Collin Liu, MD, MS1 *, Alan Wang, MD1, William Thorell, MD1
1Department of Neurosurgery, University of Nebraska Medical Center. 988437 Nebraska Medical Center, Omaha, NE 68198, USA.
*Corresponding Author: Collin Liu, MD, MS, Department of Neurosurgery, University of Nebraska Medical Center. 988437 Nebraska Medical Center, Omaha, NE 68198, USA.
Abstract
Vertebral artery (VA) transection is a rare and uncommon presentation of traumatic injury. It is more commonly seen with penetrating neck injuries than with blunt cerebrovascular injuries (BCVI). Transection of VA secondary to BCVI is associated with 100% mortality in several case reports and series. In this case study, we present a 60-year-old female who sustained a fall downstairs resulting in a right C3 transverse process (TP) fracture and right VA transection. The patient had active exsanguination from both the right proximal VA through anterograde flow and the distal ipsilateral VA through retrograde filling from the contralateral VA leading to cervical hematoma. She underwent emergent sacrifice of VA via coil embolization of VA proximally as well as distally via retrograde access through the vertebrobasilar junction (VBJ). Post-operatively, the patient was neurologically intact with no imaging signs of posterior circulation stroke. We describe our technique of sacrificing proximal and distal VA as well as important factors affecting the outcome.
Keywords: Vertebral artery (VA), Blunt Cerebrovascular Injuries (BCVI), Vertebro-Basilar Junction (VBJ)
Introduction
Background and Importance
Blunt cerebrovascular injuries (BCVI) including non-penetrating injuries to the carotid and vertebral artery (VA) are rare and under-reported. The incidence of BCVI is estimated at 27 % while traumatic VA injury is estimated at 3 % to 19 % of all non-penetrating polytraumas [1,2]. VA blunt injuries resulting in transections are even rarer, at only 3 % of all BCVI [3].
In several series and case studies, transection of VA is universally fatal, typically involving high-speed injuries [3]. In a series of four patients, Maloney et al described patients that sustained Motor Vehicle Collision (MVC) or pedestrian versus automobile collisions resulting in VA transactions. These patients had numerous other severe traumatic injuries, hemodynamic instability, and poor neurologic status. All four patients expired. Patients who survive the injury have significant permanent neurologic deficits. Griffard and Bollig describe a 62-year-old female who presented after an MVC with a C5-6 distraction injury and right VA transaction requiring VA endovascular sacrifice as well as cervical decompression and instrumentation. She developed new bilateral cerebellar infarcts and spastic quadriplegia post-operatively [4].
In contrast, penetrating neck injuries involving the VA or carotid artery have an estimated incidence of 1 % to 7 % [6,7,8]. These patients appear to have better outcomes compared to patients with BCVI after successful endovascular deconstructive treatment of transected VAs proximally and distally by navigation through the VBJ [5,6,7].
Clinical Presentation
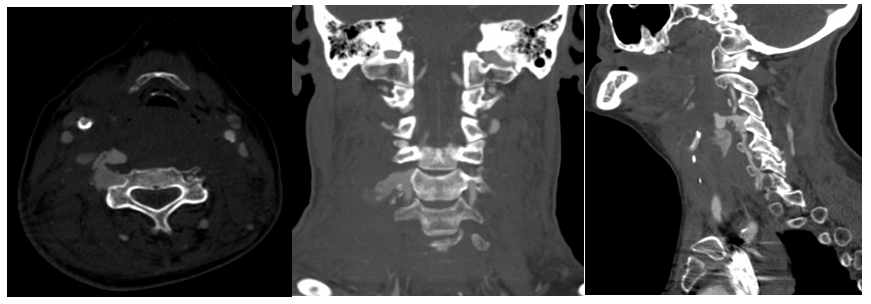
A 60-years-old female with a past medical history significant for atrial-fibrillation and mechanical mitral valve on warfarin presented after falling multiple stairs. She complained only of neck pain with no neurologic deficits. On exam, she had noticeable soft palpable enlargement over the anterior neck. CTA of the neck revealed a right C3 transverse process (TP) fracture and right VA dissection with contrast extravasation into the soft tissues (Figure 1).
Figure 1: CTA of the neck demonstrated right-sided C3 transverse process fracture with vertebral artery transection and contrast extravasation into the soft tissue. (axial image to the left, coronal image in the middle, sagittal image on the right).
After reviewing her head and neck CTA from the previous hospitalization, it was determined she had co-dominant VAs as well as a right fetal posterior communicating (PComm) artery supplying the right posterior cerebral artery (PCA) (Figure 2). After discussion with the patient and family, we proceeded with an emergent diagnostic angiogram (DSA) with the intent to reconstruct or deconstruct the right VA. Our Institutional Review Board was consulted and patient consent for this case report was not required as there are no patient identifiers.

Figure 2: Computer Tomography Angiogram of the head with three-dimensional reconstruction demonstrating right fetal posterior communicating artery and hypoplastic left posterior communicating artery.
