Diana Carolina Hennessey-Calderón3*, Silvia María Ortega-Llanes1, Gustavo Alexis Lemus-Barrios2, Lilia Andrea Rojas Garzon3
1Department of Internal Medicine, El Bosque University. Bogotá, Colombia
2Department of Internal Medicine, Hospital Fundación SantaFe. Bogotá, Colombia
3Department of Internal Medicine, National Cancer Institute. Bogota, Colombia
*Corresponding Author: Diana Carolina Hennessey-Calderón, Department of Internal Medicine, National Cancer Institute. Bogota, Colombia.
Abstract
Sialoadenosis refers increase in salivary glands, especially of the parotid, this phenomenon is non-inflammatory and at the same time non- neoplastic. Although there are many causes of sialadenosis, bulimia is one of the most common causes. We present a case of a 30 year old woman that had have a very large inflammation of the parotid glands for the last month; she was being treated with a lot of medications, antibiotic and anti-inflammatory drugs with no response. We discard some other causes like Sjogren’s syndrome, alcoholism, and sarcoidosis and the final diagnosis was sialoadenosis secondary to bulimia nervosa.
Keywords: “Bulimia”, “sialomegaly” “Parotidgland”, “Sialadenosis”, “ Eating disorder.”
Introduction
When we speak of sialoadenosis (sialosis or sialadenosis), it refers increasein salivary glands especially of the parotid, this phenomenon is non-inflammatory and at the same time non-neoplastic. This situation is a systemicmetabolic disorder that in most cases may have an endocrine cause; in that case it is influenced by diabetes mellitus and the different glands such as the pituitary and the thyroid. Dystrophic-metabolic sialoadenosis is related to malnutrition, alcoholism and chronic liver diseases, and the third type of sialoadenosis is neurogenic, where there is an alteration in the vegetative nervous system or by medications [1].
Lavender was one of the first authorsto report the association betweenvarious emetic episodes and the growthof the bilateral parotid associated with the eating disorder of bulimia [2]. The prevalence of bulimiain worldwide for young women varies between 2 and 12% and in university women it can increase up to 19%, the incidence in men in general is between 5% and 10% [3].
This article presentsa case report of parotidsialodenosis associated with long-lasting bulimia, a review of the literature and treatment options for these patients.
Case Report
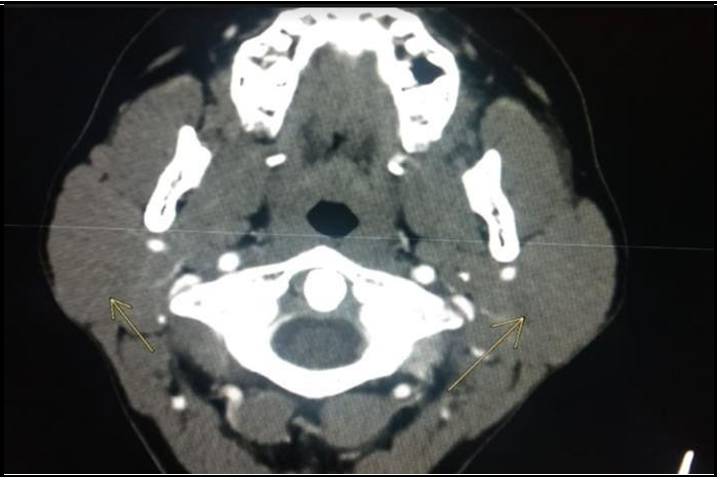
A 30 year old patient, with a history of heavy smoking and Bulimia since the age of 13 without medical follow-up. She was admitted to the hospital due to a clinical history of one month of evolution consisting of edema and bilateral pain in the parotid areas in the lower jaw, she had consultedin 4 health centers and had antibiotic treatment with clindamycin, amoxicillin with clavulanate and had taken enough anti-inflammatories (Ibuprofen and Meloxican) without improvement. Physical examination revealed edema of the parotid that alters the shape of the patient's face (Figure 1). On admission, a neck tomography was taken with clear evidence of the increase in the parotid glands, and it was symmetrical (Figure 2).
