Filippo Montali1*, Erika Boriani2, Bettoni Stefania2, Alfredo Annichiarico1,2, Edoardo Virgilio1,2, Renato Costi1,2
1Department of Surgery, Azienda Sanitaria Locale di Parma, Vaio Hospital, Via Don Tincati 5, 43036 Fidenza (PR), Italy
2Department of Medicine and Surgery, University of Parma, Via Gramsci 14, 43123, Parma
*Corresponding Author: Filippo Montali, Department of Surgery, Azienda Sanitaria Locale di Parma, Vaio Hospital, Via Don Tincati 5, 43036 Fidenza (PR), Italy.
Abstract
Appendicular torsion (AT) is a rare disorder often diagnosed intra-operatively during a diagnostic laparoscopy (DL). AT is hardly detected by pre-operative radiologic investigations such as abdominal ultrasound (US). The anticlockwise torsion can completely obstruct the appendicular lumen compromising blood supply and leading to strangulation, venous infarction, and bacterial translocation. Clinical presentation is undistin- guishable from acute appendicitis and must be included in the differential diagnosis of patients with right lower quadrant abdominal pain (RLQAP). Herein we report a rare case of a 24-year-old female with a 200-degree clockwise primary rotation of the retro-cecal appendix, and we offer a review of the pertinent literature.
Keywords: appendix, torsion, clockwise, emergency surgery.
Introduction
Appendicular torsion (AT) is a rare condition, often diagnosed in-traoperatively and clinically indistinguishable from acute appendici- tis, one of the most typical causes of urgent surgery [1]. AT can be primitive (or idiopathic) when related to specific anatomical features such as a lengthy appendix, a fan‐shaped mesoappendix with a narrow base, or the absence of azygotic folds, which usually fix the appendix laterally [2,3]. Secondary forms of AT occur when the twist is after other pathological conditions like coprolith impaction, mucocele, car- cinoid tumor, mesoappendiceal lipoma, foreign bodies, or lymphade- nitis [4,5]. AT symptoms usually mimic the ones associated with acute appendicitis: abdominal pain in the right iliac fossa, nausea, and vomiting. Consequently, AT should be included in the differential di-agnosis of patients with right lower quadrant abdominal pain (RLQAP). Some findings on pre-operative radiologic imaging could suggest the presence of a torsion - particularly the secondary forms of AT - but abdominal US is not the gold standard to detect. An ab-dominal CT scan is undoubtedly a more sensitive examination, but it is not always performed in the preoperative workup. For all these rea-sons, AT is most frequently diagnosed during a diagnostic laparos-copy (DL) [6].
Case Report
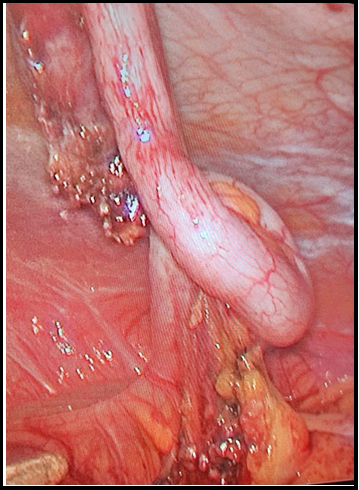
A 24-year-old woman presented to the emergency department com- plaining of a 3-day history of colicky pain in the right iliac fossa, an- orexia, and vomiting. There was no significant record in her past med- ical history. A physical examination of the abdomen revealed pain localized in the right iliac fossa and distention, guarding, and rebound tenderness. Blood tests showed a total leucocyte count of 15,300/mm and a C-reactive protein level of 0.08 mg/dL. The first bedside ultra- sonography did not detect any clear signs of appendichopathy. After an unremarkable gynecological consultation, a second US was exe- cuted after 24 hours, showing an amount of collection in the right iliac fossa with local lymphadenitis. An emergency appendectomy with a laparoscopic approach was performed. Intraoperatively, there was ev- idence of torsion of the vermiform appendix with a clockwise rotation of 200 degrees around 1 cm from the base of the appendix (Figure 1). The appendix appeared retrocausal, long, and congested. The mesen-tery was short compared to the length of the appendix. Some adhe- sions were present between the appendix and the surrounding tissues. We finally proceeded to remove the appendix. Histopathology con- firmed the AT diagnosis: a luminal dilatation was found distally to the torsion site, and the appendicular wall had already developed ne- crosis. The appendix measured 9.5 cm in length. The postoperative course was uneventful, and the patient was discharged on the fourth postoperative day.
Figure 1: Evidence of torsion of the vermiform appendix with a clockwise rotation of 200 degrees around 1 cm from the base of the appendix
Discussion
Paralleling appendicular neuralgia or Amyand’s hernia, appendicular torsion (AT) represents an unusual appendix disease in emergency surgery. AT clinically mimics acute appendicitis and leads the patient to a final diagnosis only at surgical exploration, often characterized by diagnostic laparoscopy. Although rare, AT is not a new nosologi-cal entity. In fact, AT secondary to a fecalith impaction was first de-scribed by Payne in 1918 [7]. To date, approximately 53 further cases have been reported in the literature (Table 1).