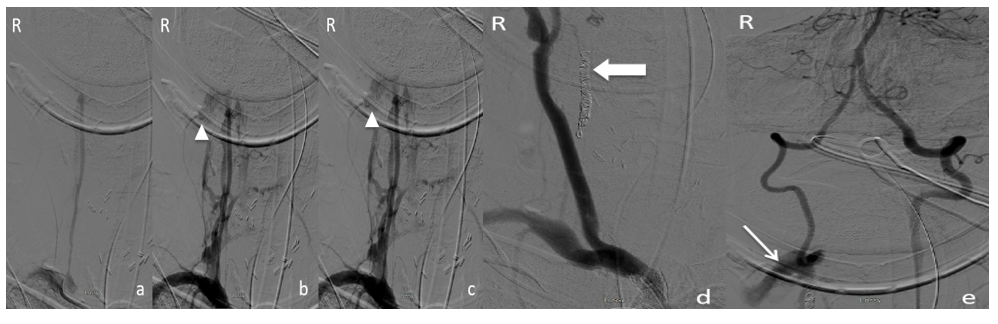
The femoral artery was accessed and 5F DAV® (Cook Medical, Bloomington, IN, USA) was navigated to the left common carotid artery (CCA), left VA, as well as the right CCA for a full DSA of head and neck. DSA of the right VA demonstrated contrast extravasation into the soft tissue at the level of the TP fracture (Figure 4 a,b,c). DAV® a catheter was then exchanged with a 5F-MPD Envoy® (DePuy Synthes/Codman Neuro, Raynham, MA, USA). We then used Synchro-2® (Stryker, Kalamazoo, MI, USA) wire and Excelsior® SL-10 catheter (Stryker, Kalamazoo, MI, USA) to navigate through the site of contrast extravasation traveling anterograde through the right VA to reconstruct or deconstruct it. However, the wire extruded out of the injured vessel into the soft tissues. An attempted super-selective road map was also unsuccessful as the contrast extravasated into the soft tissue without filling the distal VA. At this point, coils were utilized to occlude the proximal right VA (Figure 4d).
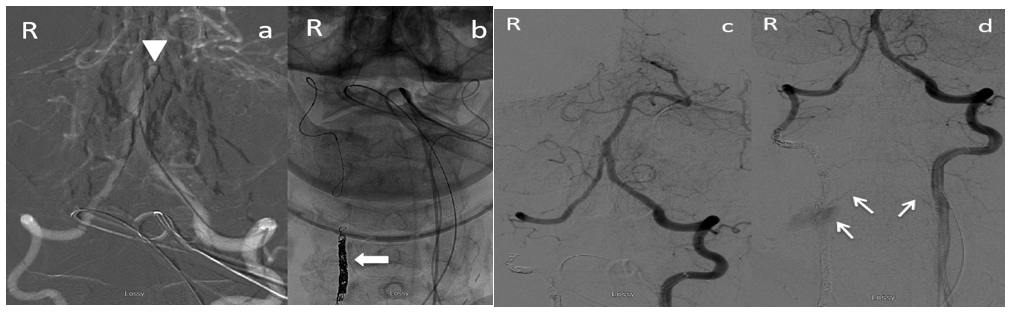
A subsequent left VA DSA revealed continued extravasation of contrast from retrograde flow into the right distal VA (Figure 4e). An initial attempt with an SL-10 catheter over Synchro®-2 microwire to navigate the vertebra-basilar junction (VBJ) to the contralateral VA was unsuccessful because of the tight turn. We subsequently switched to the Prowler® Select™ Plus (Codman Neurovascular) steamed-shaped into a tight “J” catheter tip and again were unsuccessful. We then placed an extensive shape at the tip of the Synchro® wire as illustrated in figure 3. Using a similar technique to shape Synchro® microwire into a double angle, we then positioned the distal catheter into the left PCA, which allowed us to successfully track the microwire down to the contralateral right VA inferior to the posterior-inferior cerebellar artery (PICA) and superior to the site of extravasation where several coils were subsequently deployed. Finishing runs did not reveal any contrast filling from the injured VA with the exception of minimal blush from the muscular branch of the left VA (Figure 5).
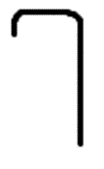
Figure 3: Shape placed on the Synchro® wire and the Prowler® Select™ Plus catheter to assist in navigating the vertebrobasilar junction to access the contralateral vertebral artery
Figure 4: Digital Subtraction Angiograms of the head and neck Anterior-Posterior views. (a-c) Contrast injection into the right vertebral artery illustrated at early (a), middle (b), and late (c) timing demonstrating contrast extravasation and no flow to the right vertebral artery distal to the transaction. Contrast extravasation is illustrated by a triangle. d) The contrast was then injected into the right innominate artery post-coiling to evaluate for occlusion of the right vertebral artery. The right common carotid artery can be seen. Large block arrow points to the coil mass in the proximal right vertebral artery without contrast extravasation into soft tissue. e) Contralateral left vertebral artery contrast injection demonstrating retrograde flow through the right vertebral artery and contrast extravasation into soft tissue as shown by the thin arrow
Figure 5: digital subtraction angiograms of the vertebrobasilar system anterior-posterior view a) demonstrates utilizing the Prowler® Select™ Plus with the Synchro® microwire navigating the acute angle of the vertebrobasilar junction to access the contralateral right vertebral artery as shown by the triangle b) coiling of the distal right vertebral artery. The Block arrow shows the coil mass. (c-d) contralateral left vertebral artery contrast injection post-coiling to evaluate for occlusion. A small muscular branch from the left VA transversely crossed midline into the area of the previous extravasation with minimal blush emphasized with arrows.
