Prabhu B1*, Venkatesh Gupta S K1, Anvith Shetty2, Gurudarshan R2
1Professor, Department of Orthopaedics, JJM Medical College, Davanagere, Karnataka, India
2Resident, Department of Orthopaedics, JJM Medical College, Davanagere, Karnataka, India
*Corresponding Author: Prabhu B, Professor, Department of Orthopaedics, JJM Medical College, Davanagere, Karnataka, India
Abstract
Introduction
Melorheostosis is a rare, non-genetic, non-developmental, sclerosing developmental dysplasia of bone and adjacent soft tissue. The characteristic radiographic appearance is that of candle wax dripping. Diagnosis is usually based on classical radiographic appearance rather than a clinical picture.
Case report
A 26-year-old female with dull aching pain over upper third left leg and knee with limitation in movements and associated swelling. On examination tenderness and limitation of movements were present. The plain radiograph showed extensive, dense, undulating, or irregular cortical hyperostosis, resembling candle wax dripping along the length of the left tibia suggestive of Melorheostosis and MRI showed features of Osteopathic striata of the left femur and Osteopoikilosis of the left hip joint. Inj. Zolindronic acid given. Physiotherapy was started to avoid contractures.
Conclusion:
Lab investigations in Melorheostosis are usually normal. The exact pathophysiology of the disease remains uncertain. No curative treatment options are available. Bisphosphonates, Denosumab, and physiotherapy are the available options for treatment.
Keywords: Melorheostosis; Leri disease; Osteopathic striata.
Introduction
Melorheostosis is a rare, nonhereditary sclerosing bone dysplasia first described in 1922 by Leri and Joanny [1]. The minimal prevalence has been estimated to be 0.9 per million [2]. It got this name because of the characteristic periosteal hyperostosis along the cortex of long bones which looks similar to the flowing or dripping of candle wax (originated from Greek, Melos = limb, Rhein = to flow, ostos = bone) [3-5]. Melorheostosis is also known by other synonyms such as candle disease of the bone, and osteosis eburnisans monomeric [6,7]. This condition may affect only one bone (monostotic form), one limb (monomeric form), or multiple bones (polyostotic form). Establishing the diagnosis in Melorheostosis is challenging. It is primarily based on radiological findings as defined by Frey Schmidt [8] and on the exclusion of other sclerosing bone diseases. It is a chronic progressive disorder and affects females and males equally [8]
Case report
A 26-year-old female came with complaints of dull aching pain over the left upper third leg and knee, which was insidious in onset, which has gradually increased and associated with swelling over the left leg since past 2 years and came to our OPD. She has consulted with orthopaedics from multiple hospitals, where radiographs were taken, and further MRI had been suggested. The patient was given analgesics and was advised physiotherapy and she does not give any relevant history of trauma to the affected limb in the recent past or before the pain started 2 years ago.
On physical examination, the swelling was tender on palpation and bony hard in consistency with an irregular surface.
Further, there was limited flexion of around 100 degrees at the left knee joint with no limitation in extension (figure 1.1 and figure 1.2) which was associated with pain.
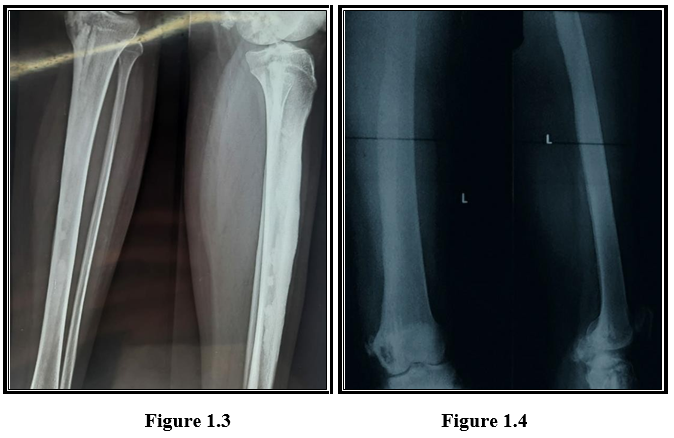
A plain radiograph of the left femur and tibia (figure 1.3 and figure 1.4) revealed an extensive, dense, undulating, or irregular cortical hyperostosis, resembling candle wax dripping, extending along the length of bone, resulting in deformity of the bone and narrowing of the medullary cavities.
