Pablo Ferrer Campos
PhD Biochemistry, Clinic Hospital Universidad de Chile Molecular Medicine Laboratory, Section of Immunology, HIV and Allergies Department of Internal Medicine, Avenue Carlos Lorca Tobar 999, Independencia.
*Corresponding Author: Pablo Ferrer Campos, PhD Biochemistry, Clinic Hospital Universidad de Chile Molecular Medicine Laboratory, Section of Immunology, HIV and Allergies. Department of Internal Medicine, Avenue Carlos Lorca Tobar 999, Independencia.
Abstract
APOBEC3G is a cellular antiviral protein able to inhibit HIV replication and may protect from progression to AIDS. In this work, we showed the APOBEC3G activity in an asymptomatic HIV patient under therapy without complete viral suppression. The patient was a homosexual Chilean man with an initial CD4 count of 427 cells/mm3 and a viral load of 33,000 copies/mL. In March 2012 began therapy with ABC, 3TC, and EFV. Seven months later, the viral load was < 40 copies/mL. However, because of persistent low-level viremia reverse transcriptase (RT) and protease genes were investigated by PCR and sequencing using HIV proviral DNA. The sequences obtained were used for the resistance report and M184I and M230I mutations were found. M184I mutation causes high-level resistance to FTC and 3TC and low-level resistance to ABC. M230I was associated with low-level resistance to EFV, DOR, and ETR and intermediate resistance to NVP and RPV.
Surprisingly we detected three stop codons in positions 88, 153, and 212 that correspond to the tryptophan codon in the RT. In our patient, the three-stop codon detected at the tryptophan codon of RT suggests an APOBEC 3G hypermutation activity. These stop codons within RT of HIV are deleterious to replication and this could explain the persistent low viral load. In conclusion, using proviral DNA we detected APOBEC3G activity in an HIV patient which showed controllers. Finally, we also showed that proviral DNA is very useful in detecting resistances mutations in cases of low-level viremia and this allowed an earlier therapeutic intervention in the patient.
Keywords: HIV-1, APOBEC3G, cure, proviral DNA, resistance, stop codon, case report, endogenization HIV
Introduction
APOBEC3G (apolipoprotein B mRNA-editing enzyme, catalytic polypeptide-like editing complex 3G) are enzymes important in both innate and adaptive immune responses against diverse kinds of viruses including HIV-1 [1]. APOBEC3G has the ability to change to A the G nucleotide present in the viral genome of HIV. Due to a G to A substitution in the TGG codon that coding for amino acid Tryptophan (W) APOBEC3G activity results in the introduction of a stop codon in all cases impairing the function of viral protein and HIV replication [2]. Thus, APOBEC3G reduces the viral load in infected patients conferring protection against progression to AIDS [3]. This strategy is an ancestral mechanism of retrovirus endogenization in humans and animals [4].
Material and Methods
The patient
In November 2011, a 29 years-old homosexual Chilean, was diagnosed HIV-positive with a CD4 cell count of 427 cells/mm3, HIV-RNA viral load (VL) of 33,000 copies/mL, and platelet count of 42,000 cells/mm3. This patient was not infected with other pathogens. At the time of diagnosis, this patient was under treatment with testosterone as a consequence of a previous testicular cancer treated by a surgical approach (2009). In March 2012, he began antiretroviral therapy (ART) with Abacavir (ABC), Lamivudine (3TC), and Efavirenz (EFV) because of the low CD4 cell count and the persistent thrombocytopenia. The clinical evolution was followed by five years with periodical medical checks at least once by year. The antiviral treatment reduces the viral load by 825-fold (2.9 log), achieving an undetectable status, however, this condition was not permanent along with the treatment, increasing progressively the VL, reaching a persistent low-level viremia (LLV) likely due to drug interaction between testosterone and EFV. Despite the LLV, the patient shows a low count of CD4 across all the treatments (Table 1). This work is part of Project AOIC#684/14. The patient was informed of the study’s scope and test limitations through pre-and post-assays counseling and voluntarily agreed to participate signing the informed consent approved by the Ethics Committee of the Hospital Clinico Universidad de Chile.
