Sonia Narula1, Mariam Jacob2*
1Consultant Radiologist, Department of Radiology, St Albans City Hospital, Hertfordshire, UK
2Consultant Radiologist, Department of Radiology, Watford General Hospital, Hertfordshire, UK
*Corresponding Author: Mariam Jacob, Consultant Radiologist, Department of Radiology, Watford General Hospital, Hertfordshire, UK
Abstract
Mammary tuberculosis is a rare disease which can be difficult to diagnose on imaging as it can mimic other pathology in symptomatic patients, such as mastitis, an abscess, or primary breast malignancy.
Introduction
Tuberculosis of the breast has a reported incidence of 0.1 % in developed countries [1]. We present a case of breast tuberculosis in a young Eastern Asian female diagnosed in a UK-based hospital.
Case Summary
The patient is a 35-year-old Chinese female who attended a symptomatic breast clinic. She was born in China and grew up in South Africa.
Clinical history on the ultrasound request form stated, ‘right breast P2 lumpiness ?cysts’ (P2 indicating a clinical suspicion of a benign lesion).
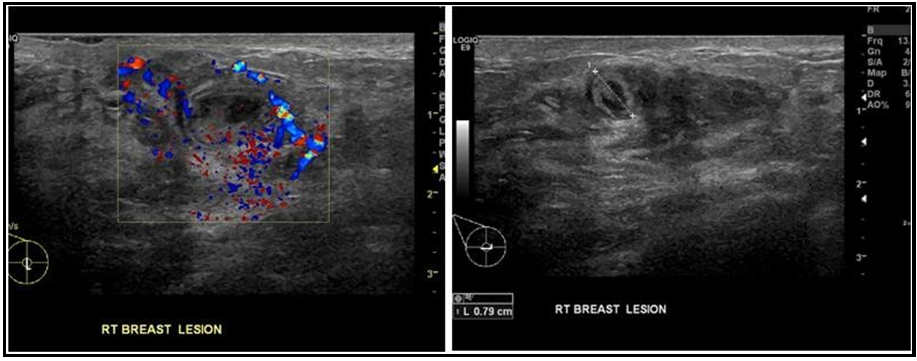
The ultrasound revealed two lesions, one in the 5 o’clock position measuring 10mm and one in the 8 o’clock place measuring 8mm (Figures 1 and 2). They had sonographic appearances of thick- walled cysts, which were aspirated to dryness. The aspirate was documented as ‘creamy’ material, which was discarded as there was no indication for cytological analysis.
Figures 1 and 2: show the ultrasound images of a well-defined heterogeneous lesion measuring 8mm, with peripheral vascularity.
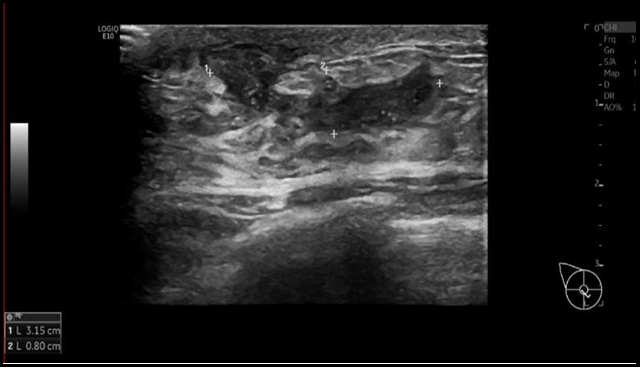
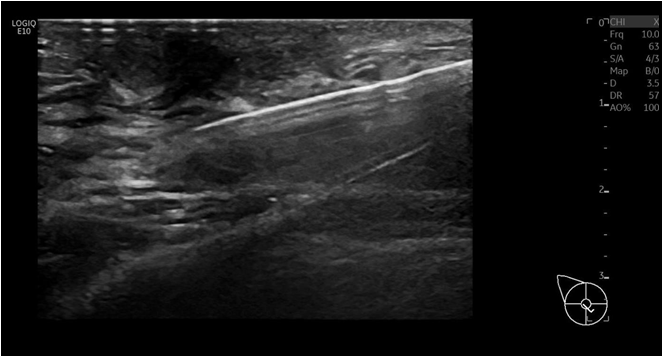
Two months later the patient presented again, with the clinical history on the ultrasound request form stating, ‘recurrent right cyst?’ Ultrasound showed a solitary subareolar 32 x 8mm partly cystic lesion with internal speckling (Figure 3). The axilla was normal. The lesion was described as a U3 lesion (indicating a sonographically indeterminate lesion), suggesting a diagnosis of periductal mastitis. A core biopsy was performed on the lesion with a 14G needle, and three cores were obtained (Figure 4).
