Ahmad Farshad Ghaznawi1, Makai Sadaat2, Mahmood Shah Rahimi3, Zahir Shah Khan Quraishi4, Sayed Tariq Pachakhan5*, Mohammad Mustafa Ludin6
¹National Disease Surveillance and Response Officer (NDSR) - WHO focal point at Balkh Regional Reference Laboratory, Mazar-E-Sharif Afghanistan. University of Peshawar (UoP), Department of Biotechnology, Peshawar, Pakistan. ORCID: 0000-0001-8802-5912
2Head of Clinical Pathology, Human Medical Laboratories and Research Center Kabul, Afghanistan. Kabul Medical University (KMU) Department of Medical Laboratory Technology (MLT), Kabul, Afghanistan. ORCID: 0000-0003-2466-0487
3Chief Executive Officer, Human Medical Laboratories (HML), Senior Microbiologist Central Public Health Laboratories (CPHL), Kabul, Afghanistan. ORCID: 0009-0001-0877-7397
⁴Specialist of Children and Newborn Care, Department of Pediatric Medicine, Shah Amanullah Ghazi Hospital, Kabul, Afghanistan. ORCID: 0009-0005-9788-0837
5Immune Infectious Disease Supervisor with World Health Organization at Central Public Health Laboratory (CPHL), Kabul, Afghanistan ORICD: orcid.org/0000-0002-9010-721X
6Senior Medical Laboratory Technologist and Specialist of Microbiology & Chromatography Testing in FDA Quality Control Laboratories, Kabul, Afghanistan. Afghan International Islamic University (AIIU) Department of MSc Medical Laboratory Technology (MLT), Kabul, Afghanistan. ORCID: 0009-0009-1669-8574
*Corresponding Author: Sayed Tariq Pachakhan, Immune Infectious Disease Supervisor with World Health Organization at Central Public Health Laboratory (CPHL), Kabul, Afghanistan ORICD: orcid.org/0000-0002-9010-721X
Abstract
Background/Aims: Celiac disease (CD) is an autoimmune disease triggered by gluten ingestion, leading to small intestine inflammation and villous atrophy. The estimated pooled global seroprevalence of celiac disease (CD) is 1.4%, with women being more affected than men. This study aimed to assess the prevalence of celiac disease (CD) among the Afghan population.
Methods: This was a cross-sectional study aimed to assess the prevalence of celiac disease (CD) in patients referred to the Human Medical Laboratory for a tissue transglutaminase antibody test. Five hundred and eighteen patients of different ages were studied for celiac disease (CD) using the ELISA method.
Results: 518 cases were studied. 327 were male and 191 were female. 191 were positive, of which 103 were male, 88 were female, 173 were children, and 18 were adults.
Conclusions: In Afghanistan, celiac disease (CD) is more common in women than in men, and it affects children more often than adults. These findings emphasize the need for awareness, screening, and tailored diagnostic guidelines for the Afghan population.
Keywords: Gluten enteropathy; Intestines, small; Tissue-Type Transglutaminase
Introduction
Celiac disease (CD) is a chronic immune-mediated disorder characterized by inflammation of the small intestine, villous atrophy and crypt hyperplasia. It is brought on by dietary gluten consumption in those with a genetic predisposition, which damages the mucosa in the small intestine and encourages malabsorption. Cereals including wheat, rye, barley, spelt, and kamut contain the protein gluten.[1] Patients with type 1 diabetes, autoimmune thyroiditis, Down's syndrome, Turner's syndrome, and William's syndrome, first-degree relatives of CD patients are among the high-risk groups.[2] Also included are bearers of the HLA-DQ2 and –DQ8 alleles.[3] Frequent signs and symptoms of CD include diarrhea, weight loss, and abdominal distention.[4] Other manifestations are anemia, bloating, and irregular bowel habits.[5] Less common symptoms include infertility,[6] migraines,[7] neuropsychiatric symptoms,[8] and abnormal liver enzyme levels.[9] The untreated disease can get complicated and lead to dermatitis herpetiformis,[10] gluten ataxia,[11] celiac crisis,[12] osteoporosis,[13] enteropathy-associated T cell lymphoma, and adenocarcinoma of the jejunum.[14]
