Adrián P. Dévoli1, Maura Gianninoto 1, Ismael Valverde1, Adrian Gallardo2*
1Department of Internal Medicine, Sanatorio Clínica Modelo de Morón
2Department of Critical Kinesiology, Sanatorio Clínica Modelo de Morón. https://orcid.org/0000-0002-9729-4839
*Corresponding Author: Adrian Gallardo, Department of Critical Kinesiology, Morón Model Clinical Sanatorium. https://orcid.org/0000-0002- 9729-4839.
Abstract
Inferior vena cava (IVC) abnormalities represent a rare type of congenital anomaly. In the case of agenesis, it is estimated that its frequency does not exceed 1 % in the general population. This condition can predispose to a pelvic congestion syndrome and produce symptoms (which are usually underestimated or attributed to other entities) such as chronic pelvic pain. Thus, in most cases, the anatomical alteration is discovered in imaging studies performed for other reasons.
We present here two clinical cases in order to highlight the importance of the differential diagnosis for IVC anomalies and to characterize the pelvic congestion syndrome, linking both entities. The prevalent symptoms (chronic pelvic pain) and hemodynamic changes led to other complications, already reported in the literature, such as deep vein thrombosis. The importance of correct differential diagnosis and timely treatment could significantly improve the clinical course of these patients.
Keywords: chronic pelvic pain, pelvic congestion syndrome, inferior vena cava agenesis, deep vein thrombosis
Introduction
The inferior vena cava (IVC) divides into 3 segments: prerenal, renal, and postrenal. Due to the complexity of the intrauterine vessel formation process, different anomalies can be observed. They are rare alterations with a frequency of 0.3 %-0.5 % in the healthy population, and 2 % in patients with cardiovascular disease [1]. This peculiarity generates abnormal venous drainage of the lower extremities, increasing the risk of deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE) [2].
Pelvic Congestion Syndrome (PCS), on the other hand, is an increasingly recognized entity. Complete absence of IVC is a rare cause of pelvic congestion syndrome [3-12]
In recent years, its diagnosis based on imaging studies has improved. In most cases, it involves a casual finding when performing these tests for reasons unrelated to the original [2]. Other less frequent presentations include sciatic neuropathy (compression of lumbar nerve roots); compressive symptoms in the form of obstructive pyelonephritis, pelvic congestion syndrome in women, and varicocele in men [4]
Considering its low frequency of appearance and the limited bibliographic evidence, we present two patients with PCS not diagnosed in time, which developed, over the years, to the complications mentioned in the literature, such as DVT.
The work was approved by the Bioethics Committee and the Institutional Teaching and Research Committee as it did not violate the rights or privacy of the patients, who gave their consent to share their data, preserving their identities.
Case 1
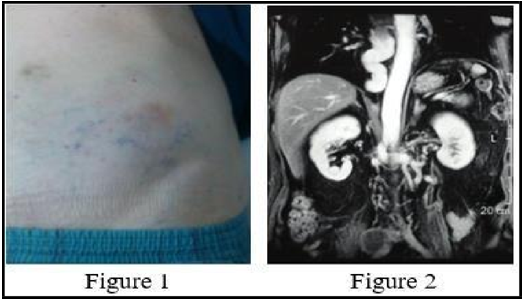
A 74-year-old male consulted for edema and pain in the lower limbs, with difficulty walking. On physical examination, he highlighted collateral venous circulation in the abdomen (Figure 1), with signs of chronic venous insufficiency of the lower limbs. The antecedents include: bilateral varicocele, chronic lower limb pain and concomitant pelvic pain. Suspecting DVT, a venous Doppler was performed, which confirmed extensive bilateral iliac-femoral DVT. In addition, an abdominopelvic angiotomography was performed, which showed the absence of an infrarenal IVC (Figure 2) with occlusion of both femoral and iliac veins and the caudal portion of the IVC, compatible with thrombosis.
Case 2
A 27-year-old woman presented with left groin pain and indurated erythema on the ipsilateral flank, manifesting difficulties in walking, pain and heaviness in the lower limbs and long-standing pelvic pain predominantly on the left. History of DVT in the left femoral vein at age 19, anticoagulated since then; thrombophilia studies, negative. No abortions. Doppler ultrasound showed left femoral DVT with collateral circulation to the abdominal wall. An angiotomography of the abdominopelvic vessels showed incomplete iliac veins, absence of the inferior vena cava, with significant pelvic collateral circulation, and tortuous veins in the left inguinal region with signs of thrombosis (Figure 3a). Venography confirmed the agenesis of the inferior vena cava with significant development of the paravertebral venous system, azygos and hemiazygos (Figure 3b), with visualization of a minimum remnant of 1cm of IVC entering the right atrium (Figure 4).
