Mladen Kasalović1*, Nikola Miljković1, Aleksandar Jakovljević1, Gojko Igrutinović2, Zlatan Elek2
1Clinical Hospital Center Kosovska Mitrovica, Surgical Clinic, Kosovska Mitrovica, Serbia
2University of Priština-Kosovska Mitrovica, Faculty of Medicine-Department of Surgery, Kosovska Mitrovica, Serbia
*Corresponding Author: Mladen Kasalović, Clinical Hospital Center Kosovska Mitrovica, Surgical Clinic, Kosovska Mitrovica, Serbia.
Abstract
Introduction: This study provides an in-depth analysis of acute cholecystitis and pancreatitis, focusing on demographic characteristics, biological parameters, and risk factors in 130 patients.
Methods: A total of 130 patients participated (mean age 51 years), with 56 having acute cholecystitis and 74 acute pancreatitis. Various biological parameters, including cholesterol, triglycerides, AST, ALT, GGT, WBC, NE%, and PLT, were analyzed. Statistical analyses included t-tests, Chi-square tests, Mann-Whitney U tests, and linear regressions.
Results: In a study involving 130 patients (56 acute cholecystitis, 43.10%; 74 acute pancreatitis, 56.90%), demographic data revealed no significant age differences. However, a notable gender difference was observed, with males being more prone to pancreatitis (p=0.010). Risks of cholecystitis were associated with a significant increase in C-reactive protein (CRP) levels (p=0.0001) and male gender (p=0.010). Age and cholesterol were not significant factors. For pancreatitis, the initial accuracy of 56.9% improved to 80.0% with the inclusion of factors such as statins, gender, CRP, cholesterol, ALT, and AST. CRP, ALT, and AST demonstrated statistical significance (p<0.05), suggesting their potential contributions, while other factors were not statistically significant.
Conclusion: Our study emphasizes the significance of C-reactive protein (CRP) in diagnosing pancreatitis, indicating statistically significant associations between risk factors such as patient gender and CRP levels in acute cholecystitis. Despite study limitations, these results provide important insights for the diagnosis and monitoring of these conditions, underscoring the need for further research in the field of gastroenterology.
Keywords: acute cholecystitis, acute pancreatitis, C-reactive protein, risk factors
Introduction
Acute cholecystitis induces acute abdominal pain and may require emergency surgery or intensive antibiotic therapy and percutaneous drainage, depending on the patient's condition [1]. Early diagnosis of acute cholecystitis is crucial for achieving favorable outcomes [1]. Reported mortality from acute cholecystitis is approximately 3%, but the rate increases with age or patient comorbidity [2]. Early diagnosis and staging of acute cholecystitis enable prompt treatment, reducing mortality and morbidity [3]. C-reactive protein (CRP), white blood cell count (WBC), and platelet count (PLT) are well-known hematologic and biochemical predictors of severe inflammation [3]. Acute pancreatitis has an overall low mortality, around 1% [4]. The risk of death increases with age, accompanying diseases, and severe conditions; in a recent meta-analysis, the risk of death was highest among patients with organ failure and infected necrosis [4].
The study aims to:
Examine Demographic Differences: Analyze the demographic characteristics of patients with acute cholecystitis and acute pancreatitis to understand if there is a significant difference in age and gender between these two groups.
Identification of Risk Factors: Determine risk factors that may be associated with the occurrence of acute inflammation of the gallbladder and pancreas.
Evaluation of the Significance of Inflammatory Markers: Investigate the role of inflammatory markers, especially CRP, in the diagnosis of acute inflammation of the gallbladder and pancreas.
Association between Gender and Inflammation: Explore the relationship between the gender of patients and the development of acute inflammation, especially pancreatitis, to understand if gender can be a significant risk factor in these conditions.
Assessment of the Complexity of Risk Factors: Analyze the complexity of risk factors contributing to the development of acute inflammation of the gallbladder and pancreas.
Methodology
The research was designed as a retrospective study. We opted for this design to analyze data from the medical records of patients who had already undergone diagnostic procedures and treatment. This allowed us to gather data on a large number of patients with diverse characteristics.
The sample consisted of 130 patients diagnosed with acute cholecystitis or acute pancreatitis. All participants were patients in our medical institution, and their data were accessible in health records. The average age of the participants was 51 years, with 77 participants being male and 53 female.
Data were collected from patients' health records. For the analysis of demographic characteristics, including gender and age, we used basic information from health records. We also recorded laboratory parameters such as cholesterol, triglycerides, AST, ALT, GGT, total white blood cell count (WBC), percentage of neutrophils (NE%), and platelet count (PLT).
