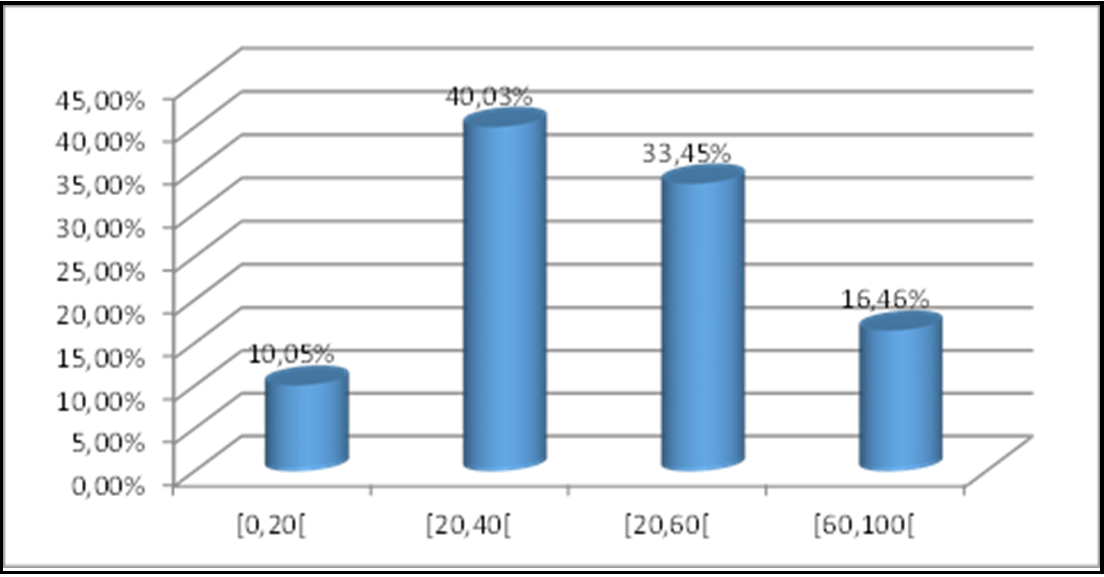
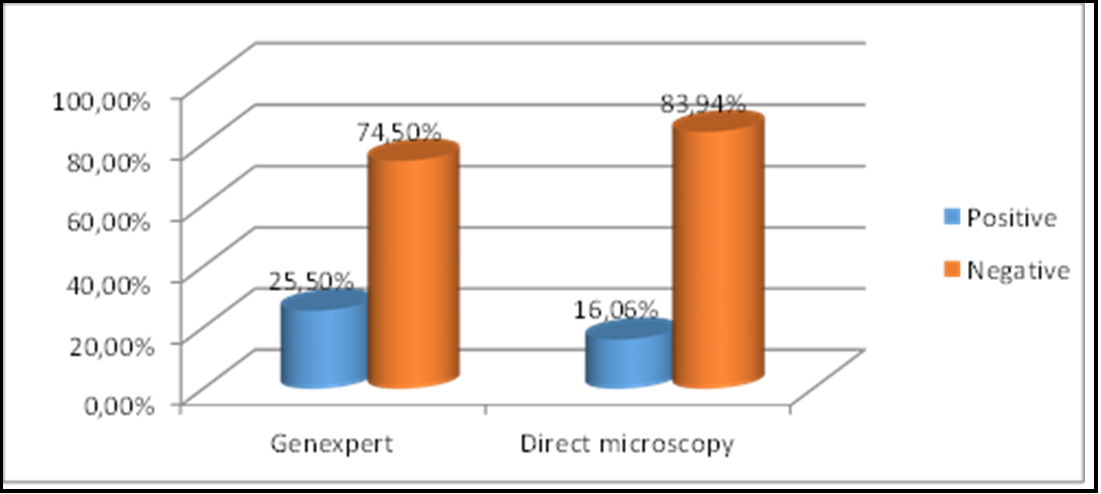
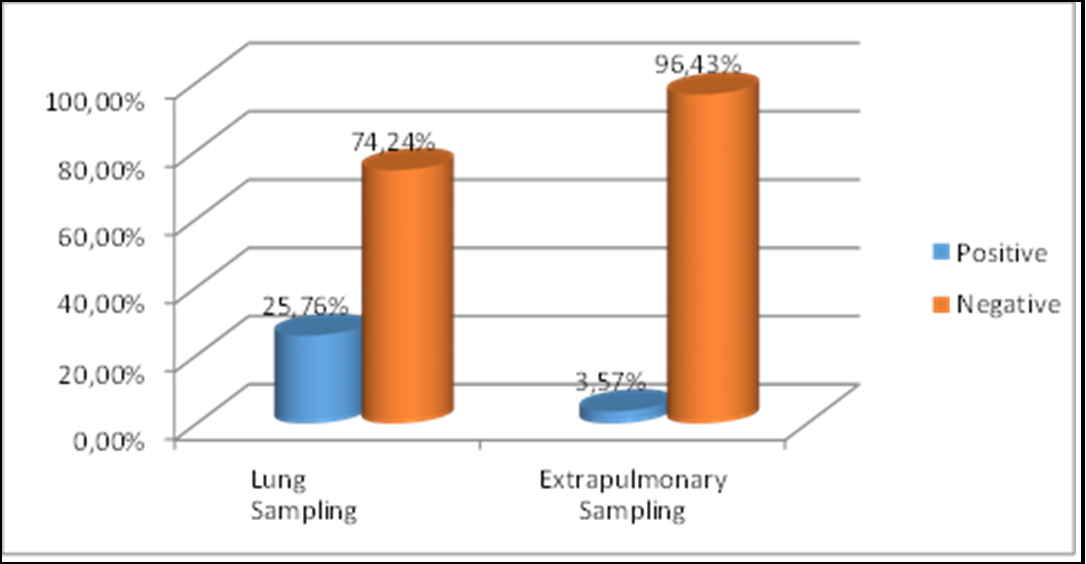
Results: During the study period, 577 patients suspected of having pleuropulmonary tuberculosis underwent an Xpert MTB/RIF test, of whom 130, or 22.53%, were positive. The majority of patients were men, with a sex ratio of 1.2. The average age was 40.4, with extremes of 1 and 95. The most represented age group was 20 to 40, with a percentage of 40.3%. The vast majority of samples were sputum (85.10%). Direct microscopy was positive in 80 cases out of 498 samples, i.e., a detection rate of 16.06%, whereas the Xpert MTB/RIF test had a detection rate of 25.5% on samples that had undergone both direct microscopy and the Xpert MTB/RIF test. Out of the 130 strains of Mycobacterium tuberculosis detected, 2 were resistant to rifampicin (1.54%). Most of our samples showed a positive Xpert MTB/RIF test at medium intensity, i.e., a total of 50 (38.46%). The Xpert MTB/RIF positivity rate was higher in samples of pulmonary origin.
Conclusion: The Xpert MTB/RIF test performed significantly better than direct microscopy in detecting pleuropulmonary tuberculosis. It would therefore be reasonable to make it more accessible in the country's various laboratories.
Keywords: Xpert MTB/RIF, Pleuropulmonary tuberculosis, Kamenge University Hospital
Introduction
Tuberculosis, a transmissible disease caused by Mycobacterium tuberculosis, remains a major public health problem. Until the 2019 coronavirus pandemic (COVID-19), tuberculosis was the leading cause of death due to an infectious agent, ranking above HIV/AIDS [1].
The disease generally affects the lungs (pulmonary tuberculosis) but can also have other locations (extrapulmonary tuberculosis). Around a quarter of the world's population is infected with M. tuberculosis [1].