During her hospitalstay, several studieswere performed rulingout that the origin was autoimmune, infectious or another cause because the patient in the system review reported dry symptoms, occasional arthralgias and subjective sensation of fever.
Studies of Hepatitis B, Hepatitis C, Human Immunodeficiency Virus(HIV), Cytomegalovirus IGG and IGM, Epstein Barr IGG and IGM, antinuclear antibodies (ANA), neutrophil cytoplasmic antibodies (ANCAs), extractable nuclear antigens (ENAs), rheumatoid factor, and all these studies were negative. Therefore, one month later, it was decided to perform a parotid biopsy without evidence of an inflammatory or neoplastic process in the material examined. The patient was given conservative management with oral pilocarpine and psychotherapy by psychiatry and follow-up is expected to verify efficacy and improvement accordingly redefine management to be followed.
Figure 1: The images show the bilateral growth of the parotids
Figure 2: Neck tomography: Evidence of increased volume of the parotid glands, which appear symmetrical and increased in density, due to known inflammatory changes, with no evidence of collections or intraparotid masses.
Discussion
Bulimia is a disorder in which the person has episodes of anxiety with binges and later compensatory behaviors, such as vomiting, diarrhea or some way that makes the person feel that they are losing weight, also the person has a perspective of their weight and their silhouette different from reality, they usually feel that they have an increase in weight and are not comfortable with their body. The frequency of the episodes for the diagnosis is once a week for a 3-month period [4].
The prevalence of Bulimia is 13% in adolescents between 14 and 24 years old and 1% in the general population. This predominates in women between 20 ± 4.3 years [5]. In bulimia, the medical complications are very varied, involve various systemsand depend due to the mode and frequency of purging [6]. Into this complications include the sialoadenosis.
Sialosis (sialadenosis) is painless, bilateral, diffuse, non- inflammatory, non-neoplastic disease and is generallycharacterized by a great growthnot only of the salivaryglands but also the parotid. [7] Sialosis when the cause is the bulimia can occurs in 10% - 60% of the total bulimicpatients [8]. The pathophysiological of sialomegaly in general is still uncertain, but it has been studied in high carbohydrate diet, the intake of different medications, malnutrition, pancreatic damage, and the repeatedregurgitation of gastric acid [11]. In 1956, Duplessis reported swelling and inflammation of the parotid gland of undernourished patient’s; he proposed that hypertrophy could be involved due to the prolonged stimulation of the salivary glands by an exaggerated esophageal-salivary reflux caused by the underlying esophagitis that malnourished patients have, in the case of bulimic patients present a secondary acidic oral pH to different episodes of vomiting in one day: it is found in patients who induce vomiting at least 1 to 3 emetic episodes per day [9,10], compensated by binge episodes where an increase in salivary flow is generated, causing hypertrophy of the parenchyma of the salivary gland [12].
The diagnosis is usually make with the exclusion of inflammatory etiologies that generate the growth and swelling of the different salivary glands, especially the exclusion of autoimmune disorders such as sjogren, granulomatous causes such as Sarcoidosis and infections like vih, these are the main causesin the general population [13] but there are other differential causes. In general terms, the causes can be classified into infectious and non-infectious origin. In the first group the etiology can be bacterial (mixed flora, Streptococcus pyogenes, Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, Mycobacterial tuberculosis), viral (paramyxovirus, Coxsackie B1 / B6 virus, HIV), parasitic as in the case of the disease Chagas or even fungal. On the other hand, the non- infectious etiology may be due to metabolic processes such as diabetes, hypoparathyroidism, disorders of the hypothalamus, pituitary and adrenal axis, among others. Also nutritional processes such as extreme malnutrition, vitamin deficiency, obesity, excessive intake of starch, cirrhosis. It's also important to highlight the intake of medications such as thiouracil, isoprenaline, dextropropoxyphene, 1st generation contraceptive pill, cytosinearabinoside, ritodrine, rhinograffin, iodide, sulfisoxazole, phenylbutazone, phenyltoin. Should also be considered allergicreactions, toxicity due to iodineor heavy metals, gastrointestinal diseases, neurological dysfunctions and even neoplastic pathologies that do not directlyaffect the parotidgland, such as esophageal carcinoma or melanoma.