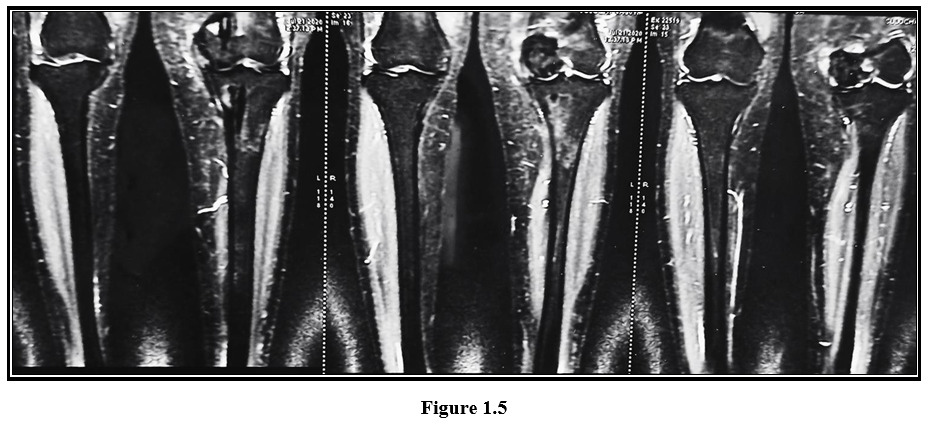
Laboratory investigations such as CBC, ESR, CRP, Serum Calcium, Serum phosphorous, Alkaline phosphatase were within normal limits Further MRI of the left lower limb showed flowing irregular cortical thickening of 2cm thickness along the medial aspect of the entire femur and along the medial and anterior aspect of the entire tibia (sparing distal tibial epiphysis) with thick undulating ridges of bone giving a flowing candle wax appearance (figure 1.5) suggestive of Melorheostosis.
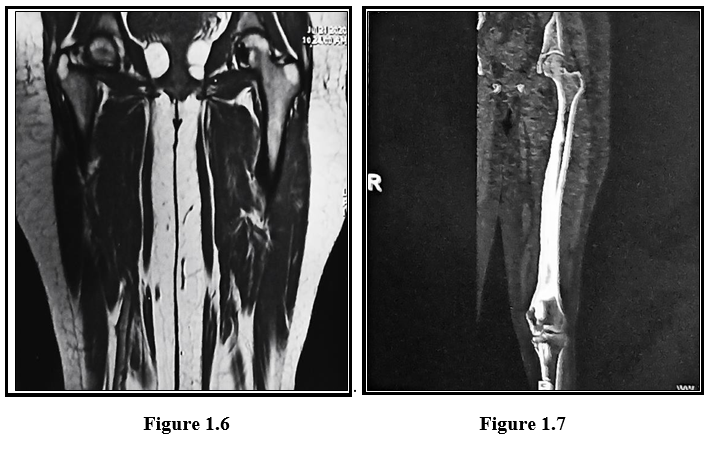
Few linear vertical dense striations saw an oriented parallel to the long axis of femur predominantly involving lower metaphysis giving a celery stalk metaphysis appearance suggestive of Osteopathic Striata (figure 1.7) Multiple enostoses/ bone islands clustered around the hip joint seen suggestive of Osteopoikilosis (figure 1.6)
Treatment included daily analgesics and bisphosphonates- Zoledronic acid 5mg, and daily physiotherapy to avoid soft tissue contractures. The patient reported alleviation of pain and was advised to continue physiotherapy to avoid the development of any deformities.
Discussion
Melorheostosis is a rare mesenchymal disease affecting the skeleton and adjacent soft tissue. It is a type of sclerosing bone dysplasia.
The exact etiology of the disease is unknown but the literature suggests that loss of function mutation of cell adhesion molecules coded by LEMD3 gene, a protein involved in bone morphogenic protein and tumour growth factor-β signalling may be the cause of melorheostosis and other diseases like Osteopoikilosis and Buschke Olendorff syndrome. [9]
Another possible etiology is altered expression of several adhesion proteins may contribute to the development of hyperostosis and concomitant soft tissue abnormalities of melorheostosis, with Beta- IGH3, in particular, playing an important role in osteogenesis. [10] Male and females are equally affected, and no hereditary features have been discovered. The onset of this rare disease is insidious, and the first symptom is usually pain because of the sub-periosteal bone formation. Range of movement limitation and joint deformities develop gradually. Limb length discrepancy and joint contractures may be seen in Melorheostosis. Soft tissue involvement in the form of soft tissue masses, scleroderma, and vascular malformations are also reported [11,12,13]
Radiologic patterns on plain radiographs of Melorheostosis include [5]
Osteoma like pattern
Classical candle wax like pattern
Osteopathic striata pattern
Myositis ossificans pattern
Mixed pattern
In most cases, a biopsy is not needed for the diagnosis of Melorheostosis, but it may be useful in case of uncertain radiographic appearance and dignity of a lesion. Most biopsy sections present a nonspecific image with dense cortical thickening with islands of cartilage, surrounded by lamellar bone in normal or irregular Haversian systems. Morris described (1963) in his sections dense bone mass with an irregular pattern of the Haversian systems, vascular obliteration, and inflammatory cells within surrounding mesenchymal tissue with areas of metaplastic cartilage. Enlarged and thickened bony trabeculae, that contain normal-appearing Haversian systems, which may be irregularly arranged or almost obliterated, are characteristic histologic appearances in most cases of Melorheostosis [11]. Intraarticular melorheostosis can present the characteristics mentioned above together with cartilaginous formations or capping of hyaline cartilage, which may lead to misdiagnosis of a highly differentiated chondrosarcoma or osteochondroma.
