PGRIS Welagedara1, AP Anand1, Dahanayake M2, PI Jayasekera1*
1Department of Mycology, Medical Research Institute, Colombo, Sri Lanka
2District General Hospital, Monaragala, Sri Lanka
*Corresponding Author: PI Jayasekera, Department of Mycology, Medical Research Institute, Colombo, Sri Lanka.
Introduction
Basidiobolomycosis is an uncommon subcutaneous fungal infection caused by Basidiobolus ranarum which is a saprophytic fungus thought to be transmitted by implantation via minor trauma which often goes unnoticed [1]. It is commonly encountered in children and adolescents and usual sites involved are buttocks and thighs [2,3]. However atypical presentations may occur.
Case History
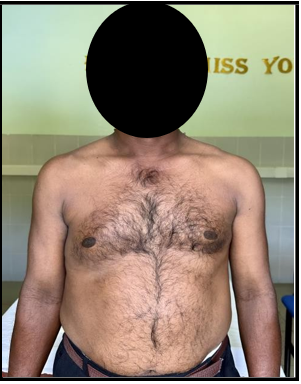
A 48-year-old paddy farmer from rural Sri Lanka (Monaragala) presented with a swelling in the right side of the chest wall for two years’ duration. He was otherwise healthy without any co- morbidities.
The swelling has gradually increased in size over the period and extended to the right anterior and posterior chest wall and crossed over to the midline to the left side of the chest wall (figure 01). It appeared as if he is wearing a “Body Armour” considering the sites involved. It resulted in marked disfigurement. Overlying skin was almost normal, non-pruritic and non-tender, but consistency was woody hard. However, due to the large area of swelling, he experienced significant limitation of chest movements and pain with chest wall movements.
He was unable to recall a history of insect bite over the involved area and there is no history of trauma. There was on and off low-grade fever during the past two years and he developed chills with rigors and evening pyrexia over last six weeks.
Physical examination revealed no abnormality other than the skin lesion. Considering the clinical picture, differential diagnosis included subcutaneous panniculitis like T cell lymphoma, Morphea profundus, subcutaneous infestation/infection (parasitic or fungal), sarcoidosis, tuberculosis and lymphoma.
He underwent several imaging studies including MRI chest, which revealed right sided chest wall soft tissue edema involving adjacent right serratus anterior and lattissmus dorsi muscles with focal area of subacute haematoma/necrotic area.
First true cut biopsy of the lesion was reported as compatible with acute on chronic abscess or foreign body reaction with granuloma formation. A second true cut biopsy was done seven months after the first one and it stated granulomatous inflammation probably foreign body giant cell reaction or tuberculosis.
Tuberculosis was excluded with negative Mantoux test, normal chest X ray, negative TB PCR of true cut biopsy and a trial of ant-TB medication given for one-month duration with no response.
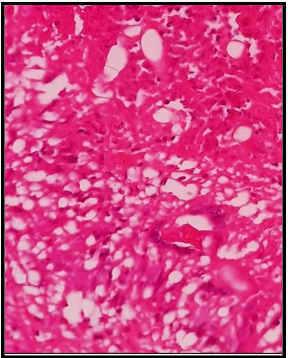
The lesion has extended over to the abdomen and axillary lymph nodes were enlarged and the patient underwent third true cut biopsy from suspicious lymph node and skin lesion. Hematoxylin and eosin (H & E) stain showed epithelioid granuloma with broad, aseptate fungal hyphae in the centre (figure 02). There are no confluent granulomas with central caseous type necrosis. Histology report was concluded as “Subcutaneous fibro-adipose tissue with suppurative granulomatous inflammation caused by a broad, aseptate fungus. Periodic acid-Schiff (PAS) stain showed broad, aseptate hyphae surrounded by bright eosinophilic material with a background of dense eosinophilic infiltrate “Splendore–Hoeppli” phenomenon. Grocott’s methenamine silver stain also became positive for fungal elements.
Fresh biopsy sample was sent to Department of Mycology at Medical Research Institute, Colombo for fungal studies. Direct microscopy performed with 10% potassium hydroxide revealed fungal filaments and fungal culture was done on Sabouraud dextrose agar at 26 °C and 37 °C. After ten days of incubation, it showed creamy white, heaped up and furrowed colonies which was identified as Basidiobolus ranarum morphologically (Figure 03).
Diagnosis of basidiobolomycosis was confirmed based on clinical features, histopathology and culture findings.
Patient was started on itraconazole 200mg twice daily after doing baseline liver function tests.
Patient very well responded to antifungal treatment and the lesion started to shrink within few weeks (figure 04). He was advised to continue itraconazole until one month after complete disappearance of the lesion and follow up with AST and ALT and other liver function tests.
Figure 01: skin lesion on presentation
Figure 02: H and E stain of biopsy
Figure 03: Basidiobolus ranarum culture
Figure 04: treatment response
Discussion
Basidiobolomycosis usually seen in children and adolescents and the sites of lesion are usually lower limbs and buttocks (2). Therefore, this is an unusual site of infection and the diagnosis may be easily missed unless specimens are collected appropriately to make a tissue diagnosis. In atypical presentations as in this case, repeat biopsy may be required. Still, it is very important to obtain repeated specimens until the definitive diagnosis is made. Then unnecessary treatment and complications can be avoided.
References