The first-line test for the diagnosis of CD is the detection of IgA anti- tissue transglutaminase antibodies [15] because of its high specificity (97%) and sensitivity (94%), especially in people who do not have IgA deficiency. [16] In IgA-deficient individuals, the detection of IgG anti-tissue transglutaminase antibodies is beneficial. [12] However, IgG-deamidated gliadin peptide antibodies, which have higher sensitivity and specificity than IgG anti-tissue transglutaminase antibodies, are a valid test for identifying CD in IgA-deficient patients. [17] A confirming test for the diagnosis of an active CD is the IgA anti-endomysial antibody (EMA) test. [18] A small intestine biopsy is necessary for the confirmation of serologic tests for CD;4 however, it is not advised for children with typical symptoms, HLA genotypes, or high anti-tissue transglutamiase antibody titers. [18] Initial research on the prevalence of CD in the general population was done in European nations.[19] Subsequently, CD prevalence was reported in Caucasian-majority nations such as North and South America and Australia. [20–22] There have recently been numerous reports of CD prevalence in non-Caucasian populations, including Asia and Africa as well. [23,24]
The pooled global seroprevalence of CD is 1.4% (95% CI, 1.1-1.7%) [25] and the biopsy-confirmed CD global prevalence is 0.7% (95% CI, 0.5-0.9%). [26] In Asian countries, the pooled prevalence of CD based on IgA anti-tissue transglutaminase antibodies and/or anti- endomysial antibodies (EMA) is 1.6%, and based on biopsy, the prevalence of CD is 0.5%. [27] Neighboring countries to Afghanistan such as Pakistan, [28] Iran, [29] and China [28] have reported cases of CD. Although practically all families in Afghanistan consume wheat as their primary food, [30] there is no data on the prevalence or incidence of CD in the country. The objective of our study is to assess the prevalence of CD in the general population of Afghanistan.
Methods
1. Study
Our study, which was done on 467 patients referred to the Human Medical Laboratory between the beginning of January 2020 and March 2023, is the first descriptive cross-sectional study of its kind in Afghanistan to estimate the prevalence of CD. The patients were from various provinces of Afghanistan, including Kabul, Khost, Bamyan, Nangarhar, Ghazni, Logar, and Mazar-E-Sharif. The inclusion of patients from diverse regions across Afghanistan ensures a more representative sample of the country's population, reflecting potential regional variations in celiac disease prevalence. Demographic characteristics of the patients including name, sex, and age were collected in the database of the laboratory. This study included patients who had tTG IgA and IgG tests recommended by the referring clinicians, along with signs and symptoms of CD, including persistent diarrhea, bloating, abdominal distension, irregular bowel habits, malabsorption, weight loss, and iron deficiency anemia. Patients who did not meet the requirements for a tTG IgA and IgG test and who displayed symptoms unrelated to CD were excluded. Three mL blood sample was needed. Each sample was centrifuged immediately after collection and the separated serum was stored at 2- 8oC. TestLine® EIA Transglutaminase IgA and IgG was used to test the samples for tTG IgA and/or IgG by the ELISA method. The kits were produced in the Czech Republic by TestLine Clinical Diagnostics s.r.o., and the protocols were followed exactly as instructed. According to the manufacturer's instructions, the test results were categorized as negative (18 U/ml), borderline (18-22 U/ml), and positive (>22U/ml).
2. Statistical Analysis: The data was analyzed using IBM® SPSS® Statistics version 22. Mann-whitney and Chi-Squared tests were used to find out any relationship between the variables.