Treatment options for Melorheostosis are limited and none of them have yielded a successful cure for the disease.
Nonoperative therapeutic options in symptomatic melorheostosis include physical and ergotherapy, nonsteroidal and opioid analgesics. There are also isolated case reports of successful management of pain with bisphosphonates in literature. Denosumab has a place in the treatment of melorheostosis when the effect of bisphosphonate treatment is insufficient [14]
Surgical options include resection of the osteosclerotic masses from osseous and soft tissues, decompression of nerves and vessels, capsulotomy, tendon release, and fasciotomy for pain and contracture management, often with uncertain results.
Amputations are rare. Due to the high recurrence rates of contractures, surgical procedures should be performed at the end of growth or a combination of surgical procedures and brace therapy or external fixation should be forced in phases of growth acceleration. Shortening of the contralateral limb is the preferred option in the management of limb length inequality.
Conclusion
Melorheostosis is a very rare benign disease. It is diagnosed by characteristic x-ray findings. There is no definite treatment available only symptomatic treatment is given. However, newer modalities of treatment such as Denosumab, Bisphosphonates have shown improvement in symptoms. However, more research needs to be done in this direction.
References
- Leri A, Joanny J (1922) Une affection non décrite des os hyperostose “en coulée” sur toute la longeur d’un member ou “melorhéostose”. Bull Mem Soc Med Hosp Paris. 46: 1141–5.
- Wynne-Davies R, Gormley J (1985) The prevalence of skeletal dysplasias. An estimate of their minimum frequency and the number of patients requiring orthopedic care. J Bone Jt Surg Br. 67(1): 133–7.
- Campbell CJ, Papademtriou T, Bonfiglio M (1968) Melorheostosis. A report of the clinical, roentgenographic, and pathological findings in fourteen cases. J Bone Joint Surg Am. 50(7): 1281-1304.
- Taylor PM (1976) Melorheostosis. J Foot Surg. 15(2): 55-58.
- Frey Schmidt J (2001) Melorheostosis: A review of 23 cases. Eur Radiol. 11(3): 474-479.
- Ihde LL, Forrester DM, Gottsegen CJ, Masih S, Patel DB, et al. (2011) Sclerosing bone dysplasias: Review and differentiation from other causes of osteosclerosis. Radiographics. 31(7): 1865- 1882.
- Rozencwaig R, Wilson MR, McFarland Jr GB (1997) Melorheostosis. Am J Orthop. 26(2): 83-89.
- Greenspan A, Azouz EM (1999) Bone dysplasia series. Melorheostosis: Review and update. Can Assoc Radiol J. 50(5): 324-330.
- Moreno Alvarez MJ, Lázaro MA, Espada G, Barceló HA, Maldonado Cocco A (1996) Linear scleroderma and melorheostosis: Case presentation and literature review. Clin Rheumatol. 15(4): 389-393.
- Kim J-E, Kim E-H, Han E-H, Park RW, Park IH, et al. (2000) ATGF-ß-induciblecelladhesionmolecule, ßig-h3,is downregulated in melorheostosis and involved in osteogenesis. J Cell Biochem. 77(2): 169–178.
- Morris JM, Samilson RL, Corley CL (1963) Melorheostosis. Review of the literature and report of an interesting case with nineteen year follow up. J Bone Joint Surg. 45: 1191–1206.
- Judkiewicz AM, Murphey MD, Resnik CS, Newberg AH, Temple HT, et al. (2001) Advanced imaging of melorheostosis with emphasis on MRI. Skeletal Radiol. 30(8): 447–53.
- Ethunandan M, Khosla N, Tilley E, Webb A (2004) Melorheostosis involving the craniofacialskeleton. J Craniofac Surg. 15: 1062–1065.
- Byberg S, Abrahamsen B, Kassem M, Ralston S, Schwarz P (2018) Clinical improvement in a patient with monostotic melorheostosis after treatment with denosumab: a case report. Journal of Medical Case Reports. 12(1): 278.