The population most frequently affected is male pediatric patients and young adults. The median age is 33 years old. Most of the cases are primitive (60 %). The anatomic feature most favoring AT is the length of the appendix. Theoretically, the longer the appendix, the higher the risk of torsion. The most extended appendix ever reported measured 55 cm in length [8]. The literature review shows 20 AT cases in which the appendix was longer than 10 cm. The twist usually occurs in the long axis of the appendix and begins at the base or at least 1 cm from that, but it could also be more distal. The degree of torsion is usually between 180 and 1080 degrees. The direction is most commonly an- ticlockwise. Reviewing the pertinent literature, the tumors most fre-quently causing secondary AT are mucous cystadenomas (5 cases) and mucoceles (10 points) (Table 1).
|
Authors |
Year |
Age |
Sex |
Degree/direction of rotation |
Lenght of appendix, cm |
Etiology or complication |
|
Payne |
1918 |
37 |
F |
1,080/- |
7 |
Fecalith impaction |
|
Bevers |
1920 |
35 |
F |
720/- |
7.6 |
UD |
|
Mcfadden |
1926 |
UD |
M |
180/- |
12.7 |
UD |
|
Flatley |
1936 |
22 |
F |
900/- |
10.8 |
UD |
|
Dickson |
1953 |
60 |
F |
720/- |
11.5 |
Simple mucocele |
|
Cassie |
1953 |
25 |
M |
540 |
10 |
UD |
|
Carter |
1959 |
8 |
F |
>360/AC |
- |
UD |
|
King-Pan |
1965 |
18 |
F |
-/- |
10 |
Simple mucocele |
|
Ghent |
1966 |
21 |
M |
450/AC |
- |
Primary |
|
Ghent |
1966 |
12 |
M |
>360/C |
7 |
Primary |
|
Killam |
1969 |
47 |
M |
-/- |
- |
Mesoappendiceal lipoma |
|
De Bruin |
1969 |
28 |
F |
360/- |
10.5 |
UD |
|
Legg |
1973 |
29 |
M |
360/- |
10 |
UD |
|
Finch |
1974 |
38 |
F |
360/- |
- |
UD |
|
12 |
M |
270/AC |
- |
UD |
||
|
Won |
1977 |
35 |
M |
-/- |
12 |
UD |
|
Petersen |
1982 |
59 |
F |
540 |
10 |
UD |
|
William |
1983 |
4 |
M |
270/AC |
- |
UD |
|
Dewan |
1986 |
3 |
M |
720/AC |
- |
UD |
|
6 |
F |
1080/C |
7 |
UD |
||
|
16 |
M |
-/- |
- |
UD |
||
|
Waters |
1986 |
3 |
M |
720/- |
- |
UD |
|
Abu Zidan |
1992 |
32 |
F, pregnant |
-/C |
5.9 |
Mucocele |
|
Merret |
1992 |
14 |
M |
720/AC |
14 |
Normal appendix |
|
Fernando |
1995 |
6 |
M |
>360/AC |
13.5 |
UD |
|
Petersen |
1998 |
44 |
M |
540/- |
5.5 |
UD |
|
Uroz-Tristan |
1998 |
5 |
M |
360/AC |
- |
Absent mesoappendix |
|
Tzilinis |
2002 |
44 |
M |
540/C |
5.5 |
Primary |
|
Moten |
2002 |
44 |
F |
360/AC |
- |
Primary |
|
Oguzkurt |
2004 |
2 |
M |
270/AC |
10 |
Duplicated colon and appendix |
|
Bowling |
2006 |
Adult |
F |
-/- |
8 |
UD |
|
Bestman |
2006 |
35 |
F |
-/- |
7.5 |
Primary |
|
Sarin |
2006 |
9 |
M |
270/C |
8 |
Normal appendix |
|
Rajendran |
2006 |
29 |
F |
360/- |
11 |
Mucoele |
|
Karger |
2007 |
34 |
M |
180/C |
10 |
Mucinous cystadenoma |
|
Rudloff |
2007 |
28 |
F |
900/C |
5 |
Mucocele |
|
Herbert |
2007 |
59 |
M |
-/- |
12 |
Mucinous cystadenoma |
|
Hamada |
2007 |
79 |
M |
180/AC |
|
Mucinous cystadenoma |
|
Wani |
2008 |
76 |
M |
540/AC |
10 |
Fecalith |
|
Montes-Tapia |
2009 |
3 |
M |
-/- |
|
UD |
|
Wani |
2010 |
38 |
F |
180/C |
20 |
Adhesion from ovarian mucocele torsion |
|
Lee |
2011 |
78 |
F |
900/AC |
10.5 |
Mucocele |
|
Marsdin |
2011 |
48 |
M |
360/C |
|
UD |
|
Dimitriadis |
2012 |
52 |
F |
540/AC |
9 |
Caecal malposition |
|
Mishin |
2012 |
30 |
M |
360/C |
11 |
Mucinous cystoadenoma |
|
Stark |
2014 |
34 |
F |
720/C |
8 |
Mucinous cystoadenoma |
|
Grebic |
2015 |
70 |
M |
1800/C |
9 |
Mesoappendiceal lipoma |
|
Dubhashi |
2016 |
52 |
F |
180/C |
8 |
UD |
|
Siddharth |
2016 |
52 |
F |
180/AC |
8 |
Primary |
|
Ejtehadi |
2017 |
81 |
M |
-/- |
- |
Mucocele |
|
Wan Assan |
2017 |
30 |
M |
720/AC |
12 |
Mucocele |
|
Knol |
2020 |
66 |
F |
-/- |
9.6 |
Mucocele |
|
Nyandoro |
2022 |
5 |
M |
-/- |
- |
Mucocele |
|
Current |
2022 |
24 |
F |
200/C |
10 |
Primary |
From the pathophysiological point of view, torsion can cause a com- plete luminal obstruction and distal dilatation; blood supply becomes compromised firstly by a reduced venous outflow and then by occlu- sion of the appendicular artery. The resulting appendicular infarction leads to a bacterial translocation that presents clinically as an acute abdomen. In primary torsion, specimen examination shows secondary ischemic or necrotic changes and luminal dilatation distal to the tor- sion site without any other lesion [9].