Figure 3: shows the ultrasound images of an elongated, hypoechoic lesion with internal debris measuring 32 x 8mm.
Figure 4: shows the ultrasound images of the core biopsy needle within the lesion, after taking a sample.
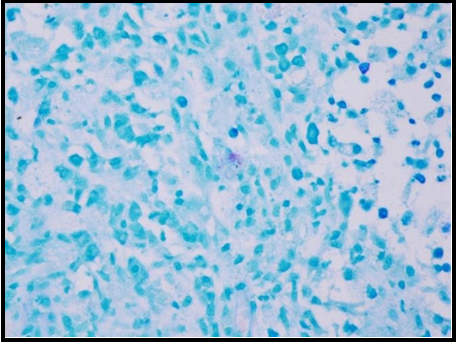
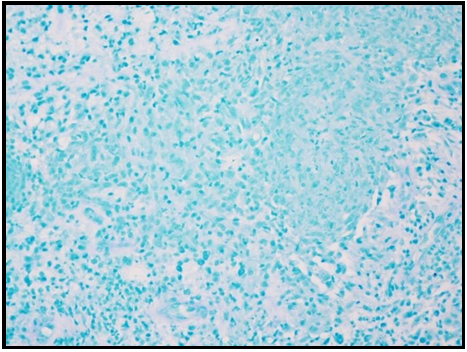
Histology revealed ‘breast tissue with granulomatous inflammation but no definite caseation (B2)’. The sample underwent Ziehl-Neelsen staining, which showed scanty acid-fast bacilli (Figure 5) and granulomatous inflammation (Figure 6), in keeping with active mycobacterial infection.
Figure 5: shows scanty mycobacterial organisms on Ziehl Neelsen stain.
Figure 6: shows granulomatous inflammation on Ziehl Neelsen stain
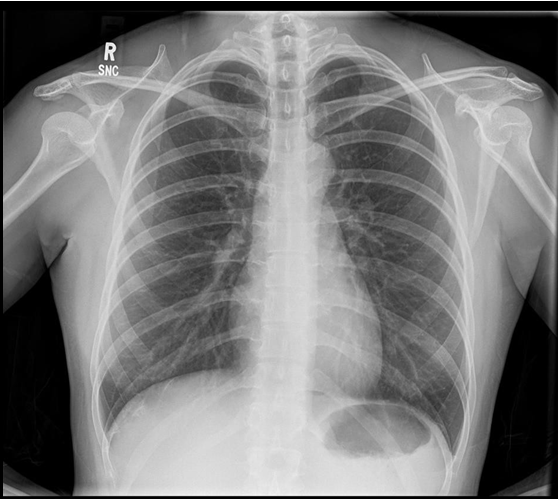
Following diagnosis, the patient had a chest x-ray, which was normal with no features to suggest pulmonary involvement (Figure 7).
Figure 7: shows the chest x-ray, with normal cardiac and mediastinal contours, and clear lung fields.