For data analysis, various statistical methods were employed. To analyze differences between groups of patients with different conditions, we used the independent samples t-test for age analysis, and the Chi-square test for gender analysis. To explore biological differences, we applied the Mann-Whitney U test for an independent sample on a set of biomarkers. For the analysis of risk factors, linear regression was used to assess the relationship between the presence of the disease and various factors.
The research was conducted in accordance with ethical guidelines and approval from the institutional ethical committee.
After data collection, analysis and interpretation were performed to draw key conclusions about the differences between acute cholecystitis and acute pancreatitis, as well as the associated risk factors.
Results
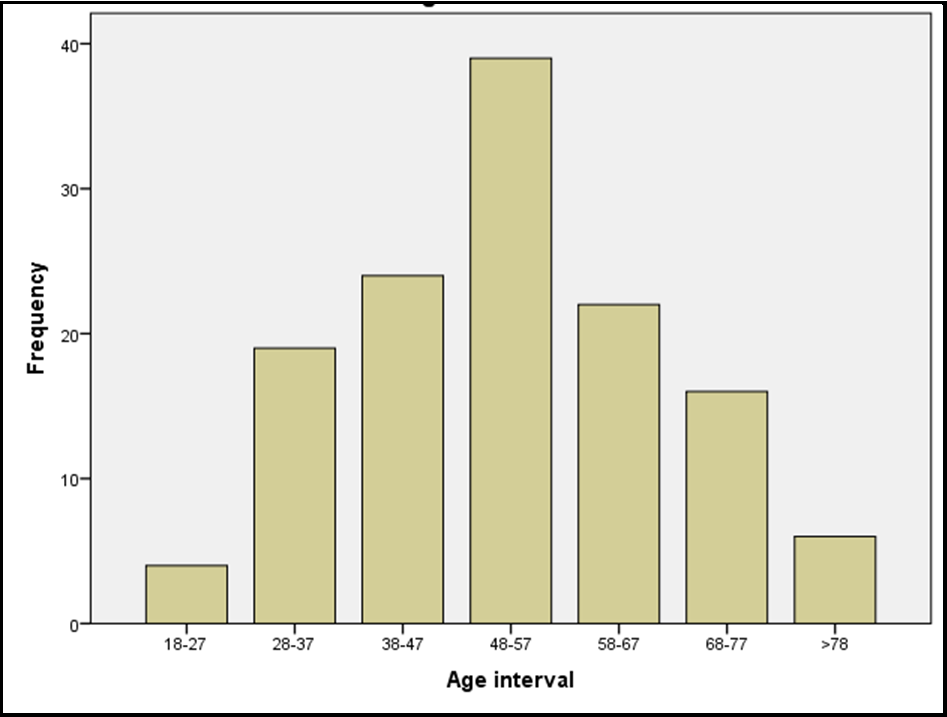
This research presents extensive findings from a study focused on analyzing differences and interrelationships between various variables in patients suffering from acute cholecystitis and acute pancreatitis. The study involved 130 patients with a mean age of 51 years, including 77 males and 53 females. Out of the total number of patients, 56 (43.10%) were diagnosed with acute cholecystitis, while 74 (56.90%) were diagnosed with acute pancreatitis. The age distribution of the participants is depicted in Chart 1.
Chart 1: Age Distribution of Patients
In the investigation of demographic characteristics in patients with acute cholecystitis and acute pancreatitis, no statistically significant differences in age were found (t-test, p=0.481) between these groups of patients (average age of 52 years). However, the study revealed a statistically significant difference in the gender of patients. Specifically, male patients were more prone to pancreatitis compared to cholecystitis, indicating gender as a potential risk factor for the development of pancreatitis (Chi-square test, p=0.010). These findings suggest that both conditions are prevalent in different age groups, with gender being a significant differentiator.
To explore potential biological differences between patients with acute cholecystitis and acute pancreatitis, we analyzed a series of biological parameters, including cholesterol, triglycerides, AST, ALT, GGT, total white blood cell count (WBC), percentage of neutrophils (NE%), and platelet count (PLT). The results showed that none of these parameters showed statistically significant differences (Mann-Whitney U test) between both conditions. Cholesterol (p=0.563), triglycerides (p=0.033), AST (p=0.0001), ALT (p=0.219), GGT (p=0.004), WBC (p=0.064), NE% (p=0.004), and PLT (p=0.007) did not exhibit statistically significant differences between patients with acute cholecystitis and acute pancreatitis. These results suggest that there are no biological differences in these parameters directly associated with the development of these conditions.