Table 1: Diagnosis, treatments, CD4 cell count and viral load evolution of the patient.
|
Date (month/year) |
CD4 cell count (%) |
Viral load (Copies/mL) |
Treatmen (HAART) |
|
11/2011c |
427 (14 %) |
33,000 |
Without HAART |
|
3/2012 |
427 (14 %) |
33,000 |
ABC+3TC+EFV |
|
10/2012 |
432 (21 %) |
< 40 |
ABC+3TC+EFV |
|
10/2013 |
395 (22 %) |
65 |
ABC+3TC+EFV |
|
2/2014 |
395 (22 %) |
105 |
ABC+3TC+EFV |
|
4/2014 |
511 (28%) |
47 |
ABC+3TC+EFV |
|
3/2015 |
537 (28 %) |
78 |
ABC+3TC+EFV |
|
6/2015 |
537 (28 %) |
78 |
AZT+TDF+ATV/r |
|
10/2015 |
425 (27 %) |
<40 |
AZT+TDF+ATV/r |
|
3/2016 |
448 (27 %) |
76 |
AZT+TDF+ATV/r |
|
7/2016 |
460 (31 %) |
<40 |
AZT+TDF+ATV/r |
Abbreviations
HAART: Highly Active Antiretroviral Therapy Treatment.
ABC: Abacavir.
ATV/r: Atazanavir/ritonavir.
AZT: zidovudine.
EFV: Efavirenz.
3TC: Lamivudine.
TDF: Tenofovir.
Viral load assay
Determination of viral load was realized by Real-time type 1 (HIV-1) HIV assay (Abbott Diagnostics) that allows the quantification of HIV-1 RNA in plasma samples from infected patients, in the range of 40 to 10,000,000 copies/mL. It detects and quantifies the viral load of a large group of viruses, group M (subtypes A-H), group O, and group N. A viral load < 40 copies/mL is considered undetectable.
CD4 cell count
CD4 cell count and (%) was realized using blood/EDTA with The AQUIOSTM CL flow cytometer from Beckman Coulter.
HIV Resistance Test by PCR and Sequencing
To characterize if LLV is the consequence of HIV drugs resistance mutations (DRMs) that confer resistance against ART, we carried out an HIV resistance test. Total DNA human genomic (HIV proviral DNA is integrated into Human DNA) was extracted from 200 µL of fresh whole blood using QIAamp® DNA Mini Kit (Qiagen). Then full HIV reverse transcriptase (RT) and protease genes were amplified and sequenced. Amplifications were performed in duplicated (short and long fragments) by nested PCR using 5 µL of HIV proviral DNA [5]. Both PCR products were sequenced directly in Macrogen USA Co according to the method described previously and DRMs were identified using Stanford Database [6,7].
Results
The analysis of the HIV resistance test allowed identifying two mutations (M184I and M230I) in the coding region of the RT gene. Mutation M184I was associated with resistance to the nucleoside reverse transcriptase inhibitors (NRTIs): 3TC and FTC (high level) and ABC (low level), while mutation M230I to non-nucleoside reverse-transcriptase inhibitors (NNRTIs): EFV and ETR (low level), and NVP and RVP (intermediate level) (Table 2). Additionally, in the RT gene, we detected three mutations in the codon that codes for the amino acid tryptophan (W, in the nomenclature of one letter). A nonsense mutation is the substitution of a single base pair that leads to the appearance of astop codon where previously there was a codon specifying an amino acid. The presence of this premature stop codon results in the production of a shortened and likely nonfunctional protein. The three-stop codon was detected in the positions W88*, W153*, and W212*. This suggests the participation of APOBEC3G in the hypermutation observed in the RT gene. The muted HIV RT sequence was deposited in GenBank with accession number KX530453 (Figure 1). Then to reduce the VL, we changed the ART to Zidovudine (AZT)+Tenofovir (TDF)+ Atazanavir/ritonavir (ATV/r). Four months after we evaluated the VL, being < 40 copies/mL.
