D. van de Hoef*, C. Davis, R. Goubran
Department of General Surgery, University Hospital Galway, Newcastle Road, Co. Galway, Ireland.
*Corresponding Author: D. van de Hoef, Department of General Surgery, University Hospital Galway, Newcastle Road, Co. Galway, Ireland.
Abstract
Presentation: We present a 22-year-old female who underwent a diagnostic laparoscopy for right iliac fossa pain query appendicitis.
Diagnosis: Having high inflammatory markers and persistent pain, she was brought for diagnostic laparoscopy. We identified terminal ileitis and incidentally found an unusually segmented but macroscopically appendix. Histologically, the appendix was non-inflamed, but the lumens were fibrosed.
Treatment: The two appendiceal segments were surgically removed to avoid future diagnostic confusion and out-rule microscopic inflammation. The patient was sent home comfortably with a gastroenterology follow-up.
Discussion/Conclusion: This is the first presentation of a viable, non-inflamed, segmented appendix. The cause for this unusual segmentation is unclear.
Introduction
Acute appendicitis is a frequently encountered clinical entity for the general surgeon with variability in presentation. Diagnostic laparoscopy is one surgical method that may be used to clinch the diagnosis and may be preferred over cross-sectional imaging when aiming to avoid the radiation associated with CT, especially among young women. Here, we discuss an unusual macroscopic and histological finding of a partly obliterated appendix found at a diagnostic laparoscopy performed in a 22-year-old female who presented with right-iliac fossa pain.
Case Report
A 22-year-old female presented to the Emergency Department with a 1-day history of right-sided abdominal pain. She had associated nausea and anorexia but no vomiting, change in bowel motions, urinary symptoms, or menstrual irregularities. Her medical and surgical history were unremarkable. Her vitals were within normal limits. Her abdominal examination revealed mild right iliac fossa tenderness without rebound or guarding. Bedside urinary dipstick testing returned no abnormal results. Her erect Chest X-ray was unremarkable.
Her laboratory tests were as follows;
|
C-Reactive Protein |
144 mg/L |
(0 – 5 mg/L) |
|
White Cell Count |
12.2 x 109/L |
(4 – 10 x 109/L) |
|
Neutrophils |
9.81 x 109/L |
(2 – 7 x 109/L) |
|
Lymphocytes |
1.3 x 109/L |
(1 – 3 x 109/L) |
|
Haemoglobin |
12.7 g/dL |
(12 – 15 g/dL) |
Given her relatively high inflammatory markers and worsening pain overnight, the decision was made to take her to the theatre for a diagnostic laparoscopy.
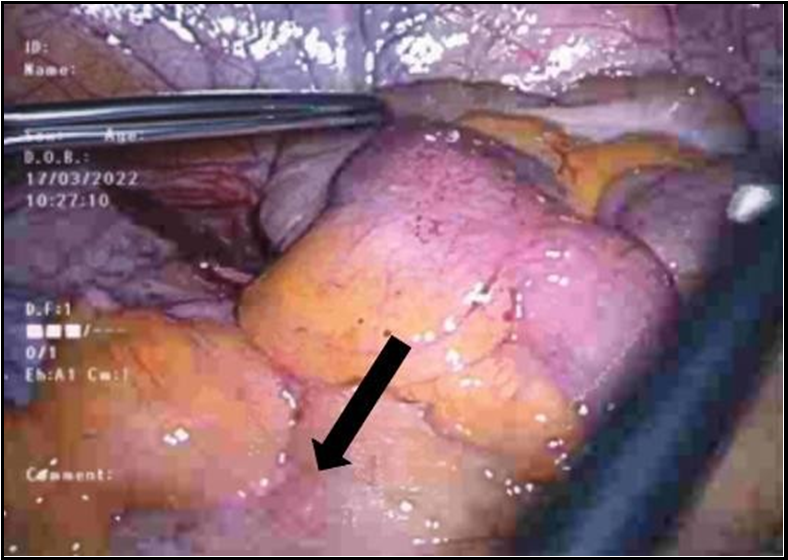
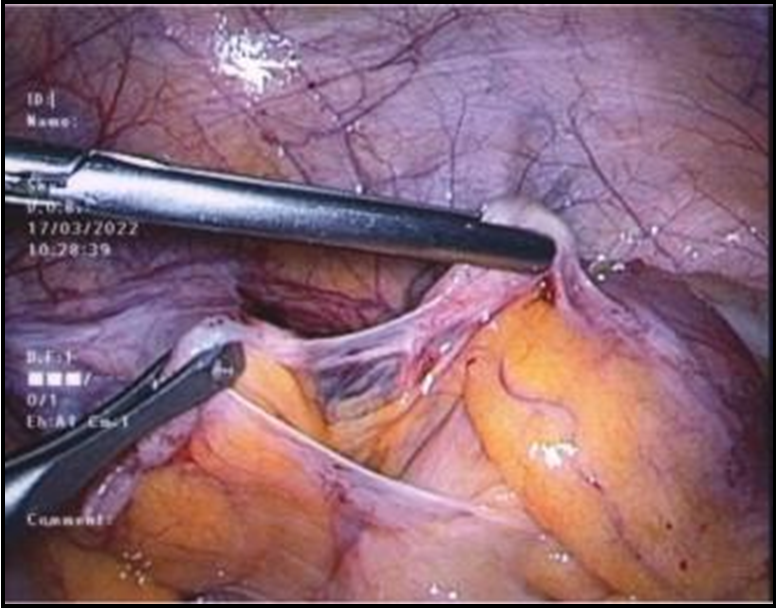
Intra-operatively, the cause of her right iliac fossa pain was identified as terminal ileitis. Her terminal ileum was mild-moderately inflamed with visible lymphadenopathy within the adjacent mesentery (Figure 1). The rest of her small and large bowel, including caecum and appendix, was assessed and found to be non-inflamed. However, the appendix's structure was markedly abnormal; the tip and base of the appendix were discontinuous in two distinct segments, which were attached only by thin fibrous tissue (Figure 2). The distal segment was viable and healthy but closed at both ends. The mesenteric perfusion of this segment was intact. The proximal segment was also healthy in appearance but short and blind-ended with normal- appearing mesenteric perfusion. The two segments of the appendix were removed to avoid future diagnostic confusion and to out-rule any microscopic causes for her abdominal pain. She had an uncomplicated postoperative course and was sent home on day 2 post- operatively with a follow-up with gastroenterology.
