Pradeep Kumar Devarakonda MD1, Kishan Reddy2, Vladimir K. Gotlieb, MD2, R. Joshua Dym MD3*
1Cardiology Department/ Ichan school of medicine, NY
2Department of Medicine, Division of Hematology/Oncology, Brookdale University Hospital Medical Center, Brooklyn, NY
3Department of Radiology, University Hospital, Rutgers New Jersey Medical School, Newark, NJ
*Corresponding Author: R. Joshua Dym MD, Department of Radiology, University Hospital, Rutgers New Jersey Medical School, Newark, NJ.
Abstract
The coronavirus (COVID-19) pandemic has brought profound disruptions to the health care systems globally. One of the severe consequences of the Covid-19 pandemic is a global scarcity of iodinated contrast agents (ICA) due to the recent government-mandated lockdown in Shanghai, China. This halted the production of a water-soluble iodine contrast at a significant General Electric factory (of the GE Healthcare subsidiary). Many elective diagnostic tests and procedures are being delayed because of this, which substantially impacts patient health care. Initially, Gadolinium-based Computed tomography Angiography (Gb-CTA) was proved an excellent alternative diagnostic test, especially in patients for whom MRI with gadolinium contrast is not feasible, or CTA with an iodinated difference is contraindicated due to iodine-related issues. But due to the concerns of nephrogenic systemic fibrosis and the cost of gadolinium, this alternative option did not become popular. The scarcity of iodinated contrast once again highlighted the need to use the gadolinium-based CTA. Advancements in CT technology, new data on more stable gadolinium agents, and methods to reduce the contrast dose showed that Gb-CTA studies are possible.
Keywords: CTA; angiography; gadolinium-based contrast agent; iodine contrast; Gadolinium-based Computed tomography Angiography; Radiology; Contrast shortage; Covid-19.
Introduction
A large General Electric facility in Shanghai discontinued the manufacture of a water-soluble iodine contrast Omnipaque (iohexol) in April 2022. This has resulted in a significant supply chain disruption of one of the most widely used low-osmolality contrast agents in diagnostic and interventional radiology [1]. Although production has now resumed, iodinated contrast is likely to remain deficient for several months, and due to this shortage, many non-emergency tests are being postponed [2]. Recently, the FDA has further announced that two additional contrast agents, Omnipaque (iohexol, from GE Healthcare) and Visipaque (iodixanol, also from GE Healthcare), are also low in supply [3].
Computed tomography (CT) scans and Magnetic resonance imaging (MRI) are valuable diagnostic tools that help radiologists and physicians diagnose various medical conditions. The first commercial CT scanner was created in the 1970s, MRI in the 1980s [4], and since then, several advanced technologies have taken place in both imaging sectors. In the United States, approximately 70 million CT scans and 35 million MRI scans are conducted annually [5]. CT angiography (CTA) is a non-invasive method that uses an intravenous contrast agent to analyze vascular anatomy and pathology. CT scan is best for assessing endo and perivascular abnormalities as it has a more excellent spatial resolution than magnetic resonance imaging (MRI) [6,7]. Standard angiography may not be appropriate for certain patients, such as those with an allergy to iodinated contrast material or receiving radioactive iodine treatment for thyroid disorders. Similarly, patients with implantable devices, postoperative clips, uncontrolled movements, claustrophobia, or surgical changes that might compromise the magnetic resonance (MR) signal may be unsuitable for MR angiography. Thus, gadolinium usage in CTA has been studied as an alternative option; however, despite multiple studies demonstrating the feasibility of gadolinium catheter arteriography, the use of gadolinium for CTA has not generally been accepted as a viable substitute [8].
Here, the need for gadolinium-based contrast agents (GBCA) is emphasized again due to the shortage of iodinated contrast in the COVID-19 pandemic and other indications mentioned above. This study aims to provide data on using GBCA instead of iodinated difference for CTA during this crisis.
Iodinated contrast
In the 1950s, an iodine-based contrast material containing three iodine atoms and a benzene ring was developed. This original agent was ionic and high-osmolar. Subsequently, non-ionic versions were developed and appeared on the market in the 1980s. This minimized the hypertonic and chemo-toxic adverse effects of iodine contrast [9,10]. Iodine-based contrast media are now considered low risk; however, there remain some potential adverse effects of these agents, which can limit their use in certain situations.