The appendix, being a relatively mobile organ, can twist on itself and involve other organs. Singal reported a case in which the appendix caused intestinal obstruction by forming a band on the abdominal wall or an adjacent loop of bowel kinking the bowel itself; intraoperative findings revealed an inflamed appendix that was rotated around the ileum, forming a sort of a mass [10].
The presented case is a primary form of AT with a clockwise rotation diagnosed intraoperatively. As seen in our experience, abdominal US is not the gold standard tool for the preoperative diagnosis of appen-dicular torsion; to date, only Uroz-Tristan et al. mentioned the US for AT [11]. On the other hand, the US represents the right choice for simple acute appendychopathy. In our case report, the torsion was id- iopathic with no evidence of local lesion causing rotation. Treatment of AT is dependent on the underlying cause. An appendectomy is suf-ficient in case of a primary torsion without any abnormal lesions. However, using conservative therapy with antibiotics for AT can cause necrosis of the appendix, leading to perforation of the appendix and peritonitis. The optimal treatment should consist of prompt lapa- roscopic detorsion and appendectomy to avoid complications second-ary to appendiceal perforation and potential intraperitoneal spillage of appendiceal or mass contents. Despite being a surgical rarity, AT should always be considered in the differential diagnosis of patients with right lower quadrant abdominal pain (RLQAP).
Conclusion
AT shows a clinical presentation similar to acute appendicitis. Pre- operative diagnosis can be reached through a preoperative contrast- enhanced CT scan of the abdomen. For secondary forms of AT, a tu- mor must be excluded. AT must be included in the differential diag-nosis of pain localized in the right iliac fossa.
Written informed consent was obtained from the patient to publish this Case Report and any accompanying images. A copy of the written permission is available for review by the Editor-in-Chief of this journal.
References
- Marsdin EL, Griffiths C (2011) Primary torsion of vermiform ap- pendix mimicking acute appendicitis. BMJ Case Rep. 2011: bcr0320113979.
- Tzilinis A, Vahedi MH, Wittenborn WS (2002) Appendiceal tor- sion in an adult: Case report and review of the literature. Curr Surg. 59(4): 410‑1.
- Lee CH, Lee MR, Kim JC, Kang MJ, Jeong YJ (2011) Torsion of a mucocele of the vermiform appendix: A case report and review of the literature. J Korean Surg Soc. 81(Suppl 1): S47‑50.
- Wan Hassan WA, Tay YK, Ghadiri M (2018) Torsion of the Ver- miform Appendix: A Case Report and Review of Literature. Am J Case Rep. 19: 365-368.
- Endo K, Sato M, Saga K, Higashio A, Yuba Y, et al. (2020) Tor- sion of vermiform appendix: case report and review of the litera- ture. Surg Case Rep. 6(1): 6
- Val‑Bernal JF, González‑Vela C, Garijo MF (1996) Primary acute torsion of the vermiform appendix. Pediatr Pathol Lab Med. 16(4): 655‑61.
- Payne JE (1918) A case of torsion of appendix. Br J Surg. 6: 327.
- Samaha AH, Tawfik AS, Abbas TO, Abdelhamid A (2011) Megaloappendix: A Case Report. Case Rep Surg. 2011: 729304.
- Cazejust J, Laumonier E (2021) Torsion and necrosis of a fatty appendix of the vermiform appendix. Clin Res Hepatol Gastroen- terol. 45(2): 101646.
- Singal R, Zaman M, Sharma BP (2017) Unusual Entities of Ap- pendix Mimicking Appendicitis Clinically – Emphasis on Diag- nosis and Treatment. MAEDICA – a Journal of Clinical Medicine. 12(1): 23-29.
- Uroz-Tristan J, García-Urgelles X, Poenaru D, Avila-Suarez R, Valenciano-Fuentes B (1998) Torsion of vermiform appendix: Value of ultrasonographic findings. Eur J Pediatr Surg. 8(6): 376‑7.