Histologically, the tip of the appendix was only tenuously attached to the main body of the appendix with fibrous tissue. There was no distension with mucin nor evidence of perforation. Both lumens were centrally fibrosed but showed no evidence of malignancy or inflammation.
Figure 1: Terminal Ileitis with local mesenteric lymphadenopathy
Figure 2: Segmented Appendix held together by fibrous tissue
Discussion
This is the first case presented in the literature of a viable, non- inflamed segmented vermiform appendix. Developmental abnormalities of the vermiform appendix have been reported, including duplication, absence, or agenesis, but these are rare [1,2]. There have been rare cases reported of autoamputation of the appendix, but these are typically associated with appendiceal macroscopic inflammation and necrotic features [3]. One case report of an auto-amputated appendix re-implanting itself against the pelvic side wall was found [4]. Agenesis of the vermiform appendix is another rare phenomenon reported in 1:100,000 laparotomies for suspected appendicitis [5]. In these cases, there is no connection between the appendix and the caecum, and the patient's presentation has been due to the inflammatory reaction of the blind-ended appendix [6]. The mesenteric lymphadenopathy in these cases is likely due to the appendicular inflammation contrary to the terminal ileal inflammation and normal appendix, as seen in our case.
There have also been reported cases of fibrous obliteration of the appendix that can result in clinical presentations and CT findings that may mimic acute appendicitis [7]. This obliteration is a histological diagnosis characterised by luminal obliteration by fibrous tissue. It is thought that recurrent, subclinical attacks of inflammation may trigger this process [8]. Histologically, the fibrosis begins with intra-mucosal neural tissue hyperplasia and eventual fibrosis, with loss of normal lymphoid follicles, mucosa, and crypts [9]. It is thought that neural tissue proliferation causes symptoms that mimic acute appendicitis [10]. Our patient's symptoms were related to the terminalileitis rather than the appendicitis obliterans. Following a discussion between clinical pathologists and the operative team, an exact cause for the unusual appearance of the appendix has yet to be determined.
References
- Hei EL (2003) Congenital absence of the vermiform appendix. ANZ J Surg. 73(10): 862.
- Elias EG, Hults R (1967) Congenital absence of vermiform appendix. Archives of surgery. 95(2): 257-258.
- Savran B, KoAak A, Şanal B, Karakuş YT (2014) Autoamputated Appendix: A Case Report. Global Journal of Medical Research. 14(4).
- Abu Masud Ansari SK, Kumar N (2018) A Curious Case of Missing Appendix. Journal of Clinical Gastroenterology and Hepatology.
- Chèvre F, Gillet M, Vuilleumier H (2000) Agenesis of the vermiform appendix. Surg Laparosc Endosc Percutan Tech. 10(2): 110-2.
- Yaylak F, Algin MC, Gungor Y, Korkmaz M (2013) Atresia of the appendix vermiformis: a rare case of developmental abnormality. World journal of gastroenterology. 19(1): 122-124.
- Choi SJ, Jang YJ, Lee D, Cho SH, Kim GC, et al. (2014) Two Cases of Fibrous Obliteration of the Appendix, Mimicking Acute Appendicitis. Journal of the Korean Radiological Society. 70(6): 430.
- Olsen BS, Holck S (1987) Neurogenous hyperplasia leading to appendiceal obliteration: an immunohistochemical study of 237 cases. Histopathology. 11: 843-9.
- Senn N (1894) Appendicitis Obliterans. Journal of the American Medical Association. 22(12): 403–411.
- Sesia SB, Mayr J, Bruder E, Haecker FM (2013) Neurogenic appendicopathy: clinical, macroscopic, and histopathological presentation in pediatric patients. Eur J Pediatr Surg. 23(3): 238- 42.