Iodinated contrast-induced renal complications and prevention:
Contrast-induced acute kidney injury (CI-AKI), also referred to as contrast-induced nephropathy (CIN), is described as an abrupt decline in kidney function due to intravenous delivery of iodine-based contrast media [8]. The pathophysiology likely depends on three independent mechanisms: medullary ischemia, direct tubular cell damage, and reactive oxygen species production. The role of each of these pathways in causing CI-AKI in a patient is still unknown [11]. Research in the past fifteen years has challenged the conventional wisdom that iodinated contrast carries a significant risk of CIN. In 2008, Newhouse et al. examined 32,161 patients and discovered that the rise in creatinine levels among those patients who did not receive contrast material was as standard as those who received contrast material [12]. In 2013, two controlled studies helped advance understanding of CIN's risk (or lack of risk). Davenport et al. found that an estimated glomerular filtration rate (eGFR) of ≥ 60 ml/min was not linked with an increased incidence of evolving post-contrast AKI (OR 1.00; 95 percent CI 0.86–1.16), while patients with pre-existing kidney damage or those with an eGFR of < 30 ml/min did have a higher risk of developing AKI post-CT (OR 2.96; 95 percent CI 1.22–7.17) [13]. In another study, McDonald et al. demonstrated that intravenous iodinated contrast media did not cause any decrease in renal function following contrast material use, even in patients with poor renal function [14]. A review by Katzberg et al. found that patients who underwent coronary angiography had a 37 % rate of CIN and a 22 % mortality rate, while patients undergoing iodinated contrast-enhanced CT exhibited 0 % CIN and 0 % mortality, concluding that fear of CI-AKI due to iodinated contrast might have been exaggerated in the past [15].
According to the articles mentioned above, patients with adequate renal function are not at a higher risk of developing post-contrast AKI; however, it is uncertain if individuals with an eGFR of less than 30 have a higher risk of post-contrast AKI [8]. Elevation of serum creatinine might be due to confounding variables rather than the iodinated contrast administration [4]. The American College of Radiology (ACR) Committee on Drugs and Contrast Media believes that CI-AKI is a genuine phenomenon, although it is an uncommon entity [8].
Prevention of CI-AKI includes
Avoiding all forms of contrast.
Using a low osmolarity contrast medium.
Expansion of the pre-exposure volume (with isotonic crystalloid preferred over half-isotonic crystalloid).
It is not recommended that all patients require a standard diagnostic examination of their renal function before receiving contrast, only those with risk factors for renal dysfunction [8]. Also, the iodinated difference can be used safely in patients with chronic hemodialysis (HD) who are anuric. Thus, regular post-procedural HD is not required in HD patients receiving IV contrast.
One other factor to consider when administering iodinated contrast is that patients with advanced chronic kidney disease (CKD) (stage IV or V; eGFR < 30) or who have AKI should stop taking metformin before or at the time of the procedure. Metformin must be stopped for 48 hours after the process in this group of individuals and should be resumed after rechecking eGFR once it is normalized [8].
Gadolinium:
Gadolinium has been used as an IV contrast medium for MRI since 1988. It is a rare earth metal in the periodic table's lanthanide class. Because it is very paramagnetic, it modifies the relaxation of water so that it allows differentiation between normal and diseased tissues in imaging. Gadopentetate dimeglumine (Magnevist®) is the first commercially available MRI contrast medium used in clinical studies. GBCAs have also been used in CT imaging since 1989; however, it was not frequently used due to limitations of the single-detector row CT technique. Helical or spiral CT elevated the effectiveness of gadolinium use with CT imaging [4,16,17].
Gadolinium-based contrast agents, renal complication, and prevention:
Initially, GBCAs were considered very safe and a reliable alternative to iodinated contrast with no significant side effects. However, in the early 2000s, a series of studies linked gadolinium contrast to NSF [19]. NSF is an uncommon disease affecting the skin and subcutaneous tissues, which has been described among patients with chronic kidney disease (CKD) but rarely among patients with normal kidney function [18]. Initially, fibrosis was thought to be localized only to the skin and subcutaneous tissues. Thus, it was named nephrogenic fibrosing dermopathy. However, postmortem examinations indicated that the fibrosis could spread to other organ systems such as the heart, skeletal muscles, lungs, and esophagus [20,21].
