Sebastião David Santos-Filho*
Biophysics, Biosciences Department, Universidade Federal do Rio Grande do Norte, Natal, RN, Brasil.
*Corresponding Author: Sebastião David Santos-Filho, Biophysics, Biosciences Department, Universidade Federal do Rio Grande do Norte, Natal, RN, Brasil.
Abstract
Introduction: The hope that the advance of medicine propitiates the treatment of chronic diseases such as diabetes mellitus is the principal dream of the entire world. Diabetes Mellitus is one of those diseases that affect many individuals around the world with different types of manifestation according to the nature of someone and the inability to escape the consequences in the future. Treatment forms were developed trying to break the evolution of diabetes, but some of them still inefficacy or make the disease increase.
Objective: In the tentative to explain these phenomena, this research was done in PubMed to find articles that have an explanation or a way of treating this disease.
Methods: The search was done using the terms elderly, blood, disorder, Diabetes Mellitus, and drug treatment, searching the last 5 years, clinical study, free full text, done in humans and written in English. All the articles had associated data.
Results: It was founded 297 articles. 14 papers were established using Canagliflozin to treat diabetes, 13 using Dapagliflozin, and 10 using Ertugliflozin, a total of 68 reports. Metformin was cited in 9 works.
Conclusion: The use of Empagliflozin or Canagliflozin to treat diabetes mellitus has clinical evidence proving that these medicines are helpful to prevent other disturbs that come with it.
Keywords: Elderly; Blood; Disease; Diabetes Mellitus; Drug Treatment.
Introduction
The increase in the world population free of diseases is due to the advance of medicine in treating diverse types of ills that affect people [1]. Diseases of the blood, such as diabetes, are of some importance in product people going to hospital and some without a specific cure [2]. Diabetes Mellitus is one of those diseases that affect many individuals around the world with different types of manifestation according to the nature of someone and the inability to escape the consequences in the future [1,2].
The prevalence of diabetes around the world has reached epidemic proportions. The International Diabetes Federation estimated that 537 million people will be living with diabetes in 2021. This number is expected to increase to 784 million by 2045 [3].
Treatment forms were developed to break the evolution of diabetes, but some of them still inefficacy or make the disease not increase [4]. Using some drugs designed to maintain the glycemic level in acceptable values is practical for the success of treating this disease [5,6].
Trying to search for explanations of these phenomena, this work was done by searching the databank known as PubMed for articles that cite some drugs used and that have good ideas about what happens with the patients.
Methodology
The search was done in PubMed (https://pubmed.ncbi.nlm.nih.gov) on 20/02/2023 using the terms: elderly, blood, disease, Diabetes Mellitus and drug treatment, searching the last 5 years, clinical study, free full text, done in humans and written in English. All the articles had associated data.
Results
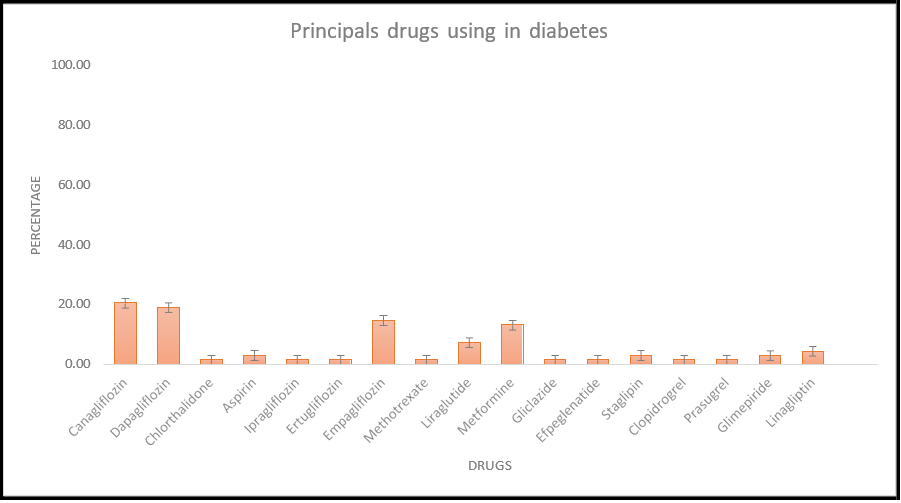
Initially, 297 articles attended the requisites. It tried to separate only the articles that treat the disease by using drugs, synthetic or not. Were founded 14 articles using Canagliflozin to treat diabetes, 13 using Dapagliflozin, and 10 using Ertugliflozin, a total of 68 articles. Metformin, the most drug used in Brazil, was cited in 9 works (13.24%). Another type of drug and treatment that was mentioned once reached 8 works. Another type of treatment was 2 to 5 citations not used in this work. Those results are summarized in Figure 1 and Table 1.
Figure 1: Principals drugs using to treat diabetes
Table 1: Number of citations (prevalence) of the principals’ drugs using to treat diabetes obtained in this research.
|
Canagliflozin |
14 |
|
Dapagliflozin |
13 |
|
Chlorthalidone |
1 |
|
Aspirin |
2 |
|
Ipragliflozin |
1 |
|
Ertugliflozin |
1 |
|
Empagliflozin |
10 |
|
Methotrexate |
1 |
|
Liraglutide |
5 |
|
Metformin |
9 |
|
Gliclazide |
1 |
|
Efpeglenatide |
1 |
|
Sitagliptin |
2 |
|
Clopidogrel |
1 |
|
Prasugrel |
1 |
|
Glimepiride |
2 |
|
Linagliptin |
3 |
All the results were analysed and studied to make this work and compared to other articles that searched the same comparison to understand the diabetes treatment used in our days.