Discussion
The IVC is a large-caliber venous trunk that returns blood from the lower limbs, abdominal organs, infradiaphragmatic veins, and the pelvis to the right atrium and is the satellite vein of the abdominal aorta. IVC agenesis has an incidence of < 1 % in the general population [5], although incidences of 8.7 % have been reported [6] . Chronic pelvic pain is defined as noncyclic pelvic pain of more than 6 months' duration. It has a reported incidence of 24-39.1 % and leads to 10-40 % of gynecological visits [7]. Despite the high incidence, studies have shown that a large percentage of women (40-75 %) do not seek medical advice [8]. It is generally known as pelvic congestion syndrome (PCS), although it has also been called “Taylor syndrome”, “congestion-fibrosis syndrome”, “pelvic vein incompetence” or “female varicocele”. The definition of PCS was established in the Transatlantic Interdisciplinary Consensus Document VEIN-TERM [9], as “chronic symptoms that may include pelvic pain, perineal heaviness, urination urgency and postcoital pain, caused by reflux of ovarian veins and/or pelvic and/or obstruction, and which may be associated with vulvar, perineal and/or lower extremity varices”.
External compression (nutcracker syndrome, May-Thurner syndrome, retroperitoneal mass) may be associated with the development of PCS. However, the link with the agenesis of the inferior vena cava is a very rare condition.
Patients with IVC agenesis may present with symptoms of lower extremity venous insufficiency, idiopathic DVT, or PCS. Although patients with absent infrarenal IVC are generally asymptomatic, the most common clinical symptom is DVT [10], usually treated with anticoagulation.
Imaging findings alone are not diagnostic. Although venography is considered the gold standard, CT, MRI, or ultrasound is often used first for the diagnosis of PCS with findings of gonadal dilation and parametrial vessels. On CT, pelvic varices appear as dilated, tubular, enhancing parametrial structures. One of the proposed diagnostic criteria on CT is at least four ipsilateral pelvic varicosities measuring > 4mm in diameter or dilation of the ovarian vein > 8mm in diameter [11] . However, this is little used in daily clinical practice and the results are often subjectively described.
In addition to symptoms of chronic pelvic pain, PCS may also be associated with varicose veins of the lower extremities, either in a typical saphenous distribution, or in atypical locations including the vulva, perineum, and posterior thigh.
In our patients, as reported in the literature, the lack of research on the symptoms of chronic pelvic pain, and the low level of consultation related to this disease led to late diagnosis. Despite currently having non-invasive high-definition imaging studies that make it possible to highlight these anatomical anomalies. Based on the foregoing, it is reasonable to consider abdominal CT angiography or magnetic resonance angiography as screening techniques in young patients with DVT or PE and without risk factors, having ruled out the existence of hereditary thrombophilia, for a definitive diagnosis.
Conclusion
Cases of IVC agenesis are rare and present diagnostic challenges. Considering the relationship between PCS and IVC agenesis, the signs and symptoms described above should guide the questioning to arrive at the diagnosis of this pathology, investigating the manifestations of "collateral damage" that are presenting in the long-term evolution of this entity. Chronic pelvic pain is a common cause of morbidity in PCS, usually underdiagnosed. Although the findings on the images may be incidental, it is necessary to increase diagnostic suspicion to identify long-term complications early and provide effective and timely treatment.
Funding: The work did not receive any funding
Conflicts of interest: none to declare.
References
- Rizzardi JLA. Buscemi D. Schiavoni J. et al. Inferior vena cava agenesis. Scientific letter. 2016. RACCV.2016;14 (2): 70-73.
- Ramos Aranda J, Ramírez Cerda C, Cohen Mussali S, Valdés Flores J (2003) Inferior vena cava agenesis as a risk factor for pulmonary thromboembolism. AN. MID INTERNA. 2003 20:6: 304-306
- Menezes T, Haider EA, Al-Douri F, El-Khodary M, Al-Salmi I (2019) Pelvic congestion syndrome due to agenesis of the infrarenal inferior vena cava. JRCR. 14(1): 36–40.
- Satyendra NS, Trilock CB (2017) Inferior Vena Cava Agenesis: A Rare Cause of Pelvic Congestion Syndrome. JCDR. 11(3): TD06-TD08.
- Sneed D, Hamdallam I, Sardi A (2005) Absence of the Retrohepatic Inferior Vena Cava: What the Surgeon Should Know. Am Surg. 71(6): 502-504.
- Cho BC, Choi HJ, Kang SM, Chang J, Lee SM, et al. (2004) Congenital Absence of Inferior Vena Cava as a Rare Cause of Pulmonary Thromboembolism. Yonsei Med J. 45(5): 947-51.
- Kaufman C, Little NA (2021) Pelvic Congestion Syndrome: A Missed Opportunity. IJRI. 31(3): 539-544.
- Zondervan KT, Yudkin PL, Vessey MP, Jenkinson CP, Dawes MG, et al. (2001) The community prevalence of chronic pelvic pain in women and associated illness behaviour. BJGP. 51(468): 541-547.
- Eklof B, Perrin M, Delis KT, Rutherford RB, Gloviczki P (2009) Updated terminology of chronic venous disorders: the VEIN- TERM transatlantic interdisciplinary consensus document. J Vasc Surg. 49(2): 498–501.
- Chee YL, Culligan DJ, Watson HG (2001) Inferior vena cava malformation as a risk factor for deep venous thrombosis in the young. Br J Haematol. 114(4): 878-80.
- Coakley FV, Varghese SL, Hricak H (1999) CT and MRI of pelvic varices in women. J Comput Assist Tomography. 23(3): 429–434.
- Knuttinen MG, Xie K, Jani A, Palumbo A, Carrillo T, et al. (2015) Pelvic venous insufficiency: imaging diagnosis, treatment approaches, and therapeutic issues. AJR. 204(2): 448–458.