Decreased renal function is the most significant risk factor for developing NSF with gadolinium use. This is explained by the etiology and pathophysiology of this condition: GBCAs are gadolinium cation-containing chelates. When gadolinium chelates are in the body for an extended period, free gadolinium ions are released, which is hazardous due to their poor solubility. The stimulation of circulating fibrocytes by free gadolinium causes a fibrotic response [8]. Gadolinium is mainly eliminated through the kidneys, with a half-life of around 2 hours in individuals with normal kidney function, while it can last up to 120 hours in patients with severe CKD and requires > 3 hemodialysis sessions to be removed from dialysis patients [18,19]. Gadolinium ions are coupled to a chelating agent that is either linear or macrocyclic. With a linear agent, patients with CKD stage 4 or 5 have a 1.7 percent probability of developing nephrogenic systemic fibrosis (NSF), whereas, with a macrocyclic agent, the risk decreases to a minimum as macrocyclic GBCAs are more thermodynamically stable (low ratio of free gadolinium to complexed ligand at steady state) and kinetically neutral (extended half-life for gadolinium separation from its ligand) [4,16]. According to the ACR, GBCAs are divided into groups based on their structure and likelihood of causing NSF [Table-1] [8]
Table 1: ACR classification of Gadolinium relative to structure and NSF risk [8]
|
ACR group |
structure |
Generic name |
U.S trade name |
|
Group -I |
Linear nonionic |
Gadodiamide |
Omniscan |
|
Linear nonionic |
Gadoversetamide |
OptiMARK |
|
|
Linear ionic |
Gadopentetate dimeglumine |
Magnevist |
|
|
Group -II |
Linear ionic |
Gadobenate dimeglumine |
MultiHance |
|
Macrocyclic nonionic |
Gadoteridol |
ProHance |
|
|
Macrocyclic nonionic |
Gadobutrol |
Gadavist |
|
|
Macrocyclic ionic |
Gadoterate meglumine |
Dotarem |
|
|
Macrocyclic ionic |
Gadoterate meglumine |
Clariscan |
|
|
Group -III |
Linear ionic |
Gadoxetate disodium |
Eovist |
According to the most recent data, NSF or renal toxicity risk after administering group II GBCAs is relatively minimal. Thus, regardless of their dialysis status, withholding group II GBCAs from a patient with renal impairment, the possible danger of late diagnosis or misinterpretation from delaying may exceed the risk of NSF. There is limited data on NSF risk in group III agents, but the group I agents have a high risk of developing NSF in CKD patients [16].
Gadolinium use has also been known to cause CIN among CKD patients. However, it is dose dependent. In one trial, 12.1 % of individuals with CKD who were administered 0.2 mmol/kg of gadolinium had developed CIN, while a dosage of 0.1 mmol/kg was not shown to be nephrotoxic in another study [22,23].
As described, both iodinated and gadolinium-based contrast agents have their attendant risks [Table 2], but overall, the chances are low for these agents when used appropriately.
Table 2: Risks of nephrogenic systemic fibrosis (NSF) and contrast-induced nephropathy (CIN) associated with gadolinium and iodine [18,8,21].