It is estimated that, worldwide, 9.9 million people contracted tuberculosis in 2020: 5.5 million men, 3.3 million women and 1.1 million children. Tuberculosis affects all countries and all age groups, but it is a preventable and curable disease [2]. Earlier and better detection of tuberculosis cases, including smear-negative cases often associated with HIV, and the development of diagnostic capacity for multidrug-resistant tuberculosis (MDR-TB) are global priorities in the fight against tuberculosis [3].
Multidrug-resistant tuberculosis (MDR-TB) poses enormous difficulties due to the complexity of its diagnosis and treatment, while HIV-associated tuberculosis is not frequently diagnosed due to the limitations of current diagnostic techniques [3].
The alarming resurgence of MDR-TB, the global emergence of extensively drug-resistant TB (XDR-TB), the proven transmission in institutions and the rapid mortality of MDR-TB or XDR-TB in HIV co-infected patients have highlighted the urgent need for rapid diagnostic methods [3].
The WHO recommends the use of rapid molecular tests for the initial diagnosis of all people presenting signs and symptoms of tuberculosis. These tests are highly reliable and will enable considerable progress to be made in the early detection of cases of tuberculosis and drug-resistant tuberculosis. The following molecular tests are recommended by the WHO: Xpert MTB/RIF, Xpert Ultra and Truenat [2].
The introduction of new tools, essentially molecular biology tools, including the Xpert MTB/RIF test, whose use has been approved since December 2010 by the WHO, has increased sensitivity and above all shortened the time required to confirm tuberculosis [4,5].
Since the Centre Hospitalier Universitaire de Kamenge acquired the equipment needed to perform the Xpert MTB/RIF test, we have set ourselves the objective of evaluating its performance in the diagnostic management of pleuropulmonary tuberculosis and rifampin resistance.
Patients and methods
This was a retrospective descriptive and analytical study conducted from 1 March 2018 to 31 December 2021 in the Mycobacteriology Department of Kamenge University Hospital in Bujumbura. Ethics Committee permission was previously requested from the administrative authorities of the hospital before conducting our study and was granted on 20.01.2022. The study included all pleuropulmonary samples for which an Xpert MTB/RIF test had been requested, regardless of the patient's age. The data were collected from the register of the CHUK Mycobacteriology Laboratory.
Statistical Analysis
Text prEpi info 7.2 software ocessing was performed using Microsoft Word version 2016. Data entry and analysis were performed using Epi info 7.2 software
Results
During the study period, 577 patients suspected of having pleuropulmonary tuberculosis underwent Xpert MTB/RIF testing, of whom 130 were positive, i.e., a frequency of 22.53%. The majority of patients were men, with a sex ratio of 1.2. The average age was 40.4, with extremes of 1 and 95. The most represented age group was 20 to 40, with a percentage of 40.3%. The vast majority of samples were sputum (85.10%). Direct microscopy came back positive in 80 cases out of 498 samples, i.e., a detection rate of 16.06%, whereas the Xpert MTB/RIF test had a detection rate of 25.5% on samples that had undergone both direct microscopy and the Xpert MTB/RIF test. Out of 130 strains of Mycobacterium tuberculosis detected, 2 were resistant to rifampicin (1.54%). Most of our samples showed a positive Xpert MTB/RIF test at medium intensity, i.e., a total of 50 (38.46%). The Xpert MTB/RIF positivity rate was higher in samples of pulmonary origin.
Table I: Patient distribution by age group
Table II: Distribution according to Bacilloscopy test results compared with Xpert MTB/RIF
Table III: Distribution of positive Xpert MTB/RIF tests by sample type
Discussion
We conducted a retrospective descriptive and analytical study analyzing the contribution of Genexpert MTB/RIF in the diagnosis of pleuropulmonary tuberculosis at Kamenge University Hospital in Bujumbura. From March 2018 to December 2021, the Xpert MTB/RIF test was performed on 577 patients suspected of having pleuropulmonary tuberculosis, 130 of whom returned positive, a frequency of 22.53%. Our study showed that 498 samples benefited from both direct microscopy and Xpert MTB/RIF testing. The positivity rate of the Xpert MTB/RIF test in these samples was 25.50%, which is higher than the positivity rate of direct microscopy, which was 16.06%.