Discussion
Diabetes in all types cited in the literature is a health problem to be solved worldwide [1,2]. This disease affects blood circulation, kidney function, hepatic function, and brain function, provoking damage in all these systems [7,8]. It is a metabolic disease of origin in the carbohydrate used for the organism to obtain energy for all functions needed. This altered metabolism provokes malcirculation of the blood in the vessels and malnutrition of the body's tissues, also causing alterations in other biochemical processes of the organism essential for surveillance [8,9].
The use of Metformin to treat diabetes has spread in the world, and its effects are well-known. Metformin is a medicine that has no efficiency in prediabetes treatment, but in the last two decades, it has been considered to be used for diabetes prevention [10]. It was surprising to find few works mentioning it (9 citations).
Canagliflozin is the most cited (15 citations) in the articles found because of its association with cardiac outcomes due to diabetes [11]. Cardiovascular problems are evident in patients with diabetes because glucose increase in the blood causes interruptions in the blood flow, giving the patient insufficiency in the cardiac bomb. The canagliflozin acts as a regulator of glucose concentrations and produces a type of cardiac protection [8,11].
The use of other drugs, like Dapagliflozin [12] and Empagliflozin [13], have similar explanations based on their pathophysiological properties.
Empagliflozin's pathophysiological properties have an explanation in acting as a sodium-glucose cotransporter 2 inhibitor, reducing the risk of cardiovascular death or heart failure hospitalization in patients with chronic heart failure [13]. These indicate that initiating empagliflozin in patients hospitalized for acute heart failure is well tolerated and results in significant clinical benefit 90 days after starting treatment. The inhibitors known as SGLT2 have risen to prominence in recent years as type 2 diabetes mellitus medications with favorable effects on cardiovascular and renal outcomes. Canagliflozin is one of all FDA-approved inhibitors that has demonstrated benefits in large-scale placebo-controlled randomized trials of patients with type 2 diabetes mellitus and elevated cardiovascular risk [12].
All these drugs prevent diabetes and cardiovascular complications more efficiently than others, and they will be of choice in treating diabetes patients with cardiovascular outcomes.
Conclusion
The use of Empagliflozin or Canagliflozin to treat diabetes mellitus has clinic evidence that proves that these medicines are of utility to prevent other disturbs that come with it.
Acknowledgments: Thanks to Universidade Federal do Rio Grande do Norte, UFRN, to support this work.
References
- Hajat C, Stein E (2018) The global burden of multiple chronic conditions: a narrative review. Prev Med Rep. 12: 284-293.
- Sapra A, Bhandari P (2023) Diabetes Mellitus. Treasure Island: StatPearls Publishing.
- Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. (2022) KDIGO 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int. 102(5S): S1-S127.
- Presad RB, Groop L (2019) Precision medicine in type 2 diabetes. J Intern Med. 285(1): 40-48.
- Vieira R, Souto SB, Sánchez-López E, Machado AL, Severino P, et al. (2019) Sugar-Lowering drugs for type 2 Diabetes Mellitus and metabolic syndrome-review of classical and new compounds: part-I. Pharmaceuticals (Basel). 12(4): 152.
- Dhatariya K, Corsino L, Umpierrez GE (2020) Management of Diabetes and Hyperglycemia in Hospitalized Patients. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc.; 2000.
- Zhao Q, Yan T, Chopp M, Venkat P, Chen J (2020) Brain-kidney interaction: Renal dysfunction following ischemic stroke. J Cereb Blood Flow Metab. 40(2): 246-262.
- Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, et al. (2020) Pathophysiology of Type 2 Diabetes Mellitus. Int J Mol Sci. 21(17): 6275.
- Daryabor G, Atashzar MR, Kabelitz D, Meri S, Kalantar K (2020) The Effects of Type 2 Diabetes Mellitus on Organ Metabolism and the Immune System. Front Immunol. 11: 1582.
- Moin T, Schmittdiel JA, Flory JH, Yeh J, Karter AJ, et al. (2018) Review of Metformin Use for Type 2 Diabetes Prevention. Am J Prev Med. 55(4): 565–574.
- Sarraju A, Spencer-Bonilla G, Rodriguez F, Mahaffey KW (2021) Canagliflozin and cardiovascular outcomes in Type 2 diabetes. Future Cardiol. 17(1): 39-48.
- Nicholson MK, Ghazal Asswad R, Wilding JP (2021) Dapagliflozin for the treatment of type 2 diabetes mellitus - an update. Expert Opin Pharmacother. 22(17): 2303-2310.
- Voors AA, Angermann CE, Teerlink JR, Collins SP, Kosiborod M, et al. (2022) The SGLT2 inhibitor empagliflozin in patients hospitalized for acute heart failure: a multinational randomized trial. Nat Med. 28(3): 568-574.