|
|
NSF |
CI-AKI(CIN) |
|
contrast agent |
1. Gadolinium |
1. Iodinated contrast 2. Gadolinium (rarely) |
|
DEFINITION |
Nephrogenic systemic fibrosis is a multiple organ system fibrosing disease that develops in individuals with renal insufficiency who are exposed to gadolinium-based contrast agents. |
The term contrast-induced acute kidney damage (CI-AKI), also known as contrast-induced nephropathy (CIN), refers to an abrupt impairment in renal function produced by the intravascular infusion of iodinated contrast media. |
|
Pathogenesis |
The precise cause of NSF is unknown. The most frequently accepted theory is due to the longer clearance time periods of GBCA in patients with kidney injuries. Gadolinium ions dissociate and bond to an anion like phosphate, forming an insoluble precipitate when it stays in the body for a longer period, it deposits into numerous tissues causing stimulation of circulating fibrocytes. |
Renal hemodynamic alterations (vasoconstriction) and direct tubular toxicity have been identified as possible etiologic causes. |
|
Subjects at risk |
Advanced CKD and dialysis patients |
Pre-existing renal dysfunction |
|
Additional risk factors |
|
1. Diabetes 2. Advanced age 3. Hypertension 4.Cardiovascular problems 5. Dehydration 6.Nephrotoxic medications 7. High contrast volumes 8. Multiple myeloma 9. Low eGFR |
|
Clinical presentation and relevance |
Usually starts with swelling in the lower limbs, followed by skin induration. Fibrotic alterations can impact the muscles, heart, liver, and lungs, which may explain why these individuals have a higher death rate. |
Serum creatinine levels rise three days after contrast injection. Even minor increases in serum creatinine can reflect a considerable decline in eGFR in individuals with severe CKD. This can lead to dialysis dependency, which has severe morbidity. |
|
Screening |
Patients using Group I or Group III gadolinium, medications should be checked for diseases and other variables that might lead to renal dysfunction. |
Any kidney disease (e.g., CKD, distant AKI, kidney surgery, kidney ablation, albuminuria). Patient’s age, Diabetes mellitus, and if they have been treated for hypertension. |
|
Prevention |
Unless the diagnostic data is critical and is not obtainable with non-contrast-enhanced MRI, avoid using it. Group II is recommended, and individuals who are at risk of developing NSF as stated above should be identified prior to injection of group I and III GBCAs. |
a) Using contrast media with a low osmolality b) Expansion of Volume c) Avoidance of Iodinated Contrast medium |
Additional considerations for iodinated and Gadolinium-based contrast agents:
Breastfeeding post IV contrast: Breastfeeding is deemed safe after injecting iodinated and gadolinium IV contrast. Given the minimal risk of severe side effects, pumping and discarding breast milk generated within 24 hours of either iodinated or GBCA injection is optional [4,8].
Pregnancy post IV contrast: Stillbirth and infant mortality have been linked to gadolinium exposure. Gadolinium should be avoided in pregnant individuals unless the therapeutic advantages outweigh the hazards due to the increased risk of severe fetal outcomes. No studies have shown that iodinated IV contrast causes damage to the fetus; therefore, screening for pregnancy is not indicated before its administration [4,8].
Acute reactions to IV iodine and gadolinium:
Adverse reactions can occur either due to iodinated or gadolinium-based contrast agents. Total estimates of all adverse reactions to IV iodinated contrast range from 1 to 12 % in various studies; however, severe reactions only comprise about 0.01 to 0.2 % of these reactions [24,25]. Mortele et al. mentioned in their research that among 29,508 patients, 0.7 % had adverse events, most of which were mild side effects such as flushing, itching, rash, and nausea [26].
Hypersensitivity reactions are the absolute contraindication to GBCAs, and the total incidence of any adverse event appears to be less than 5% [27]. Although these side effects are more common in the iodinated contrast group than in the gadolinium-based contrast group, about 0.16 % (51 patients) of 32,659 patients who received a GBCA reported acute adverse reactions. However, only two of these patients experienced a severe (i.e., anaphylactic) reaction. Notably, patients with prior adverse reactions to iodinated contrast may also be at higher risk of a reaction to gadolinium-based contrast [8,28].
Contrast reactions may be categorized as allergic-like or physiologic. “Allergic-like” reactions are believed to result from an immune response that results in symptoms similar to a typical allergic reaction, such as food, whereas physiologic reactions are physiologic responses to the contrast material, as described in Table 3. While corticosteroid premedication is believed to help prevent allergic-like reactions, this is not thought to be the case for physiologic reactions, which occur via a different mechanism [8].