Of the 418 smear-negative samples, 47 were Xpert MTB/RIF positive, giving a Xpert MTB/RIF positivity rate of 11.24%.
These results demonstrate a better performance of Xpert MTB/RIF over smears in our study. Xpert MTB/RIF therefore appears to provide added value in the diagnosis of tuberculosis cases not identified by microscopy. Diop et al. [9] found an Xpert MTB/RIF positivity rate of 65% in a series of 94 cases in Senegal. Most studies on Xpert MTB/RIF confirm the performance of this test compared with bacilloscopy. In Tanzania, Rachow et al. [6] detected 11 Xpert MTB/RIF-positive samples among 18 bacilloscopy-negative samples, with a significant difference (p = 0.001).
Zeka et al. [7] in Turkey, in their cohort of 429 patients, found a positivity rate of 68.9% (24 / 35) on smear-negative lung samples.
The vast majority of samples were sputum (85.10%). The predominance of pulmonary samples is linked to the fact that tuberculosis is a disease with a predominant respiratory tropism.
Of 493 lung samples, 25.76% were positive for Xpert MTB/RIF, and of 84 extra-lung samples (pleural fluid), 3.57% were positive for Xpert MTB/RIF. This difference was statistically significant (p- value<0.0001), enabling us to conclude that Xpert MTB/RIF was most frequently positive on lung samples, compared with extra-lung samples.
In our study, most samples were Xpert MTB/RIF positive at moderate intensity, with a total of 50 (38.46%). On the other hand, we found that a negative preliminary bacilloscopy in a suspected tuberculosis case may indicate a paucibacillary specimen, irrespective of gender. We also observed that the intensities for smear-positive specimens were higher than for smear-negative specimens. This is also what Ndoye [8] found in Senegal.
The male predominance found in our study (sex ratio=1.6) and by Diop et al. [9] (sex ratio=1.6) is in line with the epidemiology of the disease in Burundi and most African countries.
Our results resembled those of Borgdorff et al. [10] and other data in the literature, unlike those of Ajmi et al. [11], who showed that tuberculosis affects both genders equally. According to Holmes et al. [12], these observations point to the possibility that TB cases in women are under-reported in developing countries. This idea is reinforced by the results of a study comparing active and passive screening, where it appears that in the case of passive screening, women with tuberculosis are under-reported to public health authorities.
The average age of 40 was close to the average age of 41, as noted by Diop et al. [9]. The [20 - 40] and [40 - 60] age groups predominated, accounting for 73.48% of the population. These data were in line with the findings of Ajmi et al. [11], who showed that tuberculosis predominantly affects the 30-44 age group (28.4%). This is justified by the fact that in this age group, pneumopathies are often of infectious origin, particularly tuberculosis. Any request for Xpert MTB/RIF is more likely to come back positive.
Overall, studies carried out in Africa and developed countries (Agadokpessi et al. [13] in Benin, Rachow et al. [6] in Tanzania, Gagnière et al. [14] in Brittany and Valin et al. [15] in France) show that tuberculosis predominates in young adults, with a peak in frequency between the ages of 31 and 45. This population is at risk due to its active and dynamic nature, making tuberculosis an obstacle to economic development.
With regard to rifampicin resistance, we found that out of 130 Xpert MTB/RIF-positive samples, 2 were rifampicin-resistant, i.e., a rate of 1.54%, which was lower than that noted by Diop et al. [9] (3.5%) and by Sauzullo et al. (3.4%) in Rome [16].
Our results showed a predominance of sensitivity in smear-positive subjects compared with smear-negative subjects. However, these results were not statistically significant (p-value = 0.893).