Table 2: Drugs resistance interpretation in Reverse Transcriptase HIV-1
|
M184I Mutation/NRTIs Drugs |
Prediction |
|
Abacavir (ABC) |
Low-Level Resistance |
|
Zidovudine (AZT) |
Susceptible |
|
Stavudine (D4T) |
Susceptible |
|
Didanosine (DDI) |
Susceptible |
|
Emtricitabine (FTC) |
High-Level Resistance |
|
Lamivudine (3TC) |
High-Level Resistance |
|
Tenofovir (TDF) |
Susceptible |
|
M230I Mutation/NNRTIs Drugs |
Prediction |
|
Doravirine (DOR) |
Low-Level Resistance |
|
Efavirenz (EFV) |
Low-Level Resistance |
|
Etravirine (ETR) |
Low-Level Resistance |
|
Nevirapine (NVP) |
Intermediate Resistance |
|
Rilpivirine (RPV) |
Intermediate Resistance |
RT comments (Standford University HIV Drug Resistance Database) (7)
NRTI
M184V/I cause high-level in vitro resistance to 3TC and FTC and low-level resistance to ddI and ABC. However, M184V/I are not contraindications to continued treatment with 3TC or FTC because they increase susceptibility to AZT, TDF and d4T and are associated with clinically significant reductions in HIV-1 replication.
NNRTI
M230I is an extremely rare mutation selected by RPV. Its effects on NNRTI susceptibility have not been well studied. It also often occurs because of APOBEC-mediated G-to-A hypermutation resulting in viruses that are likely to be noninfectious.
Dosage Considerations
This virus is predicted to have intermediate-level reduced susceptibility to RPV. The use of the combination of CAB/RPV should be contraindicated.
The three-stop codon were detected in the positions W88S*, W153L*, and W212S*. This suggests the participation of APOBEC3G in the hypermutation observed in the RT gene.
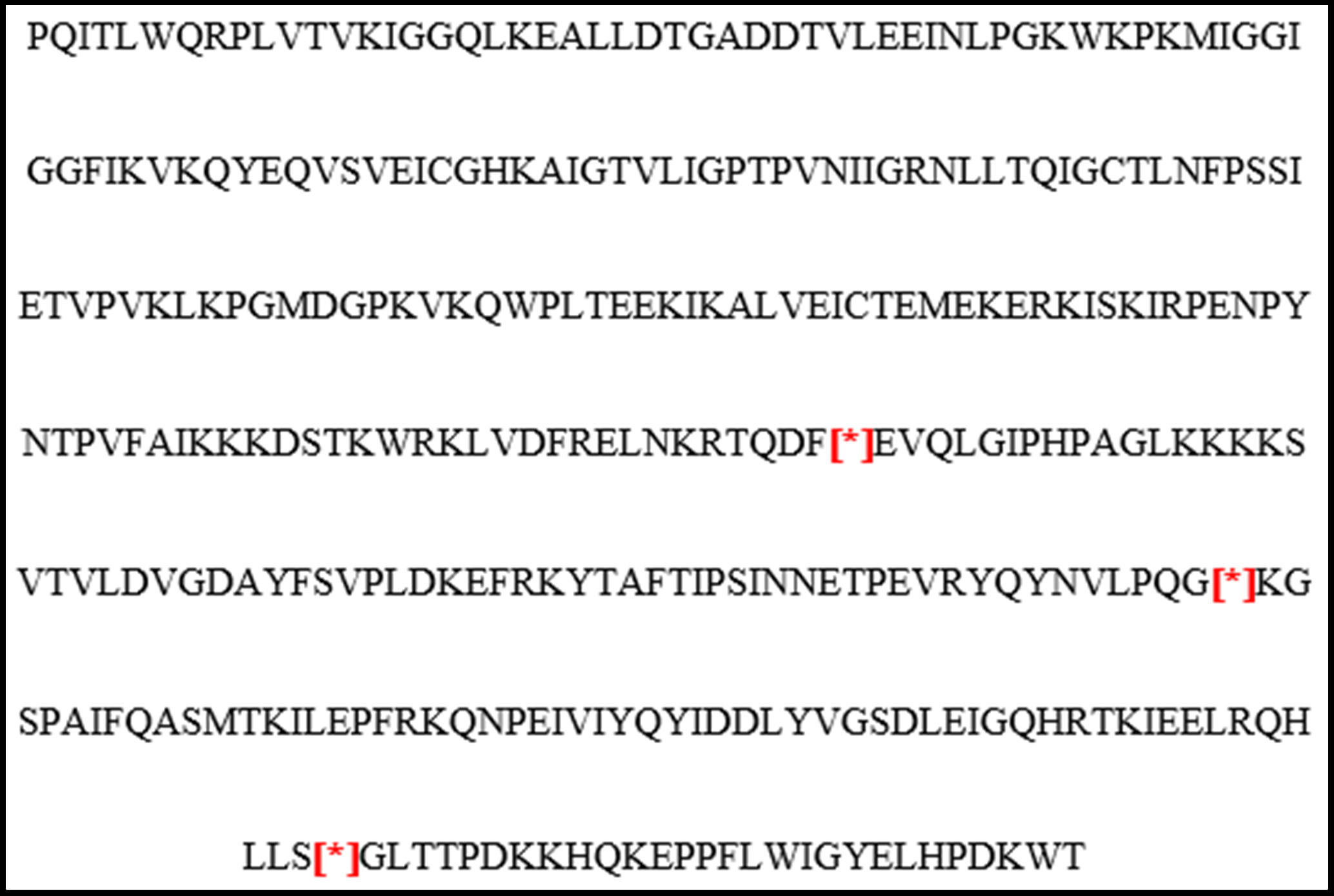
Figure 1. HIV RT protein sequence hacked by human APOBEC 3G. HIV-1 isolate HIV1505DNAp from Chile pol protein-like (pol) gene, partial sequence GenBank: KX530453.1 (10). [*] Indicate the three-stop codon that were detected in the positions W88*, W153* and W212*.
Discussion
Unfortunately, a significant number of patients with HIV do not manage to reach undetectability in their viral load, despite being on antiretroviral therapy. This results in persistent low-level viremias that could reflect the emergence of treatment-resistant viral quasispecies. Therefore, to clarify this phenomenon it is essential to perform a resistance genotype. As these low viremias are usually less than 1,000 copies/mL, the use of HIV proviral DNA is key to having information about the genetic sequence of the viral variants present in these patients, since there are no genotyping techniques on the market that can make the genotype from RNA with loads below 1,000 copies/mL. This case is interesting since the patient has two clinically relevant mutations that confer resistance to two families of drugs, only has a viral load as low as 78 copies/mL, when what was expected for these situations was to have thousands of copies of the virus. This surprising low viral load leads to strong speculation about the action of APOBEC3G.