Table 3: Adverse reactions to contrast agents [8]:
|
|
Allergic -like |
Physiologic |
|
Mild |
Mildpruritus /urticaria Edema of the skin Mild "itchy"/"scratchy" throat Nasal congestion Conjunctivitis, sneezing, and rhinorrhea |
Light nausea and vomiting Flushing/warmth/chills for a short period of time Dizziness/anxiety/alteration in taste/headache Mild hypertension Vasovagal response that resolves on its own |
|
Moderate |
Diffuse Urticaria or pruritis Diffuse erythema, steady vital signs Facial edema, throat tightness or hoarseness without dyspnea Wheezing and bronchospasm, with or without mild hypoxia |
Prolonged nausea or vomiting Chest discomfort that is isolated Vasovagal response that necessitates and responds to therapy Hypertensive urgency |
|
Severe |
Facial edema accompanying dyspnea, widespread edema Hypotension with diffuse erythema Edema of the larynx with stridor and/or hypoxia, substantial hypoxia, wheezing/ bronchoconstriction (hypotension + tachycardia), Anaphylactic shock |
Treatment-resistant vasovagal response Seizures, convulsions Hypertensive emergency |
Gadolinium usage in CTA:
Despite developments in MR imaging technology, CT continues to outperform MR imaging in evaluating endo and perivascular anomalies, particularly at the level of the pulmonary circulation and lung parenchyma, for which the speed of CT imaging can help avoid significant motion artifacts due to respiration [29]. Bloem and Wondergem were the first to publish regarding the use of gadolinium in computed tomography (CT) in 1989. They included an image of the urinary bladder and renal collecting system obtained using gadolinium, similar to iodine-enhanced CT in 2 patients [30]. Similarly, in 1993, Kinno et al. used gadolinium-chelate for intra- arterial digital subtraction angiography (DSA) in a patient with a severe allergic reaction to iodinated contrast media [31].
Iodinated contrast agents are quantified by the weight of iodine atoms per ml (mg I/ml), whereas gadolinium chelates are quantified by the number of atoms per ml, i.e., mmol/ml. A gadolinium solution with a concentration of 0.5 mmol/ml has the same number of atoms as an iodinated contrast solution with a concentration of 63 mg I/ml, and a gadolinium-chelate at 0.5 mmol/ml would produce the same degree of attenuation as iodinated contrast solution with a concentration 126 mg I/ml. On CTA, gadolinium appears hyperdense, and the usual dosage for CTA is frequently quadrupled, i.e., 0.4 mmol/kg compared to 0.1 mmol/kg for MRI. Doses like 0.3 mmol/kg - 0.4 mmol/kg gadolinium have been utilized in CTA of the aorta, pulmonary or cervical arteries in various case reports/trials [18,6,32,27,7].
The utilization of gadolinium-based contrast in CT angiography for pulmonary circulation was initially reported in a single case report by Coche et al. [17]. They successfully detected an acute pulmonary embolism in their patient (who had an allergy to iodinated contrast and renal failure) by performing a spiral (dual-detector) CT with a gadolinium-based difference. Later, Remy-Jardin et al. reported in their study of 39 patients that CT pulmonary angiograms using gadolinium-based contrast agents were diagnostic but that CTs with 16 detectors (rather than 4) were required for high-quality examinations. The frequency of diagnostic CT angiograms was significantly greater with 16–detector row CT technology (94 % vs. 68 %) (P = .007), and the scanning time was also shorter in this group [33]. Even patients with pre-existing renal insufficiency could tolerate the gadolinium-based contrast agent at doses of 0.3 and 0.4 mmol/kg, and only one of the patients had a transient reduction of renal function. Otherwise, there were no reported adverse events.
Remy-Jardin et al. also performed similar research on 60 patients to compare the effects of 0.3 mmol/kg (group A) vs. 0.4 mmol/kg (group B) doses. 83 % of CT angiograms in group A and 100 % in group B were evaluated as diagnostic tests, and the researchers concluded that GBCAs are an adequate alternate contrast material for CT pulmonary angiography. In that study, only 1 patient had developed a temporary reduction in creatinine clearance, which was restored within 2 days to baseline kidney function [6].
After retrospectively analyzing a series of 20 patients with an average pre-procedural serum creatinine of 2.7 mg/dL, Gemmete et al. determined that vast doses of gadolinium (80 to 440 ml) are relatively safe in association with interventional procedures [34]. Similarly, research conducted by Tombach et al. using 1.0 mol/L gadobutrol (a greater concentration than the standard dosage of 0.5mol/L) found no effect on kidney function, even in patients with prior kidney damage, indicating that gadolinium is safe in individuals with compromised renal function [35].
