Jaber Abdulwahab Asiri1*, Mohammed Abdullah Alshehri1, Rami Abdullah Alghamdi1, Mohahmmed Hadi Alarjani1, Ali Saeed Alaskar1, Nahed AL Fawaz1, Shahad Alrasheed1
1Nuclear Medicine Unit/ Radiology and Medical Imaging, King Saud Medical City, Ulaishah, Riyadh 12746, Saudi Arabia
*Corresponding Author: Jaber Abdulwahab Asiri, Nuclear Medicine Unit/ Radiology and Medical Imaging, King Saud Medical City, Ulaishah, Riyadh 12746, Saudi Arabia
Abstract
A four-year-old female pediatric patient was complaining of back pain, along with fatigue. The parents noticed a small mass in the right abdominal region. The lab results showed elevated inflammatory markers and AST. Also, a KUB ultrasound and abdomen CT were ordered. According to the CT and U/S, besides the patient’s symptoms, neuroblastoma is highly suggestive. I-123 MIBG was ordered to rule out neuroblastoma. Additionally, the patient had Tc99m MDP bone scan to rule out bone metastasis. The patient started 1 cycle of chemo combination of different chemotherapy drugs. MIBG scan was ordered to see the improvement of the chemo treatment. The second MIBG scan showed improvement of metastatic diseases.
Keywords: MIBG, Neuroblastoma, pediatric, Metastases
Introduction
Neuroblastoma is a kind of cancer that is created from the nerve cells, yet which originates in the adrenal gland. In addition, neuroblastoma is very common in children, especially newborns. Also, this type of cancer represents the second most common tumor in childhood [1]. Unfortunately, there are more than 600 children every year to be diagnosed with this cancer annually in the United States [2]. Around 70 % of neuroblastoma cases have metastatic disease [3]. Usually, MRI and CT will be performed initially to diagnose neuroblastoma; however, there is no proof that CT and MRI can confirm neuroblastoma. CT scan has the advantageof evaluating calcification which is one of signs of neuroblastoma and which is a solid heterogeneousmass that contains calcification [4]. I-123 MIBG is superior in diagnosing neuroblastoma. In addition, it more accurate, especially with the curie scoring technique [5].
Case presentation
A four-year-old female pediatric patient was complaining of pain in the back bones, along with fatigue. Also, she was experiencing seizures. For the seizures, a brain MRI was ordered, which came out normal. The parent noticed a small mass in the right abdominal region. The lab results showed elevated inflammatory markers and AST. Also, a KUB ultrasound and abdomen CT were ordered. The sonographer and the CT report found a large mass in the right suprarenal area with partial calcification. In addition, the mass measures were 5.4 * 7.2 * 6.3 cm. CT report said the right adrenal gland was not visualized (Figure 1).

Figure 1: An axial CT scan showed a large mass in the right suprarenal area with partially calcified. B ultrasound showed mass in the right suprarenal area the mass measures were 5.4 * 7.2 * 6.3 cm. the right adrenal gland is not visualized.
According to the CT and U/S, besides the patient’s symptoms, neuroblastoma is highly suggestive. I-123 MIBG was ordered to rule out neuroblastoma. The protocol was to give the patient 4 drops of strong Iodine lugols which were diluted in a cup of water to block the thyroid gland. After one hour, the patient was ready for the MIBG dose. A low iodine diet was required. After 24 hours, the patient came to the department. The acquired images were whole body planar, regional images of the chest, abdomen, and pelvis. The patient position was supine feet first (Figure 2). Additionally, the patient had Tc99m MDP bone scan to rule out bone metastasis (Figure 3).