However, in our daily clinical routine, it is not the most frequent to find in patients with low-level viremias mutations associated with resistance. For example, in our cohort of 212 patients with viremias less than one thousand copies/mL, in reverse transcriptase, we found that only 44 (26.8 %) patients were resistant to any antiretroviral (26.8 %) and 117 (71.3 %) were sensitive to all drugs (data not shown).
APOBEC 3G is a well-known antiviral mechanism that works by hacking the genetic program of HIV. In turn, HIV responds with the VIF protein that has the can ability to inhibit the antiviral activity of APOBEC3G [11], so there is a fine molecular interaction between the host and the pathogen, where sometimes the host wins and sometimes the pathogen wins A good example of this molecular interaction between APOBEC 3G from the patient and Vif from the virus is the article published by Tadashi Kikuchi et al., in 2015 in which they evaluated the anti- APOBEC3G activity of Vif, quantified in terms of luciferase signal. Comparing APOBEC 3G activity in 46 elite controllers (EC, HIV-1 infected persons who control viremia below detection limit without antiviral therapy) and 46 non-controllers (NC) found that on average, the anti-APOBEC3G activities of EC-derived Vif sequences were significantly lower than those of EC-derived sequences of NC. This means that APOBEC 3G activity is significantly higher in EC than in NC. The viral polymorphism could explain the reduced anti-APOBEC3G activity of EC-derived Vif, suggesting that various combinations of minor polymorphisms may underlie these effects. These results further support the idea of relative attenuation of viral protein function in EC-derived HIV sequences. This work reinforces the importance of the APOBEC 3G mechanism as a host protective factor against HIV [12].
The APOBEC3G strategy is very novel since it takes advantage of the fact that the tryptophan amino acid is encoded only by the UGG codon and that changing the G for A has the possibility of producing the three stop codons, UAG, UGA, and UAA which generates a non-functional truncated protein [13].
APOBEC3G is a mechanism of genetic evolution for the virus, through which it manages to escape the selective pressure of the immune system or the action of antiretroviral therapy. However, this escape does not come free for the virus since the resulting quasispecies has modifications in its genome that make it less efficient in replication and infective capacity.