Results
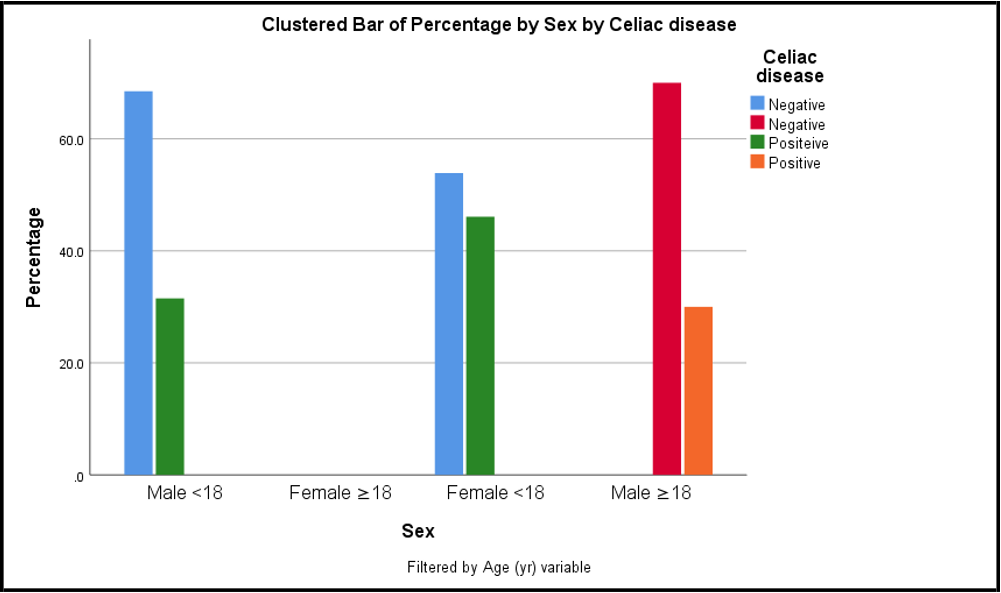
Of the 518 cases studied, 327 were male, 191 were female, 485 were children, 60 were adults, 191 were positive, and 327 were negative (Table 1) (Figure 1).
Table 1: Frequency of Different Variables
|
Variable |
Frequency |
|
|
Age (yr) |
<18 |
485 |
|
≥18 |
60 |
|
|
Sex |
Male |
327 |
|
Female |
191 |
|
|
Celiac disease |
Positive |
191 |
|
Negative |
327 |
|
Figure 1: Clustered Bar Chart Showing the Percentage of Celiac Disease Cases by Sex and Age Group.
Among positive cases, 103 were male, 88 were female, 173 were children (<18 years), and 18 were adults (≥18 years). Females are more affected than males. The Chi-squared test result also indicates a significant difference between the occurrence of CD and the female sex (p=0.001). In addition, the Mann-Whitney test showed no significant difference between CD and the two age groups (p=0.282) (Table 2).
Table 2: Results of the Chi Squared Test and Mann-Whitney Test
|
Celiac disease |
|
Positive (N,%) |
Negative (N,%) |
Total (N,%) |
P-value |
|
Sex |
Male |
103 (31.5) |
224 (68.5) |
327 (100) |
0.001(F)a |
|
Female |
88 (46.1) |
103 (53.9) |
191 (100) |
||
|
Age (yr) |
<18 |
173 (37.8) |
285 (62.2) |
458 (100) |
0.282b |
|
≥18 |
18 (30.0) |
42 (70.0) |
60 (100) |
a P<0.05.
b P>0.05.
F, Fisher’s exact test.
The IgA anti-tissue transglutaminase (tTG IgA) alone was positive in 47.1% of cases. Similarly, 47.1% of cases were positive for both IgA and IgG antibodies, and 5.8% were positive for IgG anti-tissue transglutaminase (tTG IgG) only (Table 3). There was no borderline result.
Table 3: Percentage of Positive and Negative tTG IgA and tTG IgG Antibodies
|
Tissue transglutaminase antibodies (tTG) |
Celiac disease |
Total (N,%) |
|
|
Positive (N,%) |
Negative (N,%) |
||
|
tTG IgA |
90 (47.1) |
71 (21.7) |
161 (31.1) |
|
tTG IgG |
11 (5.8) |
1 (0.3) |
12 (2.3) |
|
tTG IgA+tTG IgG |
90 (47.1) |
255 (63.1) |
345 (66.6) |
IgA: immunoglobulin A, IgG: immunoglobulin G
According to the sample size of our study, the seroprevalence of CD was found to be 36.8% (95% CI, 0.32-0.41%). The demographic characteristics and statistical analysis results are summarized in Tables 1, 2, and 3.
