Fatimah Al Muqarrab, MBBS1*, Zahraa Al Muqarrab, MBBS2, Mohammed Almosbeh, MBBS3
1King Fahad Hospital, Hofuf, Saudi Board of Dermatology, Postal code: 36348
2King Faisal University, Ahsaa, Medical student
3King Fahad Hospital- Hofuf, Saudi Board of General surgery
*Corresponding Author: Fatimah Al Muqarrab, MBBS, King Fahad Hospital, Hofuf, Saudi Board of dermatology, Postal code: 36348
Abstract
Herpes zoster infection represents a localized reactivation state of latent varicella-zoster virus. Zoster presents as a grouped vesicular rash on an erythematous base distributed over sensory dermatomes. Disseminated zoster is defined as the presence of >20 vesicles outside the primary area or adjacent dermatomes. Atypical manifestations of zoster infection, especially in immunocompromised patients, may lead to delayed diagnosis, complication; however, more serious deep soft tissue infection is not. infection dissemination, and potentially life-threatening systemic complications. Bacterial superinfection of zoster lesions is a common.
Here we present two atypical cases of zoster infection, which needed a high index of suspicion to avoid misdiagnosis and inappropriate treatment. Our first patient is a 30-year-old Saudi male, with systemic lupus erythematosus on oral steroids who presented with a tense vesiculobullous eruption over two adjacent dermatomes. Biopsy revealed herpes infection. The second case is for a 58-year-old diabetic female who presented to the emergency department for evaluation of an extremely painful eruption in a dermatomal distribution one week after zoster resolution. Clinical and radiologic evaluation of the lesions identified necrotizing fasciitis. Although zoster commonly affects immunocompromised individuals, the atypical presentation of the initial lesions in our two patients was challenging. A high index of suspicion is required for early detection, with special consideration of the painful lesion in a cropped configuration.
Introduction
Herpes zoster infection represents a localized reactivation state of latent varicella-zoster virus. Zoster is more common and clinically severe during adulthood. Unusual presentations and serious complications can develop in immunocompromised individuals with a high risk of mortality if the diagnosis is delayed or treatment is not performed. [1]
This series highlights the need for a high index of suspicious and the importance of early detection of zoster infection to avoid serious complications in immunocompromised patients.
Case Reports:
Case 1
A 30-year-old Saudi male patient had a long-term history of systemic lupus erythematosus treated with low-dose oral prednisone. One month before the presentation, he was diagnosed as having lupus nephritis progressing to end-stage renal disease, for which he received hemodialysis plus oral prednisone 1 mg/(kg·day). Shortly thereafter, he developed a localized tense bullous eruption on an erythematous base over the medial aspects of the right foot and arm (Figure 1). Owing to the initial distribution and tense nature of the blisters, biopsies were taken for hematoxylin-eosin staining and immunofluorescence. The initial differential diagnostic impression was bullous lupus erythematosus, bullous disease of dialysis, bullous pemphigoid, and linear IgA bullous dermatosis.
Figure 1 a, b: Clinical photo of the right foot, There are inflammatory tense bullous lesions confined to the medial right foot.
Over the next few days, the bullous eruption extended to involve the anterior, medial, and lateral aspects of the ipsilateral leg over two adjacent dermatomes (L4 and L5) with a confluent and annular configuration of the lesions (Figure 2). The right arm lesions involved the volar forearm in a linear confluent distribution over the T1 dermatome. At that time, the Tzanck smear was negative, and administration of the empirical renal adjusted dose of IV acyclovir was initiated under the impression of disseminated bullous zoster.
Figure 2 a, b: Clinical photo to the right lower limb, there are confluent tense bullae extending over L4-L5 dermatomes.