To lessen the amount of contrast, many methods have been developed. In a porcine model, Bae et al. used diluted gadolinium and demonstrated that combining a fast CT scanner with bolus monitoring techniques (and maybe adding a saline bolus flush or "chaser") could significantly reduce the volume of contrast required for gadolinium CTA [36]. Another investigation revealed an increase in optic density when four parts of gadolinium-based difference were combined with one piece of iodinated contrast in digital subtraction angiography (DSA) [37]. To minimize the volume and improve imaging quality, Nadjiri et al. employed a 64-slice single-source dual-layer spectral CT system with lower dosages of 0.2 mmol/kg body weight Gd-DOTA (a macrocyclic GBCA), monoenergetic pictures, and a bolus-tracking technique. These approaches demonstrated that low-dose Gd-based angiography is practically possible [38]. Smadja et al. also showed that gadolinium-based contrast employed for thoracic CTA using 64-slice MDCT was superior to 16-slice MDCT in terms of diagnostic quality tests [39].
Similarly, Henson et al. found that Gadolinium-enhanced (0.4 mmol/kg) CTA for head and neck arteries is technically possible and helpful in patients who cannot utilize iodinated contrast material [40]. Carrascosa et al. demonstrated that, despite gadolinium's reduced attenuation, diagnostic accuracy for identifying obstructive coronary artery disease is comparable to iodine-enhanced CT [41].
Only CO2 and gadolinium-chelates have been approved as feasible alternatives for iodine contrast. According to the articles mentioned above, diagnostic CT exams can be performed following intravenous injection of GBCAs. Additionally, there are several other reported uses of GBCAs, including galactography, retrograde pyelography, endoscopic retrograde cholangiography, cystography, myelography, cisternography, and urethrocystography, intravenous urography, percutaneous nephrostomy, and biliary tract drainage. The use of GBCAs for these examinations requires no particular logistics and can be injected by hand or via a standard automated injection system with the same pressures and flow rates as iodinated contrast [27].
Gadolinium-based contrast media may be significantly more expensive (by 4 or 5 times) than iodinated nonionic compounds per ml, although this may also depend to some degree on the number and size of the vials required to be opened for a specific examination. However, when compared to the length of a hospital stay and the dangers of delayed or inadequate treatments, GBCAs are a reasonable and suitable option, especially given the current scarcity [42,43].
Conclusion: [Figure-1]
GBCAs can be used for diagnostic CT angiography when there are contraindications to iodinated contrast or in situations like the iodinated contrast shortage we are currently experiencing. Many advanced technologies from the past few years will reduce the limitations of gadolinium. More stable gadolinium agents may help reduce the risk of NSF among those patients with renal disease.
Similarly, dilution or mixing of gadolinium with iodine or saline and bolus tracking methods would decrease the total volume of contrast necessary without compromising the study. The recent developments in multi-detector row CT scan developments in DSCT and spectral for cardio-thoracic scanning will also provide better temporal resolution using contrast.
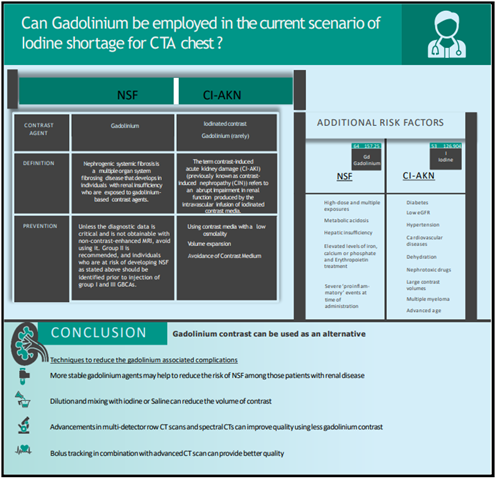
Figure 1: Explaining the difference between NSF and CI-AKI along with conclusion
References
- Salazar G, Mossa-Basha M, Kohi MP, Burke LM (2022) Short- Term Mitigation Steps During the Iohexol Contrast Shortage: A Single Institution's Approach. J Am Coll Radiol. S1546- 1440(22)00348-9.
- Shanghai factories scramble to reopen as COVID lockdown lingers.
- FDA reports shortage of GE contrast media for CT imaging.
- Huynh K, Baghdanian AH, Baghdanian AA, Sun DS, Kolli KP, et al. (2020) Updated guidelines for intravenous contrast use for CT and MRI. Emergency radiology. 27(2): 115–126.
- OECD (2017) Health at a glance 2015: OECD indicators.