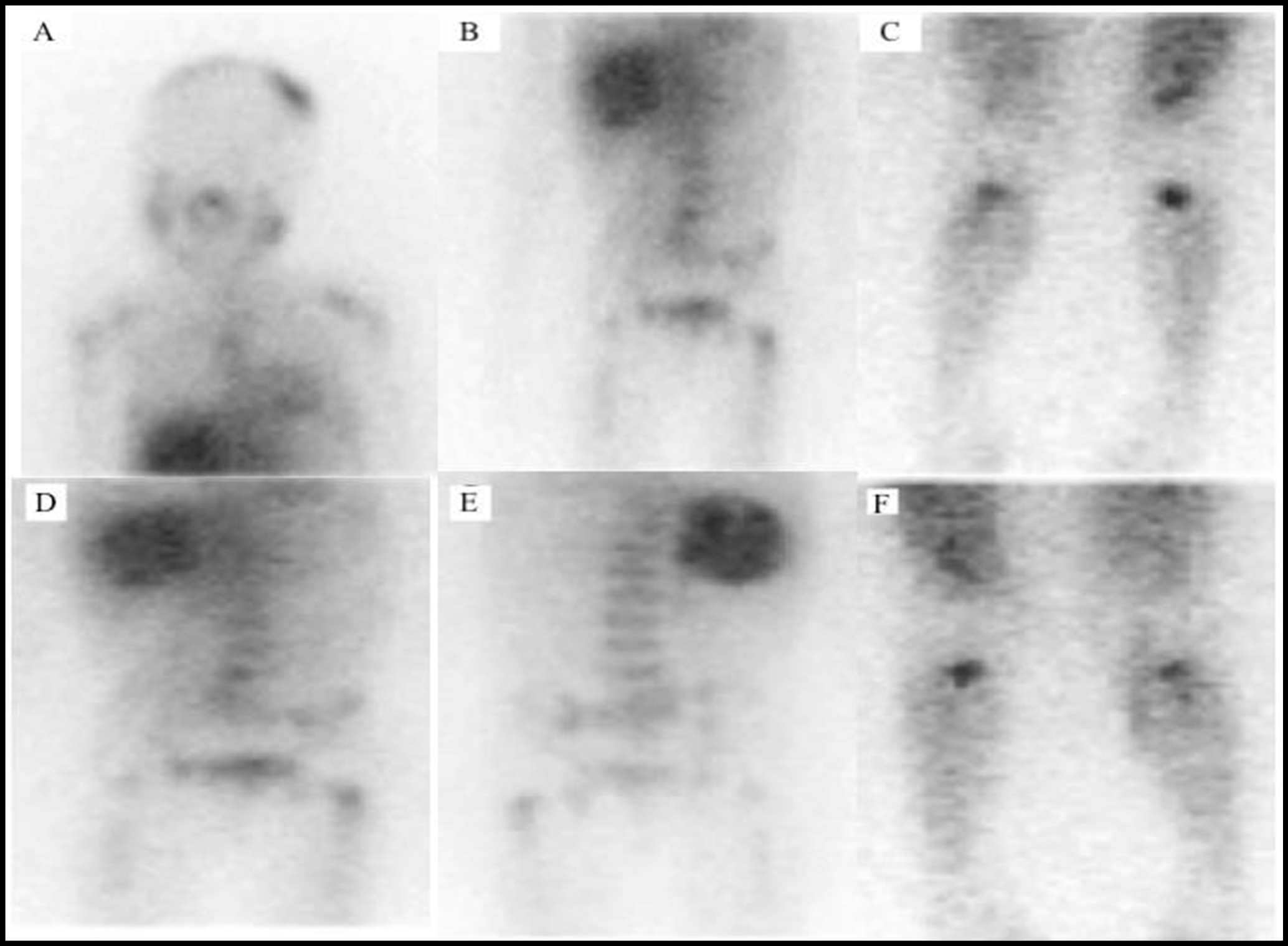
Figure 2: I-123 MIBG planar views. B, D and E intensely increased MIBG uptake within the right suprarenal mass corresponding to the patient’s known primary tumor. A, there were increasing MIBG uptake within the left calvarium and midline occipital area. C and F. There were increasing MIBG uptake in the left proximal femur, and bilateral proximal tibia. Also, there are metastatic lesions within the spin are not well visualized on MIBG imaging E.