Discussion
In a study including 2277 in-patients with gastrointestinal symptoms in Xinjiang Uyghur Autonomous Region of China, the seroprevalence was found to be 1.27% (95% CI, 0.81-1.73%). [31] In a relatively small study including 562 young healthy volunteers from Malaysia, a seroprevalence of CD was found to be 1.25% (95% CI, 0.78-1.72%). [32] Another study including 1961 Vietnamese children showed that 1.0% of them had anti-tTG antibodies. [33] In a multicenter pan-India study including 23 331 healthy adults the age adjusted seroprevalence of CD was 1.23% in Northern India, 0.87% in North-eastern India, and 0.10% in Southern India. [22] In our study, the prevalence of celiac disease was higher in Afghanistan than in neighboring countries. The reason is that the population studied was not selected among the healthy population, as in other studies, and only those subjects were included who were unhealthy and suspected of having celiac disease.
The prevalence of CD is 1.5 to 2 times greater in women compared to men with a female-to-male ratio ranging from 2:1 to 3:1.12 In addition, a systematic review and meta-analysis found that seropositivity among male participants in screening studies was slightly lower than in females, [34] although some studies of adults indicate that men and women have similar seroprevalences.[35,36] Results from all the studies conducted earlier have revealed that there is no statistically significant difference between age and CD. Thus, the disease can develop at any age. [37,38] The prevalence of CD in individuals younger than 60 years is 1.8%, and in individuals 60 years and older, it is 1.0%. [39] Additionally, recent prospective cohort studies have suggested that the majority of patients develop CD in their first decade of life. [40] Despite the higher prevalence of CD in younger age groups, meta-regression was not able to find any relationship between the prevalence of CD and age.[39]
In our study, 161 cases were referred to for tTG IgA testing only, of which 90 had positive results and 71 had negative results. This may have an impact on our nation’s actual CD prevalence because celiac- positive patients with IgA deficiency may not have been diagnosed. Additional factors affecting the results of the current study include the lack of biopsy confirmation of the serologically positive cases or other serological confirmatory tests, the absence of appropriate guidelines for the diagnosis of CD in Afghanistan, and most doctor’s unawareness of the disease, which results in many patients going undiagnosed. Furthermore, the serologic kits that were used in our study to find tTG antibodies were produced in Europe. As a result, their diagnostic precision was assessed for Caucasian groups, and the cut-offs for the antibody levels were established for those populations. Consequently, those cut offs established for that demographic may not apply to the Afghan population.
In conclusion, the results of our study are supported by the findings of earlier research. With a prevalence of 36.8%, CD affects the Afghan population. It affects women more than men and children more than adults. Research should be done in the future on the assessment of CD prevalence based on biopsy.
Declaration
Data Availability Statement: The raw data supporting the conclusions of this article will be made available by the authors, on reasonable request to the corresponding author.
Competing Interests: All authors declared no potential personal or financial conflicts of interest.
Ethics Statement: This study was ethically approved by the medical bioethics committee of the Human Medical Laboratory HML ethics committee (HML-ERC-23-002). The patients/participants provided their written informed consent to participate in this study.
Consent To Participate: This confirms that all human participants in the study agreed to be part of the research.
Consent For Publication: This ensures participants agreed to have their data published.
Author Contributions:
A. F. Ghaznawi (First Author)1: Data curation, Formal analysis, Validation (serological testing protocols), Manuscript review and writing.
M. M. Ludin2: Conceptualization (study design), Formal analysis, writing original draft, supervision of laboratory quality control.
M. S. Rahimi3: Supervision, Project coordination, Funding acquisition (HML research support).
Z. S. K. Quraishi4: Validation, Clinical interpretation, Review & editing (clinical implications), Patient referral for testing.
S. T. Pachakhan5: Citation/references review, Manuscript preparation for publication.
M. Sadaat6: Data collection, Patient sample management, Formal analysis, Investigation (clinical pathology oversight), Statistical analysis (SPSS).
All authors approved the final manuscript and agreed to be accountable for all aspects of the work.
Funding: This study was financially supported by HML.
Data Availability Statement
The data used to support the findings of this study are included within the article.
References
- Andrén Aronsson C, Lee HS, Hård Af Segerstad EM, Uusitalo U, Yang J, et al. (2019) Association of Gluten Intake During the First 5 Years of Life With Incidence of Celiac Disease Autoimmunity and Celiac Disease Among Children at Increased Risk. JAMA - J Am Med Assoc. 322(6): 514-523.