To complement the diagnosis, additional studies with computed tomography can be performed, where normally it only shows the enlargement of the glands without specific characteristics and the aspiration biopsy its other way that can help in the diagnosis, but they are not common to be done [7].
Management of the pathology is based on the etiologythat is generating the syndrome depends on identifying the underlying cause that needs to be corrected [7]. In the cases of patients with bulimia, certain common treatments may not work like the sialogogues in the form of sour caramel, local application of heat, and abundant liquids [14]; as pharmacological management, high doses of pilocarpine hydrochloride may help (5 to 15 mg/day). It is described in some studies as an adequate treatment, but the results are generally poor [15]. Other therapies, such as glandular chemo denervation with botulinum toxin injections or infusion of triamcinolone, have now been proposed, although their efficacy has not been proven [14].
Surgery can be considered as a last resort to improve the aesthetics of the patient [7]. For the psychological part of these bulimic patients, it is important to continue management with psychiatry with cognitive- behavioral therapy in order to reduce emetic episodes and achieve resolution of eating disorders and thus of chronic inflammation of the salivary glands.
Conclusion
Sialadenosis consisting of the growth and swelling of the salivary glands including the parotid and despite the fact that there are various causes, infectious, metabolic, bulimia is one of the most common causes that must be taken into account within the differential diagnosis.
References
- Garcia B, Dean Ferrer A, Diaz Jimenez N, Alamillos Granados FJ (2018) Bilateral Parotid Sialadenosis Associated with Long- Standing Bulimia: A Case Report and Literature Review. J Maxillofac Oral Surg. 17(2): 117-121.
- Lavender S (1969) Vomiting and parotid enlargement. Lancet. 1(7591): 426.
- Mandel L, Kaynar A (1992) Bulimia and Parotid Swelling: A Review and Case Report. J Oral Maxillofac Surg. 50(10): 1122- 1125.
- Wade TD (2019) Recent Research on Bulimia Nervosa. Psychiatr Clin North Am. 42(1): 21-32.
- Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, et al. (2013) The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 73(9): 904-914.
- Westmoreland P, Krantz MJ, Mehler PS (2016) Medical Complications of Anorexia Nervosa and Bulimia. Am J Med. 129(1): 30-37.
- Scully C, Eveson J (2004) Sialosis and necrotizing sialometaplasia in bulimia; a case report. Int. J. Oral Maxillofac Surg. 33(8): 808–810.
- Ogren FP, Huerter JV, Pearson PH, Antonson CW, Moore GF (1987) Transient salivary gland hypertrophy in bulimics.Laryngoscope 97(8 pt 1): 951–953.
- Coleman H, Altini M, Nayler S, Richards A (1998) Sialadenosis: a presenting sign in bulimia. Head Neck. 20(8): 758–762.
- Mignogna M.D, Fedele S, Lo Russo L (2004) Anorexia/bulimia‐ related sialadenosis of palatal minor salivary glands. Journal of Oral Pathology & Medicine. 33(7): 441-442.
- Levin PA, Falko JM, Dixon K, Gallup EM, Saunders W (1980) Benign parotid enlargement in bulimia. Ann Intern Med. 93(6): 827-829.
- Buchanan JA, Fortune F (1994) Bilateral parotid enlargement as a presenting feature of bulimia nervosa in a post-adolescent male. Postgrad Med J. 70(819): 27-30.
- Du Plessis DJ (1956) Parotid enlargement in malnutrition. S Afr Med J. 30(30): 700-703.
- Benedek-Spät E, Puskás M, Rajki J (1980) Electrophoretic protein pattern of human parotid saliva in Sjögren's syndrome and sialosis. Acta Otolaryngol. 90(3- 4): 275-282.
- Mehler PS, Wallace JA (1993) Sialadenosis in bulimia. A new treatment. Arch Otolaryngol Head Neck Surg. 119(7): 787-788.
- Nassour DN, Patel SV, Kosseifi SG, Jordan RM, Peiris AN (2007) Marked bilateral parotid enlargement in metabolic syndrome: a case report and review of the literature. Tenn Med. 100(1): 39-41.