Gülistan Barca Önen1*, Duygu Kara2, Feray Gürsoy2
1Aydın State Hospital, Anesthesiology and Reanimation Clinic
2Aydın Adnan Menderes University Medical Faculty, Anesthesiology and Reanimation Department
*Corresponding Author: Gülistan Barca Önen, Aydın State Hospital, Anesthesiology and Reanimation Clinic
Abstract
Mucopolysaccharidosis type IIIA (MPS IIIA, Sanfilippo syndrome) is a lysosomal storage disorder characterized by craniofacial dysmorphism, macroglossia, and short neck, all of which contribute to an increased risk of difficult airway management during anesthesia. Foreign body aspiration, a frequent pediatric emergency, further complicates anesthetic care in these patients. We present the case of an eight-year-old girl with MPS IIIA requiring emergency bronchoscopy for tracheal foreign body removal. A difficult airway was anticipated due to her phenotypic features. Despite desaturation during the first attempt at rigid bronchoscopy, oxygenation was restored with mask ventilation, and the foreign body was successfully removed on the second attempt. This case highlights the anesthetic challenges of managing pediatric patients with MPS in emergency settings. It also underscores the importance of thorough preparation, the availability of alternative airway devices, and multidisciplinary teamwork to prevent complications.
Keywords: Mucopolysaccharidosis IIIA, Difficult airway, Emergency bronchoscopy, Pediatric anesthesia, Foreign body aspiration
Introduction
Mucopolysaccharidoses (MPS) are a heterogeneous group of lysosomal storage diseases caused by deficiencies in specific enzymes required for the degradation of glycosaminoglycans (GAG). The accumulation of these GAG leads to progressive damage to multiple organ systems. Among these, MPS IIIA, also known as Sanfilippo syndrome type A, is particularly associated with neurocognitive decline and distinctive craniofacial features. The craniofacial abnormalities, including coarse facial features, macroglossia, short neck, and skeletal malformations, create substantial difficulties for anesthesiologists, particularly in securing the airway [1]. Moreover, although some literature suggests that MPS IIIA may carry less airway difficulty compared to other MPS subtypes, many cases still exhibit significant airway management challenges [2].
Foreign body aspiration remains one of the most common pediatric emergencies requiring urgent bronchoscopy, and the risk of complications is markedly increased in patients with MPS [3]. The combination of urgent surgical intervention, the need for rigid bronchoscopy (the therapeutic gold standard in pediatric foreign body removal) [4], and the patient’s underlying pathology necessitates meticulous planning and preparedness by the anesthetic team. This report describes a patient with MPS IIIA who presented with tracheal foreign body aspiration and required emergency rigid bronchoscopy. We detail the anesthetic challenges, airway management strategies, and postoperative considerations, while comparing our experience with the existing literature [5].
Case Report
An eight-year-old girl was brought to the emergency department with acute onset noisy breathing and stridor. On arrival, she was hypoxemic with SpO₂ of 86%, despite receiving 6 L/min of oxygen via nasal cannula. A chest radiograph confirmed the presence of a foreign body lodged in the trachea. The patient had a known diagnosis of MPS IIIA, with a history of delayed neurocognitive development. Physical examination revealed coarse facial features, macroglossia, short neck, and craniofacial dysmorphism, all suggestive of a difficult airway scenario (Figure 1). Emergency rigid bronchoscopy was indicated for removal of the foreign body. Standard American Society of Anesthesiologists monitoring was instituted in the operating room. Due the high risk of airway difficulty, a video laryngoscope, endotracheal tubes of various sizes, supraglottic airway devices including laryngeal mask airway (LMA), and a rigid bronchoscope were prepared and checked prior to induction. Preoxygenation was performed for three minutes with 100% oxygen. Anesthesia was induced with propofol 2 mg/kg, rocuronium 0.6 mg/kg, and fentanyl 1 μg/kg. Anesthesia was maintained with a continuous infusion of propofol.
Figure 1: Coarse facial features, macroglossia, and short neck consistent with mucopolysaccharidosis type.
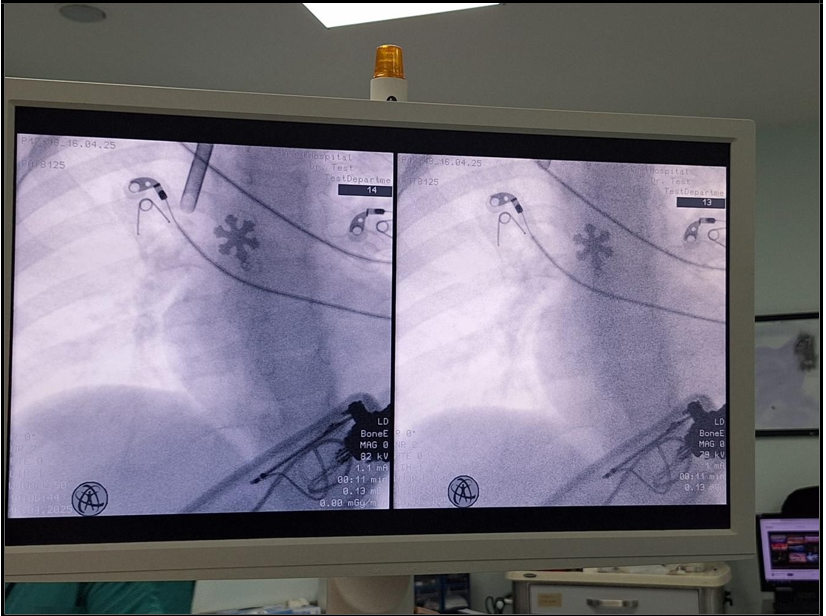
The surgeon attempted rigid bronchoscopy, although the first attempt was unsuccessful, and the patient experienced severe desaturation with SpO₂ dropping to 40%. Immediate mask ventilation was provided, which restored oxygenation. A second attempt at rigid bronchoscopy was then successfully performed, leading to removal of a snowflake-shaped pendant from the right main bronchus (Figure 2). In order to reduce the risk of post-procedural airway edema, prednisolone 1 mg/kg was administered intravenously.