- Remy-Jardin M, Bahepar J, Lafitte JJ, Dequiedt P, Ertzbischoff O, et al. (2006) Multi-detector row CT angiography of pulmonary circulation with gadolinium-based contrast agents: prospective evaluation in 60 patients. Radiology. 238(3): 1022–1035.
- Peña CS, Kaufman JA, Geller SC, Waltman AC (1999) Gadopentetate dimeglumine: a possible alternative contrast agent for CT angiography of the aorta. Journal of computer assisted tomography. 23(1): 23–24.
- American College of Radiology (2021) ACR manual on contrast media.
- Pollack HM (1999) History of lodinated Contrast Media. In: Thomsen, H.S., Muller, R.N., Mattrey, R.F. (eds) Trends in Contrast Media. Medical Radiology. Springer, Berlin, Heidelberg.
- Nyman U, Ekberg O, Aspelin P (2016) Torsten Almén (1931- 2016): the father of non-ionic iodine contrast media. Acta radiologica. 57(9): 1072–1078.
- Mohammed NM, Mahfouz A, Achkar K, Rafie IM, Hajar R (2013) Contrast-induced Nephropathy. Heart views : the official journal of the Gulf Heart Association. 14(3): 106–116.
- Newhouse JH, Kho D, Rao QA, Starren J (2008) Frequency of serum creatinine changes in the absence of iodinated contrast material: implications for studies of contrast nephrotoxicity. AJR. American journal of roentgenology. 191(2): 376–382.
- Davenport MS, Khalatbari S, Cohan RH, Dillman JR, Myles JD, et al. (2013) Contrast material-induced nephrotoxicity and intravenous low-osmolality iodinated contrast material: risk stratification by using estimated glomerular filtration rate. Radiology. 268(3): 719–728.
- McDonald RJ, McDonald JS, Bida JP, Carter RE, Fleming CJ, et al. (2013) Intravenous contrast material-induced nephropathy: causal or coincident phenomenon?. Radiology. 267(1): 106–118.
- Katzberg RW, Newhouse JH (2010) Intravenous contrast medium-induced nephrotoxicity: is the medical risk really as great as we have come to believe?. Radiology. 256(1): 21–28.
- Weinreb JC, Rodby RA, Yee J, Wang CL, Fine D, et al. (2020) Use of Intravenous Gadolinium-Based Contrast Media in Patients With Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation. Kidney medicine. 3(1): 142–150.
- Coche EE, Hammer FD, Goffette PP (2001) Demonstration of pulmonary embolism with gadolinium-enhanced spiral CT. European radiology. 11(11): 2306–2309.
- Pugliese F (2010) Gadolinium-enhanced coronary CT angiography: improved safety?. Heart (British Cardiac Society). 96(19): 1513–1515.
- Grobner T (2006) Gadolinium--a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis?. Nephrol Dial Transplant. 21(4): 1104–1108.
- Ting WW, Stone MS, Madison KC, Kurtz K (2003) Nephrogenic fibrosing dermopathy with systemic involvement. Archives of dermatology. 139(7): 903–906.
- Schlaudecker JD, Bernheisel CR (2009) Gadolinium-associated nephrogenic systemic fibrosis. American family physician. 80(7): 711–714.
- Ergün I, Keven K, Uruç I, Ekmekçi Y, Canbakan B, et al. (2006) The safety of gadolinium in patients with stage 3 and 4 renal failure. Nephrology, dialysis, transplantation. 21(3): 697–700.
- Haustein J, Niendorf HP, Krestin G, Louton T, Schuhmann- Giampieri G, et al. (1992) Renal tolerance of gadolinium- DTPA/dimeglumine in patients with chronic renal failure. Investigative radiology. 27(2): 153–156.
- Bush WH, Swanson DP (1991) Acute reactions to intravascular contrast media: types, risk factors, recognition, and specific treatment. AJR. American journal of roentgenology. 157(6): 1153–1161.
- Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, et al. (1990) Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. 175(3): 621–628.
- Mortelé KJ, Oliva MR, Ondategui S, Ros PR, Silverman SG (2005) Universal use of nonionic iodinated contrast medium for CT: evaluation of safety in a large urban teaching hospital. AJR. American journal of roentgenology. 184(1): 31–34.
