Gottsberger J. MD1*, Huber F. MD MSc.1#, Kurz F. MD2, Illek J. MD1, Schachner B. MD1, Zierer A. MD Prof.1
1Department of Cardiothoracic and Vascular Surgery, Johannes Kepler University, Linz, Austria.
2Department of visceral surgery, Johannes Kepler University, Linz, Austria.
#Florian Huber, MD MSc is corresponding author of this manuscript and has contributed equally to this work.
*Corresponding Author: Gottsberger J. MD, Department of Cardiothoracic and Vascular Surgery, Johannes Kepler University, Linz, Austria.
Abstract
Objective: Penetrating aortic ulcer (PAU), as a part of the acute aortic syndrome, by itself already represents a life-threatening condition. Surgical treatment of PAU involving the aortic arch remains a complex and challenging procedure. Furthermore, extensive PAU formation may cause oesophageal erosion over time, eventually leading to an aorto-oesophageal fistula, which represents a typically fatal clinical nightmare observation. Emergent interdisciplinary surgical management remains the only option. We present herein a successful case of a patient presenting with a ruptured aorto-oesophageal fistula originating from the aortic arch.
Methods: A 57-year-old female patient was hospitalized with the leading symptom of hematemesis and subsequent hemodynamic deterioration. Emergent imaging work up, including an acute gastroscopy, revealed a PAU-like bulging of the inner curvature of the aortic arch, causing oesophageal erosion. On a CT scan, a mass of hematoma and air pockets comprising the esophagus was detected within the mediastinum. Facing this devastating finding, we first performed a total aortic arch replacement employing the frozen elephant trunk technique with an Evita Open Neo prosthesis (E-vita OPEN Neo, Artivion/Cryolife, Hechigen, Germany) in Zone 2 performing an extra-anatomic left subclavian artery bypass grafting. Right at the end of the aortic arch replacement, the prolonged treatment of the oesophageal fistula was initiated by placing a percutaneous endoscopic gastrostomy and starting oesophageal endo-VAC therapy by our general surgeons. In a third step, the FET had to be extended downstream by thoracic endovascular aortic repair to cover all PAU-like alterations of the descending aorta.
Results: We are delighted to report that our patient recovered well and could be discharged home on post-OP Day 43 in a fully recovered fashion, including regular enteral nutrition. Proper pre-discharge CT scan and gastroscopy confirmed our successful therapeutic approach.
Conclusion: This case underlines the importance of an immediate interdisciplinary management of such extensive and otherwise fatal aorto-oesophageal pathologies.
Keywords: acute aortic syndrome, penetrating aortic ulcer, Porto-oesophageal fistula, total aortic arch replacement
1. Introduction
The penetrating aortic ulcer (PAU), as a part of the acute aortic syndrome, represents a critical and life-threatening condition with a high mortality rate. The incidence of the PAU is 7.5% of all aortic syndromes. Erosion of deeper layers of the aortic wall caused by a rupture of an atherosclerotic plaque is the underlying pathophysiological pathway. Penetrating atherosclerotic ulcer eroding into the esophagus is a rare case that can lead to an aorto-oesophageal fistula with a fatal outcome. [1,2]
Only a few cases of penetrating aortic ulcer complicated with an oesophageal fistula have been reported in the literature. The majority of these documented clinical nightmare scenarios ended fatally. [1,3] Due to the rarity and complexity of this pathology, there exist no clinical guidelines.
Against this background, we present herein a successful case of a patient presenting with a ruptured aorto-oesophageal fistula originating from the aortic arch.
2. Case report
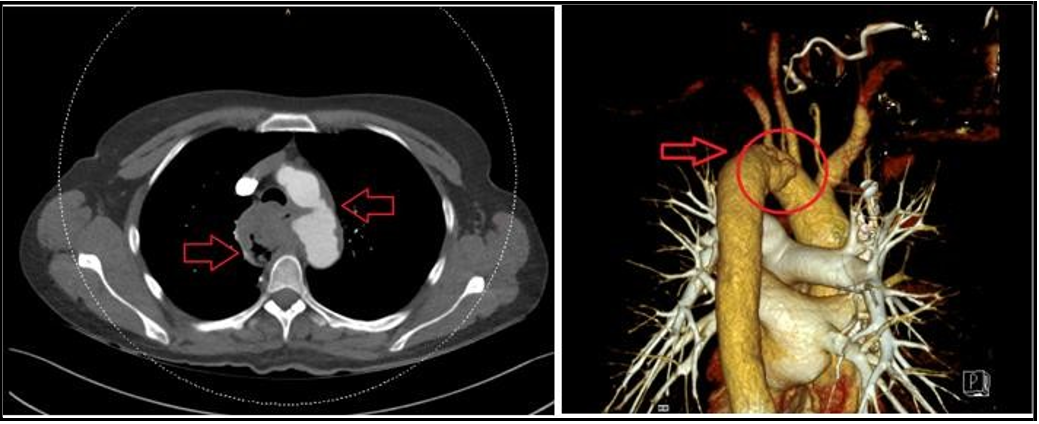
A 57-year-old female patient was hospitalized with the leading symptom of hematemesis and subsequent hemodynamic deterioration in November 2022. Emergent imaging revealed a PAU-like bulging of the inner curvature of the aortic arch. The CT scan showed an unclear 3x4cm mass in the mediastinum with air pockets as well as an ulcer-like bulging of the aortic arch and a poorly defined aortic wall (Figure 1). Due to hematemesis and the unclear defined mediastinal mass, there was suspicion of an oesophageal fistula.