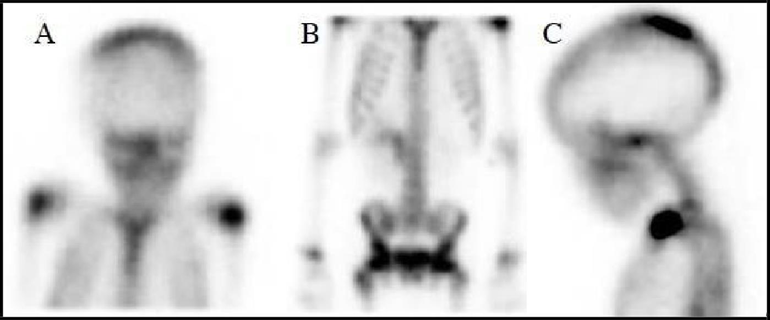
Figure 3: Tc99m MDP. planar views. The patient received an intervenors dose of 4.5 mCi of Tc-99m MDP. The stander dose is 300uCi/kg, and the patient weight is 15 kg. Finding of MDP bone scan, osseous lesion is seen within the left side of the calvarium, more prominently near the vertex A and C, as well as possibly in the high right parietal region, within the thoracic and mid lumbar spine B. In addition, there was uptake in the right sacroiliac joint. There are increasing activity along the occipital potion of the calvarium. There was accumulation of the radiotracer within the soft tissues of the right mid and upper abdomen B.
The patient started 1 cycle of chemo combination of different chemotherapy drugs: cyclophosphamide D1-5, neoplasia D6 and topotecon. During the chemotherapy, the patient was experimenting most chemotherapy side effects. For example, hair loss, less ability to eat or loss of appetite, and vomiting. For this reason, the doctors decided to start a GI tube, as well as a pic line to make the injection much easier since the patient was pediatric. After one month from the first chemo, MIBG scan was ordered to see the improvement of the chemo treatment. The patient was administered lugols to block the thyroid. After one hour, the patient received 2.5 mci of I-123 MIBG. On the second day, there was a 24-hour imaging (Figure 4).
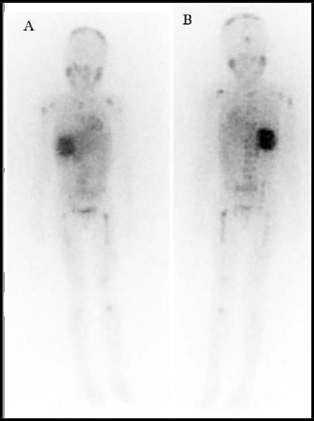
Figure 4: I-123 MIBG whole body, A anterior view B. posterior view there are areas of interval improvement of metastatic diseases especially within the thoracolumbar spine, left calvarium and occipital bone. In addition, an interval reduction in central photopenia within the right abdominal mass is of uncertain etiology.
Conclusion
In conclusion, neuroblastoma is a type of cancer that can affect the pediatric patient from newborn until the age of five. The symptoms of this disease are varied. However, the most common symptoms are fatigue, bone pain, and adrenal gland issue. MIBG I-123 helps us find the bone metastatic that MDB shows as well. The patient had surgery to remove the mass before the chemotherapy. Also, the patient’s health is improving on different levels. According to the parent, the patient is eating better and is more active than before. After the second chemotherapy, the patient doctor’s decided to continue the therapy plan for four weeks and do a third MIBG to see the staging.
References
- Cheung NK, Dyer MA (2013) Neuroblastoma: developmental biology, cancer genomics and immunotherapy. Nat Rev Cancer. 13(6): 397-411.
- Esiashvili N, Anderson C, Katzenstein HM (2009) Neuroblastoma. Current Problems in Cancer. 33(6): 333-360.
- Cheung NK, Zhang J, Lu C, Parker M, Bahrami A, et al. (2012) Association of age at diagnosis and genetic mutations in patients with neuroblastoma. JAMA. 307(10): 1062-1071.
- Swift CC, Eklund MJ, Kraveka JM, Alazraki AL (2018) Updates in Diagnosis, Management, and Treatment of Neuroblastoma. RadioGraphics. 38(2): 566-580.
- Yanik GA, Parisi MT, Shulkin BL, Naranjo A, Kreissman SG, et al. (2013) Semiquantitative mIBG scoring as a prognostic indicator in patients with stage 4 neuroblastoma: a report from the Children's oncology group. J Nucl Med. 54(4): 541-548.