It is of great clinical importance to be able to demonstrate that those patients with persistent low-level viremias who are susceptible to all drugs have defective viruses due to APOBEC 3G or other immunogenetic mechanisms of the host since it would be less of concern to the attending physician if the patient does not reach the ideal of undetectability [14]. Undoubtedly, this type of study is a window of research that opens in the era of seeking definitive solutions in the clinical management of people living with HIV.
A limitation of our work is that we did not look for other genetic determinants in the patient such as the HLA system, the D 32 mutation in the CCR5 coreceptor, or cytokine expression that could have any association with APOBEC 3G activity or with the clinical course followed by the patient. They are certainly targets for further research in this area.
In conclusion, is very suggestive our patient has an APOBEC3G mechanism that allows controlling the viral replication probably due to the synthesis of nonfunctional or truncated RT protein. Thanks, to a genotyping proviral DNA we show a case report which contains mutations related to resistance at two families of antiretroviral drugs, and three non-sense mutations at the W codon of HIV RT. The presence of these nonsense mutations suggests an APOBEC3G activity that could explain the LLV and CD4 count up to 500 cells/mm3 for approximately five years without relevant clinical consequences.
Acknowledgments: This work was supported by grant AOIC#684/14 from Hospital Clínico Universidad de Chile.
Conflict of Interest: The author declares no potential conflicts of interest exist.
References
- Gandhi SK, Siliciano JD, Bailey JR, Siliciano RF, Blankson JN (2008) Role of APOBEC3G/F-Mediated Hypermutation in the Control of Human Immunodeficiency Virus Type 1 in Elite Suppressors. J Virol. 82(6): 3125–30.
- Ran X, Ao Z, Yao X (2016) Apobec3G-Based Strategies to Defeat HIV Infection. Curr HIV Res. 14(3): 217-24.
- Jin X, Brooks A, Chen H, Bennett R, Reichman R, et al. (2005) APOBEC3G/CEM15 (hA3G) mRNA levels associate inversely with human immunodeficiency virus viremia. J Virol. 79(17): 11513-16.
- Holmes EC (2011) The Evolution of Endogenous Viral Elements. Cell Host & Microbe. 10(4): 368-77.
- Lübke N, Di Cristanziano V, Sierra S, Knops E, Schülter E, et al. (2015) Proviral DNA as target for HIV-1 Resistance analysis. Intervirology. 58(3): 184-89.
- Woods CK, Brumme CJ, Liu TF, Chui CK, Chu AL, et al. (2012) Automating HIV Drug Resistance Genotyping with RECall, a Free accessible sequence analysis tool. J Clin Microbiol. 50(6): 1936–42.
- Standford University HIV Drug Resistance Database.
- Colson P, Ravaux I, Tamalet C, Glazunova O, Baptiste E, et al. (2014) HIV infection en route to endogenization: two cases. Clin Microbiol Infect. 20(12): 1280–88.
- Eyzaguirre LM, Charurat M, Redfield RR, Blattner WA, Carr JK, et al. (2013) Elevated hypermutation levels in HIV-1 natural viral suppressors. Virology. 443(2): 306-12.
- Ferrer P. HIV-1 isolate HIV1505DNAp from Chile pol protein- like (pol) gene, part-Nucleotide - NCBI (nih.gov).
- Sadeghpour S, Khodaee S, Rahnama M, Rahimi H, Ebrahimi D (2021) Human APOBEC3 Variations and Viral Infection. Viruses. 13(7): 1366.
- Kikuchi T, Iwabu Y, Tada T, Kawana-Tachikawa A, Koga M, et al. (2015) Anti-APOBEC3G activity of HIV-1 Vif protein is attenuated in elite controllers. J Virol. 89(9): 4992–5001.
- Ikeda T, Yue Y, Shimizu R, Nasser H (2021) Potential Utilization of APOBEC3-Mediated Mutagenesis for an HIV-1 Functional Cure. Front. Microbiol. 12: 686357.
- Singh H, Jadhav S, Khan AA, Aggarwal SK, Choudhari R, et al. (2022) APOBEC3, TRIM5α, and BST2 polymorphisms in healthy individuals of various populations with special references to its impact on HIV transmission. Microbial Pathogenesis 162: 105326.