Tracheal intubation with video laryngoscopy was achieved on the second attempt, ensuring a secure airway for the remainder of the procedure. At the end of the procedure, postoperative analgesia was achieved with intravenous paracetamol, and neuromuscular blockade was reversed with sugammadex. The patient was extubated uneventfully and observed in the post-anesthesia care unit for six hours before being transferred to the pediatric ward.
Figure 2: Snowflake-shaped pendant removed from the right main bronchus during rigid bronchoscopy.
Discussion
The management of anesthesia in children with MPS is challenging due to multiple anatomical and systemic factors. Airway management is particularly difficult because of macroglossia, thickened pharyngeal tissues, short neck, and limited cervical mobility, all of which contribute to difficulty in mask ventilation, laryngoscopy, and intubation [1]. Several reports have described failed intubation and airway trauma in this patient group, with some cases requiring emergency tracheostomy [3]. The urgency of foreign body aspiration cases also further complicates anesthetic planning, since time for detailed assessment and gradual induction is frequently limited.
Rigid bronchoscopy remains the therapeutic method of choice for foreign body removal in children, enabling airway protection and safe extraction even for sharp or irregular objects [4]. The desaturation that occurred during the first bronchoscopy attempt highlights the vulnerability of pediatric patients with limited oxygen reserves [5]. Prompt recognition and effective mask ventilation were critical in preventing adverse outcomes. The successful use of video laryngoscopy for subsequent intubation reinforces the recommendation that advanced airway devices should always be readily available for patients with MPS [3, 6].
In addition to airway considerations, anesthesiologists must remain vigilant in terms of systemic complications. Patients with MPS frequently present with cardiac involvement, including valvular disease and conduction abnormalities, which may increase the perioperative risk [5]. Although not present in this case, such comorbidities should be assessed whenever possible. The administration of corticosteroids, as in the present case, can reduce airway edema after multiple manipulations, potentially improving postoperative recovery [7].
Foreign body aspiration in children is a life-threatening emergency that requires rapid diagnosis and prompt intervention to avoid severe morbidity or mortality [8], particularly in syndromic patients with difficult airway anatomy. Our experience aligns with the previous literature emphasizing the importance of preparation, communication, and teamwork. Walker et al. described multidisciplinary planning and the availability of alternative strategies as key to successful airway management in MPS [3]. Richa et al. similarly concluded that close collaboration between anesthesiologists and surgeons minimizes complications during airway procedures in this high-risk population [5].
Conclusion
Airway management in pediatric patients with MPS is extremely challenging, particularly during emergencies such as foreign body aspiration. Anticipating a difficult airway, preparing alternative airway equipment, and ensuring multidisciplinary collaboration are essential for safe outcomes. This case underscores the importance of vigilance and thorough preparation to prevent life-threatening complications.
References
- Cohen MA, Stuart GM (2017) Delivery of anesthesia for children with Mucopolysaccharidosis Type III (Sanfilippo syndrome): a review of 86 anesthetics. Paediatr Anaesth. 27(4): 363-369.
- Clark BM, Sprung J, Weingarten TN, Warner ME (2018) Anesthesia for patients with mucopolysaccharidoses: Comprehensive review of the literature with emphasis on airway management. Bosn J Basic Med Sci. 18(1): 1-7.
- Walker R, Belani KG, Braunlin EA, Bruce IA, Hack H, et al. (2013) Anaesthesia and airway management in mucopolysaccharidosis. J Inherit Metab Dis. 36(2): 211-9.
- Chai J, Wu XY, Han N, Wang LY, Chen WM (2014) A retrospective study of anesthesia during rigid bronchoscopy for airway foreign body removal in children: propofol and sevoflurane with spontaneous ventilation. Paediatr Anaesth. 24(10): 1031-6.
- Frawley G, Fuenzalida D, Donath S, Yaplito-Lee J, Peters H (2012) A retrospective audit of anesthetic techniques and complications in children with mucopolysaccharidoses. Paediatr Anaesth. 22(8): 737-44.
- Goudra B, Sundararaman L, Chandar P, Green M (2024) Anesthesia for bronchoscopy – an update. J Clin Med. 13(21): 6471.
- Megens JH, de Wit M, van Hasselt PM, Boelens JJ, van der Werff DB, et al. (2014) Perioperative complications in patients diagnosed with mucopolysaccharidosis and the impact of enzyme replacement therapy followed by hematopoietic stem cell transplantation at early age. Paediatr Anaesth. 24(5): 521-7.
- Moslehi MA (2022) Failures in emergency management of pediatric airway foreign bodies by rigid bronchoscopy: we have yet to complete our learning. World J Pediatr Sur. 5: e000321.