Figure 1: Contrast enhanced CT scan prior surgery showing a mass of hematoma due to a ruptured PAU of the aortic arch.
Initially, it needed to be clarified where the problem was originating from. Either there was a covered rupture of a penetration aortic ulcer forming from the aortic arch, or oesophageal cancer has led to a perforation secondary causing an auto-intestinal fistula. Further endoscopic imaging added valuable information to the diagnostic process. Gastroscopy showed no malignant alteration of the esophagus, but a fistula and a mass of blood could be identified (Figure 2). Finally, we came to the diagnosis of a ruptured penetrating aortic ulcer leading to mediastinal hematoma. Second, this hematoma induced compression necrosis on the posterior wall of the esophagus, leading to an auto-intestinal fistula. Written informed consent could not be obtained because of the emergency.
Figure 2: Gastroscopy imaging of the upper GI showing a hematoma and the fistula after removing the blood.
Facing this devastating finding, we needed a clearly defined therapeutic strategy. First, we performed a total aortic arch replacement employing the frozen elephant trunk technique with an Evita Open Neo prosthesis (E-vita OPEN Neo, Artivion/Cryolife, Hechigen, Germany) during selective bilateral antegrade cerebral perfusion at 28 °C bladder temperature in Zone 2 performing an extra-anatomic left subclavian artery bypass grafting. After surgical treatment of the aortic arch pathology, an oesophageal endo-VAC therapy was initiated. This was mandatory for the prolonged healing of the fistula. As a further step, the FET had to be extended downstream by TEVAR to cover all PAU-like alterations of the descending aorta. A regression of the oesophageal fistula could be observed in regular endoscopic controls as part of the Endo-VAC changes. During the hospital stay, repeated swallow X-rays showed neither evidence of leakage nor continuity break.
We are delighted to report that our patient recovered well and could be discharged home on postoperative day 43 in a fully recovered fashion, including regular enteral nutrition. Proper pre-discharge CT scan and gastroscopy confirmed our successful therapeutic approach as well (Figure. 3).
Figure 3: (A) no evidence of leakage nor continuity break in the swallow x-ray, (B) Postoperative CT scan after aortic arch replacement revealing sufficient coverage of all PAU like alterations.
3. Discussion
The treatment of a penetrating aortic ulcer is a difficult task, and it is associated with high perioperative morbidity and mortality [4]. Particular locations of PAU, even in the aortic arch, need to be addressed surgically. Due to anatomical difficulties, surgical replacement of the aortic arch requires more extended perfusion and cardiac arrest time. Furthermore, there is a period of hypothermic circulatory arrest with cerebral perfusion for reimplanting the supra-aortic vessel. These facts are generally known for higher surgical mortality.
If the aortic arch pathology is associated with a fistulation to the esophagus, a well-considered therapeutic strategy is required to help the patient survive [5].
Despite various strategies for treatment, there needs to be more consensus regarding the best possible management of this pathology. To ensure a successful result, the surgical procedure should follow established principles for managing the aortic pathologies. After surgery or endovascular treatment of the aortic lesion, treatment of the esophageal lesion or fistula is mandatory. As in our case described, the usage of endo-VAC induced the healing of the fistula. Concluding from our case report, our repair consisted of two stages, which led to a success. First, it is essential to define the underlying etiology. As described, if the primary cause for the fistula is an aortic pathology, this must be addressed immediately. In a second step or simultaneously, it requires treatment of the intestinal lesion.
4. Conclusion
This case underlines the importance of immediate interdisciplinary management of such extensive and otherwise fatal auto-oesophageal pathologies.
List of abbreviations
PAU: Penetrating atherosclerotic ulcer
CT: Computer tomography
FET: Frozen elephant trunk
TEVAR: Thoracic endovascular aortic repair
Authors’ Contributions
All authors have made substantial contributions to the conception and design, have been involved in drafting the manuscript and revising it critically for important intellectual content, and have given final approval of the version to be published.
Conflict of Interest and Funding: Prof. Zierer is a proctor for ARTIVION and receives speaker fees from ARTIVION.
References
- Eggebrecht H, Plicht B, Kahlert P, Erbel R (2009) Intramural hematoma and penetrating ulcers: indications to endovascular treatment. Eur J Vasc Endovasc Surg. 38(6): 659-65.
- Evangelista Masip A (2004) Historia natural y tratamiento del síndrome aórtico agudo Natural history and therapeutic management of acute aortic syndrome. Rev Esp Cardiol. 57(7): 667-679.
- Chandrashekar G, Kumar VM, Kumar AK (2007) Repair of aortoesophageal fistula due to a penetrating atherosclerotic ulcer of the descending thoracic aorta and literature review. J Cardiothorac Surg. 2: 12.
- Dev R, Gitanjali K, Anshuman D (2021) Demystifying penetrating atherosclerotic ulcer of aorta: unrealised tyrant of senile aortic changes. J Cardiovasc Thorac Res. 13(1): 1-14.
- Lansman SL, Saunders PC, Malekan R, Spielvogel D (2010) Acute aortic syndrome. J Thorac Cardiovasc Surg. 140(6 Suppl): S92-7.