Post-operatively, the patient remained intubated until post-operative day four after her neck swelling resolved. MRI/MRA after the procedure did not reveal any diffusion restriction or stroke in the posterior circulation (Figure 6). The patient was neurologically intact and discharged with a cervical collar. On her 2 monthly clinic follow-up, she remained neurologically intact with no residual or recurrent pseudoaneurysm flow or arteriovenous fistula (Figure 7).

Figure 6: Post-operative imaging of right vertebral artery transection endovascular coiling. a) Diffusion-weighted imaging Magnetic Resonance Imaging of the brain without evidence of post-operative posterior circulation stroke. b) apparent diffusion coefficient Magnetic Resonance Imaging of the brain without evidence of post-operative posterior circulation stroke. c) Magnetic Resonance angiogram of the neck demonstrating post-operative successful occlusion of the right vertebral artery injury without contrast extravasation into the soft neck tissue.
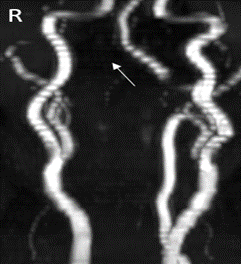
Figure 7: 2 month follow up MRA without evidence of pseudoaneurysm or arteriovenous fistula
Conclusion
Vertebral artery injuries are rare and account for 2.4-6.1 % of all arterial injuries and 7.1 %-19.4 % of cranial-cervical arterial injuries [6]. Trauma to the VA can lead to dissection, pseudoaneurysm, transection, arteriovenous fistula, mural hematoma, and occlusion [6]. Transection of the VA is associated with high mortality and morbidity. The clinical outcome can range from asymptomatic to vertebrobasilar insufficiency, posterior circulation infarct, and death [3]. Treatment of transected VA is difficult because of the deep-seated location in the neck for surgical exposure and access for ligation. Alternative therapies largely involve endovascular approaches including covered stent for reconstruction and embolization for occlusion.
In our case, a covered stent was considered but not possible as we were unsuccessful in traversing across the transection to deploy a stent. The patient was neurologically intact post-operatively likely because she had co-dominant VAs. In addition, we were able to preserve perfusion through the PICA ipsilateral to the right VA injury by confirming we were inferior to the PICA prior to coiling the distal right VA. There was no competing forward flow in the distal V4 segment of the right VA so the retrograde flow from the contralateral VA provided adequate perfusion as demonstrated by the absence of cerebellar infarcts post-operatively. Other factors that lead to a good outcome despite her multiple medical co-morbidities include: 1) no neurologic deficits pre-procedure; 2) no spinal cord injury or other injuries; 3) right fetal PComm circulation decreasing her dependence on the vertebrobasilar system to supply the PCA distribution.
References
- Lee YJ, Ahn JY, Han IB, Chung YS, Hong CK, et al. (2007) Therapeutic endovascular treatments for traumatic vertebral artery injuries. Journal of Trauma and Acute Care Surgery. 62(4): 886-891.
- Biffl WL, Moore EE, Offner PJ, Burch JM (2001) Blunt carotid and vertebral arterial injuries. World journal of surgery. 25(8): 1036-43.
- Maloney E, Lehnert B, McNeeley MF (2015) Vertebral artery transection in nonpenetrating trauma: a series of 4 patients. Annals of Vascular Surgery. 29(7): 1450-e11.
- Griffard J, Bollig R (2020) Right Vertebral Artery Transection with a Vertical Distraction of C5-6: Case Report of a Patient Survival. American Surgeon. 86(5): 531-533.
- Sofoluke N, Shimony N, Goren O (2020) Endovascular Treatment of Traumatic Transection of the Vertebral Artery Caused by Penetrating Injury to the Oropharynx in a Pediatric Patient. World Neurosurgery. 137: 389-392.
- Yevich SM, Lee SR, Scott BG, Shaltoni HM, Mawad ME, et al. (2014) Emergency endovascular management of penetrating gunshot injuries to the arteries in the face and neck: a case series and review of the literature. J Neurointerv Surg. 6(1): 42-46.
- Cohen JE, Rajz G, Itshayek E, Umansky F, Gomori, JM (2005) Endovascular management of exsanguinating vertebral artery transection. Surgical Neurology. 64(4): 331–334.
- de Castro SM, Christiaans SC, van den Berg R, Schep NW (2014) Minimal invasive management of traumatic transection of the vertebral artery. Springerplus. 3(1): 206.