The analysis of risk factors for acute cholecystitis provided important insights. Firstly, the research results revealed a statistically significant association between the presence of cholecystitis and C-reactive protein (CRP) levels (linear regression, p=0.0001). This implies that elevated CRP values are strongly linked to the presence of cholecystitis, with each increase in CRP value increasing the likelihood of cholecystitis by approximately 2.8 times. This is significant information for clinical diagnosis and assessment of this condition. Another significant risk factor is the gender of patients (linear regression, p=0.010). Statistical significance indicates a connection between gender and the presence of cholecystitis. More precisely, the results indicate that males are more prone to developing cholecystitis compared to females. This finding provides additional information for assessing risk factors in the context of this condition.
It is important to note that other variables, such as age and cholesterol, did not show statistical significance in this model (linear regression, p-values greater than 0.05). This suggests that these variables are not crucial risk factors for the development of cholecystitis within this study.
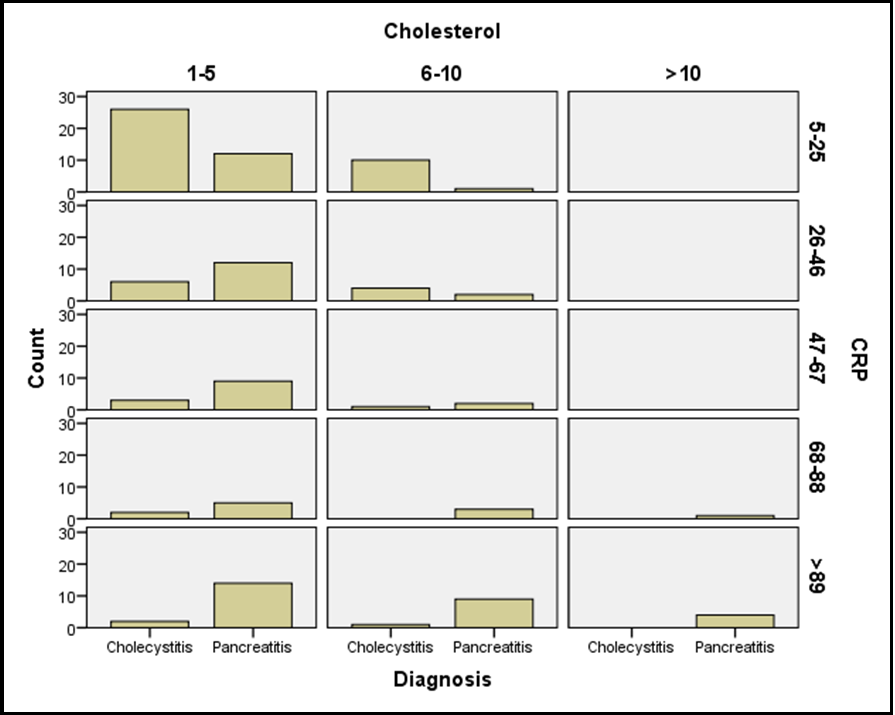
The analysis of risk factors for acute pancreatitis reveals key conclusions. The initial model showed a relatively low percentage of correct predictions for the presence of pancreatitis at 56.9%. However, after certain factors were included in the model (Step 1), the accuracy of predictions significantly improved to 80.0%. This significant improvement indicates the importance of these factors in the precise diagnosis of pancreatitis. The final model for pancreatitis included various variables, including the use of statins, gender, CRP, cholesterol, ALT, and AST. The relationship between these conditions and certain biomarkers is depicted in Chart 2. However, most of these variables did not show statistical significance (linear regression, p-values greater than 0.05), suggesting that there are no statistically significant associations between these variables and the presence of pancreatitis. It is important to note that factors such as CRP, ALT, and AST showed statistical significance (linear regression, p-values less than 0.05), suggesting their potential contribution to pancreatitis.
Chart 2: Relationship between Diseases and Biological Markers
Discussion
Our study contributes to an enhanced understanding of risk factors and biological differences between acute cholecystitis and acute pancreatitis, adding value to the current knowledge of these conditions. C-reactive protein (CRP) emerges as a notable acute-phase reactant produced by hepatocytes in response to systemic inflammatory markers such as interleukin 6 (IL-6) [5]. Our study confirms a statistically significant association of CRP with pancreatitis, aligning with findings from other research, including Tarar et al. [5] and Lin et al. [6], emphasizing elevated CRP as a risk factor for pancreatitis. Similar correlations were observed for Aspartate Aminotransferase (AST) and Alanine Aminotransferase (ALT), consistent with Liu et al.'s research [7].