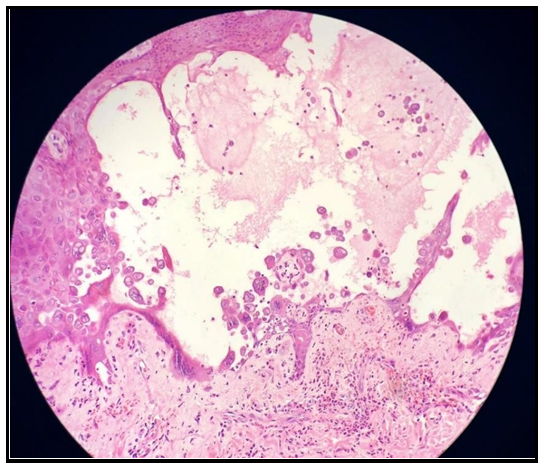
The biopsy specimen from a new fresh blister showed a suprabasal bulla with acantholysis and marked ballooning degeneration of keratinocytes, multinucleated cells, and peripheral chromatin clumping along with superficial perivascular neutrophilic infiltrates, consistent with herpes infection (Figure 3). The IgG direct immunofluorescence for immune-blistering disorders was negative and thus revealed no inflammatory autoimmune disorders. After a week of acyclovir therapy, most lesions had dried up. (Figure 4)
Figure 3: Histopathologic photo (H&E), There is a large supra-basal cleft with acantholysis. Multinucleated cells and chromatin margination. Superficial perivascular neutrophilic infiltrates.
Figure 4: clinical photo of the right lower limb most of the bullous lesions has been dried up after acyclovir course.
Case 2
A 58-year-old diabetic female patient presented to the emergency department with a febrile illness one week after resolution of cutaneous herpes zoster, along with an extremely painful upper back skin lesion.
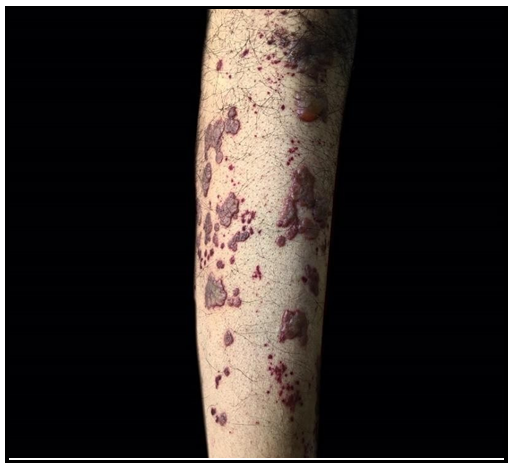
Upon examination, the patient looked ill, febrile, and had dusky, erythematous-to-violaceous, ill-defined, tender warm patches over the upper right side of the back. The patches extended along with the dermatomal distribution, encircling the right hemithorax associated with the superimposed yellowish crusted, violaceous bordered erosions, in addition to the post-inflammatory hyperpigmentation of the resolved zoster. The initial provisional diagnosis was herpes zoster complicated by necrotizing fasciitis (Figure 5 a,b.).
Figure 5 a, b: Clinical photo of the back There are ill-defined violaceous-erythematous patches over dermatomal distribution (T2) with superimposed crusted ulcers.
Urgent ultrasonography revealed soft tissue edema with multiple small subcutaneous fluid collections. Consequently, she was admitted under surgical care and underwent a surgical debridement for the extensive necrotizing soft tissue infection. She received an IV piperacillin/tazobactam, metronidazole, and vancomycin, oral valacyclovir at 1 g/day for 10 days, and intensive supportive care.
Discussion
Bullous herpes zoster is rare. [2,3,4,5,6] The risk factors include alcoholism and systemic malignancy, immunosuppressives, and corticosteroid use. One reported patient was without any predisposing conditions. (Table 1)
Table 1: Comparison of six cases of bullous zoster.