Discussion
Mammary tuberculosis is a rare disease and therefore low, or not even considered, on the list of differential diagnoses in a patient presenting with a breast lump. In the case presented, the breast lump had a working diagnosis of an infected cyst/mastitis in a young female. Clinical presentation can also be variable; patients can present with a lump, a fistula causing discharge or skin infiltration and nipple retraction in advanced cases [2].
Breast tuberculosis can be primary or secondary. however primary TB is very rare as breast tissue is not a suitable site for the multiplication and survival of tubercle bacilli [3]. However, in pregnant and lactating women, the breast is vascular with dilated ducts predisposed to trauma, making it more susceptible to tuberculosis. Tuberculosis of the male breast has been reported very rarely [4].
Three forms of breast tuberculosis have been described; nodular, diffuse, and sclerosing. Nodular describes a focal lesion in the breast (the most common form); diffuse (or disseminated) is multiple tuberculous foci in the breast, and sclerosing is a fibrotic process [5].
As discussed, imaging features can be non-specific and often mimic breast cancer or abscess [6]. On mammography, there is an ill-defined mass which can cause a reduction in breast volume. Abscesses may be seen as a mass connected to skin thickening by a tract. Adenopathy is seen in 40 % of patients (axillary or intra-mammary), which can be densely calcified [7]. Ultrasound will show a hypoechoic mass, with some (approximately 40 %) having duct ectasia [8].
Acid-fast bacilli are only identified in 12 % of patients [5], therefore not required to make a diagnosis of tuberculosis, as long as there is evidence of caseating granulomas and necrosis. The other differentials for granulomatous inflammation include sarcoidosis, inflammation as a reaction to a tumor, and foreign body reaction – these would have to be correlated with the clinical presentation.
Medical treatment is the mainstay of treatment with six months treatment of anti-tuberculous medication. Surgical intervention is rarely required unless there is diffuse disease needing a mastectomy.
Conclusion
Although rare, it is important to remember breast tuberculosis as a differential and diagnosis of exclusion for a patient presenting with a breast lump, taking into account the patient’s ethnicity and clinical presentation.
The mainstay of diagnosis is histological analysis after biopsy with Ziehl-Neelsen staining as imaging findings can be variable in these patients, and the mainstay of treatment is anti-tubercular therapy.
Declaration of patient consent: The patient’s written consent was obtained.
Financial support and sponsorship: Nil.
Conflicts of interest: No conflicts of interest.
References
- Marinopoulos S, Lourantou D, Gatzionis T, Dimitrakakis C, Papaspyrou I, et al. (2012) Breast tuberculosis: Diagnosis, management and treatment. Int J Surg Case Rep. 3(11): 548-550.
- Khanna R, Prasanna GV, Gupta P, Kumar M, Khanna S, et al.(2002) Mammary tuberculosis: report on 52 cases. Postgrad Med J. 78(921): 422-424.
- Mahasweri V, Tyagi SP, Asraf SM, et al. Tubercular mastitis: A clinicopathological study. Ind J Surg 1993;55:129-33
- da Silva BB, Lopes-Costa PV, Pires CG, Pereira-Filho JD, dos Santos AR (2009) Tuberculosis of the breast: analysis of 20 cases and a literature review. Trans R Soc Trop Med Hyg. 103(6): 559- 563.
- Baharoon S (2008) Tuberculosis of the breast. Ann Thorac Med. 3(3): 110-114.
- Maroulis I, Spyropoulos C, Zolota V Tzorakoleftherakis E (2008) Mammary tuberculosis mimicking breast cancer: a case report. J Med Case Reports 2. 34 (2008).
- Sabaté JM, Clotet M, Gómez A, Heras PDL, Torrubia S, et al. (2005)Radiologic Evaluation of Uncommon Inflammatory and Reactive Breast Disorders. RadioGraphics. 25(2): 411-424.
- Sakr AA, Fawzy RK, Fadaly G, Baky MA (2004) Mammographic and sonographic features of tuberculous mastitis. European Journal of Radiology. 51(1): 54-60.