- Caio G, Volta U, Sapone A, Leffler DA, De Giorgio R, et al. (2019) Celiac disease: a comprehensive current review. BMC Med. 17(1): 142.
- Castillo NE, Vanga RR, Theethira TG, Rubio-Tapia A, Murray JA, et al. (2015) Prevalence of abnormal liver function tests in celiac disease and the effect of a gluten-free diet in the US population. Am J Gastroenterol. 110(8): 1216-1222.
- Catassi C, Rätsch IM, Fabiani E, Rossini M, Bordicchia F, et al. (1994) Coeliac disease in the year 2000: exploring the iceberg. Lancet. 343(8891): 200-203.
- Choi JM, Lebwohl B, Wang J, Lee SK, Murray JA, et al. (2011) Increased prevalence of celiac disease in patients with unexplained infertility in the United States. J Reprod Med. 56(5- 6): 199-203.
- Choung RS, Ditah IC, Nadeau AM, Rubio-Tapia A, Marietta EV, et al. (2015) Trends and racial/ethnic disparities in gluten- sensitive problems in the United States: findings from the National Health and Nutrition Examination Surveys from 1988 to 2012. Am J Gastroenterol. 110(3): 455-461.
- Dreisigacker S, Sharma RK, Huttner E, Karimov A, Obaidi MQ, et al. (2019) Tracking the adoption of bread wheat varieties in Afghanistan using DNA fingerprinting. BMC Genomics. 20(1): 660.
- Fasano A (2003) Celiac disease--how to handle a clinical chameleon. N Engl J Med. 348(25): 2568-2570.
- Fasano A, Berti I, Gerarduzzi T, Not T, Colletti RB, et al. (2003) Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 163(3): 286-292.
- Fasano A, Cellier C (2012) Clinical practice. Celiac disease. N Engl J Med. 367(25): 2419-2426.
- Green PH, Cellier C (2007) Celiac disease. N Engl J Med. 357(17): 1731-1743.
- Hadjivassiliou M, Sanders DS, Woodroofe N, Williamson C GR (2008) Gluten ataxia. Cerebellum. 7(3): 494-498.
- Hill ID, Dirks MH, Liptak GS, Colletti RB, Fasano A, et al. (2005) Guideline for the diagnosis and treatment of celiac disease in children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 40(1): 1-19.
- Hovell CJ, Collett JA, Vautier G, Cheng AJ, Sutanto E, et al. (2001) High prevalence of coeliac disease in a population-based study from Western Australia: a case for screening? Med J Aust. 175(5): 147-150.
- Husby S, Koletzko S, Korponay-Szabó IR, Mearin ML, Phillips A, et al. (2012) European Society for Pediatric Gastroenterology, Hepatology and Nutrition. European society for pediatric gastroenterology, hepatology, and nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr. 54(1): 136-160.
- Jansson-Knodell CL, Hujoel IA, West CP, Taneja V, Prokop LJ, et al. (2019) Sex Difference in Celiac Disease in Undiagnosed Populations: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 17(10): 1954-1968.
- Katz KD, Rashtak S, Lahr BD, Melton LJ 3rd, Krause PK, et al. (2011) Screening for celiac disease in a North American population: sequential serology and gastrointestinal symptoms. Am J Gastroenterol. 106(7): 1333-1339.
- Laszkowska M, Mahadev S, Sundström J, Lebwohl B, Green PHR, et al. (2018) Systematic review with meta-analysis: the prevalence of coeliac disease in patients with osteoporosis. Aliment Pharmacol Ther. 48(6): 590-597.
- Lebwohl B, Roy A, Alaedini A, Green PHR, Ludvigsson JF (2016) Risk of Headache-Related Healthcare Visits in Patients With Celiac Disease: A Population-Based Observational Study. Headache. 56(5): 849-858.
- Lebwohl B, Rubio-Tapia A (2021) Epidemiology, Presentation, and Diagnosis of Celiac Disease. Gastroenterology. 160(1): 63- 75.
- Ludvigsson JF, Michaelsson K, Ekbom A, Montgomery SM (2007) Coeliac disease and the risk of fractures - a general population-based cohort study. Aliment Pharmacol Ther. 25(3): 273-285.