|
|
Case 1 |
Case 2 |
Case3 |
Case 4 |
Case 5 |
Case 6 (present) |
|
Age (yrs)/Gender |
13/F |
3.5/F |
58/M |
56/M |
94/F |
30/M |
|
Immune status |
Immuno-compromised |
Immuno-compromised |
- |
Immuno- competent |
Immuno- compromised |
Immuno- compromised |
|
General risk factors |
Juvenile idiopathic arthritis on prednisolone + anakinra. |
Acute lymphoblastic leukemia on vincristine, doxorubicin, dexamethasone and L- asparaginase |
Alcoholic liver cirrhosis |
Healthy |
Elderly |
SLE on high dose prednisone |
|
Skin lesions localization (dermatome) |
C2-4 |
C6, C7 and T1 |
L2 |
T4 |
C4-7 |
L4-5 and T1 |
|
Diagnostic test |
PCR from the blood and bullous fluid |
PCR of the bullous fluid |
Tzank smear |
Tzank smear |
Histo- pathology, viral PCR |
Histo- pathology |
|
Co-infection |
Staphylo-coccus aureus |
None |
None |
None |
None |
None |
|
Treatment |
IV flucloxacillin and acyclovir changed to foscarent |
IV acyclovir for 10 days followed by oral acyclovir for 5 days |
Acyclovir |
- |
Valcyclovir 1 gram daily for 7 days |
IV acyclovir (renal adjusted dose) |
|
Outcome |
Resolved |
Resolved |
Unknown |
Resolved |
Resolved |
Resolved |
Atypical manifestations of zoster, especially in immunocompromised patients, may lead to delayed diagnosis, disseminated disease, and potentially life-threatening systemic complications. Disseminated zoster, defined as the presence of > 20 vesicles outside the primary area or adjacent dermatomes, affects approximately 10 % of immunocompromised persons with zoster. [1] The prevalence of dissemination was much higher in immunocompromised bullous zoster cases. Prompt administration of IV acyclovir helps prevent visceral dissemination. [7]
Bullous herpes zoster should be distinguished from blistering disorders, including immune-mediated subepidermal bullous dermatosis. In our patients, the medical history of lupus erythematosus was misleading, especially in the setting of the very early localized presentation to the acral site.
One report described bullous zoster associated with an increased titer of 180 anti-BP autoantibodies during an active infection, which subsequently declined after valacyclovir therapy initiation. This is another explanation for the unusual tense nature of the bullae. [2] Bacterial superinfection is a relatively common complication of herpes zoster. However, bacterial cellulitis, the more serious complication of zoster infection, is rare, and necrotizing fasciitis is rarer. [7] Necrotizing fasciitis is surgically challenging, with a relatively poor prognosis if not diagnosed and treated properly early in its course. It usually presents as pale-red edematous skin that is severely painful and progresses rapidly to cyanotic erythema and, if not treated, to frank gangrene. It involves the extremities, abdominal wall, groin, and, rarely, the head and neck region, and upper back. [9,10] Of the 5 reported cases of zoster gangrenosum, 2 affected the trunk, and 3 were distributed over the periorbital skin. The immunodeficiency status of our patient might have contributed to the rare complication, as in previously reported cases, of which some were immunocompetent. [10]
Although zoster commonly affects immunocompromised individuals, the atypical presentation of the initial lesions in our two patients was challenging. A high index of suspicion is required for early detection, with special consideration of the painful lesion in a cropped configuration.
Funding sources: None
Conflicts of Interest: None declared.
References
- Bolognia JL, Schaffer JV, Cerroni L (2017) Dermatology. 4th ed. London, UK: Elsevier health sciences.
- Kamiya K, Aoyama Y, Suzuki T, Niwa H, Horio A, et al. (2016) Possible enhancement of BP180 autoantibody production by herpes zoster. Journal of Dermatology. 43(2): 197–199.
- Ponce-Olivera RM, Tirado-Sânchez A, Díaz-Molina VL. Bullous and hemorrhagic herpes zoster. Dermatología Rev Mex 2012; 56 (6): 414-417.
- Wong KJ, Osowicki J, Seaby E, Curtis N, Gwee A (2014) Bullous herpes zoster. J Pediatr. 164(3): 667.
- Haimi M, Ben-Arush MW, Kassis I, Postovsky S, Kra-Oz Z, et al. (2004) Bullous herpes zoster in a child with leukemia: case report and review of the literature. J Pediatr Hematol Oncol. 26(9): 587- 90.
- Veraldi S, Carrera C, Gianotti R, Caputo R (2000) Bullous herpes zoster. Acta Derm Venereol. 80(1): 55.
- Mandal B K (2006) Herpes zoster in the immunocompromized populations. Indian J Dermatol. 51(4): 235-243.
- Maureen B Poh-Fitzpatrick. (2017) Bullous Disease of Dialysis Treatment & Management. Medscape.
- Sadasivan J, Maroju NK, Balasubramaniam A (2013) Necrotizing Fasciitis. Indian J Plast Surg. 46(3): 472-478.
- Cozzupoli GM, Gui D, Cozza V, Lodoli C, Pennisi MA, et al. (2019) “Necrotizing Fasciitis Following Herpes Zoster Ophthalmicus in an Immunocompromised Patient,” Case Reports in Ophthalmological Medicine. 2019: 4534153.