- Strunk HM, Schild H (2004) Actual clinical use of gadolinium- chelates for non-MRI applications. Eur Radiol. 14(6): 1055– 1062.
- Abujudeh HH, Kosaraju VK, Kaewlai R (2010) Acute adverse reactions to gadopentetate dimeglumine and gadobenate dimeglumine: experience with 32,659 injections. AJR. American journal of roentgenology. 194(2): 430–434.
- Kauczor HU, Kreitner KF (1999) MRI of the pulmonary parenchyma. European radiology. 9(9): 1755–1764.
- Bloem JL, Wondergem J (1989) Gd-DTPA as a contrast agent in CT. Radiology. 171(2): 578–579.
- Kinno Y, Odagiri K, Andoh K, Itoh Y, Tarao K (1993) Gadopentetate dimeglumine as an alternative contrast material for use in angiography. AJR. American journal of roentgenology. 160(6): 1293–1294.
- Gupta AK, Alberico RA, Litwin A, Kanter P, Grossman ZD (2002) Gadopentetate dimeglumine is potentially an alternative contrast agent for three-dimensional computed tomography angiography with multidetector-row helical scanning. Journal of Computer Assisted Tomography. 26(6): 869-874.
- Remy-Jardin M, Dequiedt P, Ertzbischoff O, Tillie-Leblond I, Bruzzi J, et al. (2005) Safety and effectiveness of gadolinium- enhanced multi-detector row spiral CT angiography of the chest: preliminary results in 37 patients with contraindications to iodinated contrast agents. Radiology. 235(3): 819–826.
- Gemmete JJ, Forauer AR, Kazanjian S, Dasika N, Williams DM, Cho K. Safety of large volume gadolinium angiography. (abstr) J Vasc Interv Radiol 2001; 12[part 2]: S28
- Tombach B, Bremer C, Reimer P, Kisters K, Schaefer RM, et al. (2001) Renal tolerance of a neutral gadolinium chelate (gadobutrol) in patients with chronic renal failure: results of a randomized study. Radiology. 218(3): 651–657.
- Bae KT, McDermott R, Gierada DS, Heiken JP, Nolte MA, et al. (2004) Gadolinium-enhanced computed tomography angiography in multi-detector row computed tomography: initial observations. Academic radiology. 11(1): 61–68.
- Badiola CM (2004) Use of a mixture of gadolinium and iodinated contrast for angiography. Cardiovascular and interventional radiology. 27(2): 148–150.
- Nadjiri J, Pfeiffer D, Straeter AS, Noël PB, Fingerle A, et al. (2018) Spectral Computed Tomography Angiography With a Gadolinium-based Contrast Agent: First Clinical Imaging Results in Cardiovascular Applications. Journal of thoracic imaging. 33(4): 246–253.
- Smadja L, Rémy-Jardin M, Dupuis P, Deken-Delannoy V, Devos P, et at. (2009) Gadolinium-enhanced thoracic CTA: retrospective analysis of image quality and tolerability in 45 patients evaluated prior to the description of nephrogenic systemic fibrosis]. Journal de radiology. 90(3 Pt 1): 287–298.
- Henson JW, Nogueira RG, Covarrubias DJ, Gonzalez RG, Lev MH (2004) Gadolinium-enhanced CT angiography of the circle of Willis and neck. AJNR. American journal of neuroradiology. 25(6): 969–972.
- Carrascosa P, Capuñay C, Bettinotti M, Goldsmit A, Deviggiano A, et al. (2007) Feasibility of gadolinium-diethylene triamine pentaacetic acid enhanced multidetector computed tomography for the evaluation of coronary artery disease. Journal of cardiovascular computed tomography. 1(2): 86–94.
- Nyman U, Elmståhl B, Leander P, Nilsson M, Golman K, et al. (2002) Are gadolinium-based contrast media really safer than iodinated media for digital subtraction angiography in patients with azotemia?. Radiology. 223(2): 311–329.
- Kane GC, Stanson AW, Kalnicka D, Rosenthal DW, Lee CU, et al. (2008) Garovic, Comparison between gadolinium and iodine contrast for percutaneous intervention in atherosclerotic renal artery stenosis: clinical outcomes. Nephrology Dialysis Transplantation. 23(4): 1233–1240.