Concerning cholecystitis, our study did not find a statistically significant correlation between White Blood Cells (WBC) and Neutrophil Percentage (NE%), although literature, like Jones et al., suggested the significance of WBC in individual conditions like cholecystitis [8]. However, our results show a statistical correlation of WBC, NE%, and CRP with cholecystitis, supporting previous research emphasizing their relevance [3].
Regarding cholesterol levels, our study does not confirm a pivotal role in the risk of developing cholecystitis, while other studies, such as Yang et al. [9], demonstrated a connection above reference values with the risk of cholecystitis, with contradictory findings in another research [3].
Our study brings significant advantages to understanding acute cholecystitis and pancreatitis. Firstly, we thoroughly analyzed risk factors and biological differences, providing a comprehensive overview of their complexity. This approach deepens the understanding of clinical characteristics and potential mechanisms of their development. Secondly, our results contribute to existing knowledge on these conditions, enriching the current literature. This knowledge is valuable for gastroenterology experts and the broader medical community. Thirdly, we explored and identified biological markers like C-reactive protein (CRP) and white blood cells (WBC), emphasizing their potential in the diagnosis and monitoring of these conditions. These findings can directly impact improving the approach to diagnosing and treating patients with acute inflammation of the gallbladder and pancreas.
Despite these advantages, our study has certain limitations. Firstly, the retrospective design limits the interpretation of results as we rely on existing medical records. These limitations may affect the accuracy and completeness of the collected data. Secondly, the sample of 130 patients may be considered limited, impacting the generalizability of our conclusions to a broader population. A larger sample would allow for broader applicability of our findings. Finally, while we identified biological markers, we did not conduct additional experimental analyses to confirm specific mechanisms of action. This limitation highlights the need for future research to deepen the understanding of the biological aspects of these conditions.
Conclusion
Our study provides a valuable contribution to the understanding of acute cholecystitis and pancreatitis by analyzing risk factors and biological differences among patients. In-depth analysis of demographic characteristics, biological markers such as C-reactive protein (CRP) and white blood cells (WBC), and the identification of risk factors enable a comprehensive overview of these conditions.
Our study emphasizes the significance of C-reactive protein (CRP) as a reliable indicator for diagnosing pancreatitis, aligning with previous research. Additionally, we observe a statistically significant association between risk factors, such as patient gender, and levels of C-reactive protein (CRP), with acute cholecystitis.
However, we acknowledge the limitations of our study, including its retrospective design and a restricted sample size, which may impact result generalizability. Despite these limitations, our findings provide additional insights into the diagnosis and monitoring of acute inflammation of the gallbladder and pancreas, highlighting the need for further research to expand the understanding of these complex gastroenterological conditions.
References
- Ikeda H, Ohta R, Sano C (2022) Risk Factors for Delayed Diagnosis of Acute Cholecystitis among Rural Older Patients: A Retrospective Cohort Study. Medicina (Kaunas). 58(10): 1392.
- Lee SO, Yim SK (2018) Management of Acute Cholecystitis. Korean J Gastroenterol. 71(5): 264-268.
- Kasalović M, Jakovljević A, Igrutinović G, Miljković N, Rakić D, et al. (2023) Assessment of the risk for cholecystitis when performing laparoscopic cholecystectomy in a retrospective cohort study: Assessment of the risk for cholecystitis. J Surg Med. 7(7): 413-415.
- Yadav D, Lowenfels AB (2013) The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 144(6): 1252-61.
- Tarar MY, Khalid A, Choo XY, Khurshid S, Tumeh H, et al. (2022) Use of the C-Reactive Protein (CRP)/Albumin Ratio as a Severity Tool in Acute Pancreatitis: Systematic Review. Cureus. 14(9): e29243.
- Lin XY, Zeng Y, Zhang ZC, Lin ZH, Chen LC, et al. (2022) Incidence and clinical characteristics of hypertriglyceridemic acute pancreatitis: A retrospective single-center study. World J Gastroenterol. 28(29): 3946-3959.
- Liu W, Du JJ, Li ZH, Zhang XY, Zuo HD (2021) Liver injury associated with acute pancreatitis: The current status of clinical evaluation and involved mechanisms. World J Clin Cases. 9(34): 10418-10429.
- Jones MW, Genova R, O'Rourke MC (2023) Acute Cholecystitis. Treasure Island (FL): StatPearls Publishing.
- Yang H, Chen L, Liu K, Li C, Li H, et al. (2021) Mendelian randomization rules out the causal relationship between serum lipids and cholecystitis. BMC Med Genomics. 14(1): 224.