Conclusion
Tuberculosis is a major public health problem worldwide. Its control has become increasingly difficult with the emergence of multidrug- resistant and even extensively drug-resistant strains. We found that Xpert MTB/RIF performed significantly better than direct microscopy in detecting tuberculosis and that making this test more accessible and using it systematically in conjunction with bascilloscopy would enable us to better control tuberculosis in our environment and limit its complications.
References
- Organisation Mondiale de la Santé (2021) Rapport sur la tuberculose dans le monde 2021. Genève, 2021.
- Organisation Mondiale de la Santé, Tuberculose.
- Organisation Mondiale de la Santé, (2011) Mise en oeuvre rapide du test diagnostique Xpert MTB/RIF :Guide technique et opérationnel Considérations pratiques. Genève.
- Ninet B, Roux-Lombard P, Schrenzel J, Janssens JP (2011) Nouveaux tests pour le diagnostic de la tuberculose. Rev Mal Respir. 28(6): 823 833.
- Truffot-Pernot C, Veziris N (2011) Les tests bactériologiques de la tuberculose maladie: standards et perspectives. Rev Ma Respir. 28(8): 1034 1047.
- Rachow A, Zumla A, Heinrich N, Rojas-Ponce G, Mtafya B, et al. (2011) Rapid and accurate detection of Mycobacterium tuberculosis in sputum samples by Cepheid Xpert MTB/RIF assay—a clinical validation study. PloS One. 6(6): e20458.
- Zeka AN, Tasbakan S, Cavusoglu C (2011) Evaluation of the GeneXpert MTB/RIF assay for rapid diagnosis of tuberculosis and detection of rifampin resistance in pulmonary and extrapulmonary specimens. J Clin Microbiol. 49(12): 4138 4141.
- N. B. Ndoye (2018) Apport du Genexpert dans le diagnostic de la tuberculose toutes formes confondues. Université Cheikh Anta Diop. Dakar.
- Diop SA, Massaly A, Ka D, Manga NM, Fortes-Déguénonvo L, et al. (2016) Utilisation du test GeneXpert pour le diagnostic de la tuberculose au service des maladies infectieuses du CHNU de Fann. Pan Afr. Med. J. 23: 244.
- M. W. Borgdorff, N. J. D. Nagelkerke, C. Dye, et P. Nunn, (2000) Genre et tuberculose: une comparaison entre les enquêtes de prévalence et les données de déclaration pour explorer les différences entre sexes dans la détection des cas. Int J Tuberc Lung Dis. 4(2): 123-132.
- Ajmi T, Tarmiz H, Bougmiza I, Gataa R, Knani H, et al. (2010) Profil épidémiologique de la tuberculose dans la région de sanitaire de Sousse de 1995 à 2005. Rev Tunis D’Infectiologie- Janvier. 4: 18-22.
- Holmes CB, Hausler H, Nunn P (1998) A review of sex differences in the epidemiology of tuberculosis. Int J Tuberc Lung Dis. 2(2): 96-104.
- Agodokpessi G, Ade G, Ade S, Wachinou AP, Affolabi D, et al. (2012) Management of tuberculosis and HIV co-infection in Cotonou, Benin. Médecine Mal. Infect. 42(11): 561-566.
- Gagnière B, Le Goff-Mevel D, Marquis M, Guillois-Bécel Y, Mari C, et al. (2011) Épidémiologie de la tuberculose en Bretagne:les cas déclarés entre 2000 et 2007. Médecine Mal. Infect. 41(1): 33-37.
- Valin N, Chouaïd C (2012) La tuberculose en France en 2010: épidémiologie, clinique et microbiologie. Rev Mal Respir. 29(2): 267 276.
- Sauzullo I, Rodio DM, Facchinetti S, Puggioni G, De Angelis M, et al. (2016) Diagnostic accuracy of Xpert MTB/RIF versus smear microscopy in the early diagnosis tuberculosis in the real life of "Umberto I" Hospital Rome. New Microbiologica. 39(4): 304- 306.