- Makharia GK, Verma AK, Amarchand R, Bhatnagar S, Das P, et al. (2011) Prevalence of celiac disease in the northern part of India: a community based study. J Gastroenterol Hepatol. 26(5): 894-900.
- Mohta S, Rajput MS, Ahuja V, Makharia GK (2021) Emergence of Celiac disease and Gluten-related disorders in Asia. J Neurogastroenterol Motil. 27(3): 337-346.
- Mohindra S, Yachha SK, Srivastava A, Krishnani N, Aggarwal R, et al. (2001) Coeliac disease in Indian children: assessment of clinical, nutritional and pathologic characteristics. J Heal Popul Nutr. 19(3): 204-208.
- Ramakrishna BS, Makharia GK, Chetri K, Dutta S, Mathur P, et al. (2016) Prevalence of Adult Celiac Disease in India: Regional Variations and Associations. Am J Gastroenterol. 111(1): 115- 123.
- Rubio-Tapia A, Kyle RA, Kaplan EL, Johnson DR, Page W, et al. (2009) Increased prevalence and mortality in undiagnosed celiac disease. Gastroenterology. 137(1): 88-93.
- Saberi-Firouzi M, Omrani GR, Nejabat M, Mehrabani D, Khademolhosseini F (2008) Prevalence of celiac disease in Shiraz, southern Iran. Saudi J Gastroenterol. 14(3): 135-138.
- Shamir R, Lerner A, Shinar E, Lahat N, Sobel E, et al. (2002) The use of a single serological marker underestimates the prevalence of celiac disease in Israel: a study of blood donors. Am J Gastroenterol. 97(10): 2589-2594.
- Sharaiha RZ, Lebwohl B, Reimers L, Bhagat G, Green PH, et al. (2012) Increasing incidence of enteropathy-associated T-cell lymphoma in the United States. Cancer. 118(15): 3786-3792.
- Singh P, Arora A, Strand TA, Leffler DA, Catassi C, et al. (2018) Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 16(6): 823-836.
- Singh P, Arora S, Singh A, Strand TA, Makharia GK (2016) Prevalence of celiac disease in Asia: A systematic review and meta-analysis. J Gastroenterol Hepatol. 31(6): 1095-1101.
- Sollid LM, Thorsby E (1994) HLA susceptibility genes in celiac disease: genetic mapping and role in pathogenesis. Gastroenterology. 106(4): 1133.
- Tonutti E, Visentini D, Picierno A, Bizzaro N, Villalta D, et al. (2009) Diagnostic efficacy of the ELISA test for the detection of deamidated anti-gliadin peptide antibodies in the diagnosis and monitoring of celiac disease. J Clin Lab Anal. 23(3): 165-171.
- van der Windt DA, Jellema P, Mulder CJ, Kneepkens CM, van der HH (2010) Diagnostic testing for celiac disease among patients with abdominal symptoms: a systematic review. JAMA. 303(17): 1738-1746.
- Volta U, Tovoli F, Caio G (2011) Clinical and immunological features of celiac disease in patients with Type 1 diabetes mellitus. Expert Rev Gastroenterol Hepatol. 5(4): 479-487.
- Yap TW, Chan WK, Leow AH, Azmi AN, Loke MF, et al. (2015) Prevalence of serum celiac antibodies in a multiracial Asian population--a first study in the young Asian adult population of Malaysia. PLoS One. 10(3): e0121908.
- Zanella S, De Leo L, Nguyen-Ngoc-Quynh L, Nguyen-Duy B, Not T, et al. (2016) Cross-sectional study of coeliac autoimmunity in a population of Vietnamese children. BMJ Open. 6(6): e011173.
- Zhou C, Gao F, Gao J, Yuan J, Lu J, et al. (2020) Prevalence of coeliac disease in Northwest China: heterogeneity across Northern Silk road ethnic populations. Aliment Pharmacol Ther. 51(11): 1116-1129.
- Zingone F, Swift GL, Card TR, Sanders DS, Ludvigsson JF, et al. (2015) Psychological morbidity of celiac disease: A review of the literature. United Eur Gastroenterol J. 3(2): 136-145.
- Zintzaras E, Germenis AE (2006) Performance of antibodies against tissue transglutaminase for the diagnosis of celiac disease: meta-analysis. Clin Vaccine Immunol. 13(2): 187-192.