Terrell D. Coring, MD1, Asha Tipirneni, MD2, Hira Latif, MD3*, Deborah Topol MD4
1Medstar/Georgetown GME Department, Internal Medicine, MedStar Washington Hospital, Washington DC, USA
2Medstar/Georgetown GME Department, Hematology/Oncology, MedStar Washington Hospital, Washington DC, USA
3Medstar/Georgetown, Hematology/Oncology, MedStar Washington Hospital, Washington DC, USA
4Medstar/Georgetown, Internal Medicine, MedStar Washington Hospital, Washington DC, USA
*Corresponding Author: Hira Latif, MD, Medstar/Georgetown, Hematology/Oncology, MedStar Washington Hospital, Washington DC, USA
Abstract
Aims: To describe a case of Acyclovir-induced thrombocytopenia in a patient being treated for shingles where signs and symptoms presented as encephalopathy, which is underreported in the literature and often confused with worsening herpes encephalitis in clinical practice.
Case description: A 76-year-old male renal transplant recipient on immunosuppressive therapy recently diagnosed and treated for shingles with Acyclovir was admitted for encephalopathy.
The patient's labs on admission were significant for acute, chronic thrombocytopenia. The patient was initially started on IV acyclovir on admission due to concerns for VZV (Varicella Zoster Virus) encephalitis. However, his encephalopathy worsened, and the Acyclovir was discontinued. After ruling out other pathologies for the encephalopathy and thrombocytopenia, we concluded that his presentation was secondary to Acyclovir-induced thrombocytopenia. This diagnosis was initially missed; however, after withdrawing the offending agent, Acyclovir's platelets and mental status significantly improved.
Conclusion: Acyclovir-induced thrombocytopenia causing neurotoxicity may occur in someone with known renal disease, especially end-stage renal disease (ESRD) and renal transplant patients. This diagnosis is underreported in the literature and can be missed in elderly patients treated for shingles. The diagnosis can be confused with disseminated varicella-zoster causing encephalitis and worsening dementia on presentation. It is vitally important to recognize this diagnosis early and withhold Acyclovir for reversal of platelets and mental status.
Keywords: Drug-induced thrombocytopenia HSV- Herpes simplex virus ITP- Idiopathic thrombocytopenic purpura MAHA- Microangiopathic hemolytic anemia TTP- Thrombotic thrombocytopenic purpura VZV- Varicella zoster virus
Case Presentation
A 76-year-old male with a PMH of renal transplantation on immunosuppressive therapy, aortic stenosis s/p TAVR, IgA kappa MGUS, chronic leukopenia, thrombocytopenia, and anemia presented with complaints of shoulder pain and encephalopathy. The patient was recently hospitalized for acute uncomplicated herpes zoster infection where he has treated with Acyclovir 800 mg five times daily for five days. Although his rash had improved significantly, shoulder pain persisted in the area and was attributed to acute neuritis for which he was prescribed an additional five days of treatment with acyclovir. Upon presentation to the emergency room, he was afebrile and hemodynamically stable on room air. Physical examination was significant for waxing and waning mentation with persistent disorientation to time and place, but no focal neurologic deficits, diffuse ecchymoses along bilateral upper extremities, crusted vesicular lesions along his right upper extremity, and petechial rash along his right lower extremity. Lab work was notable for elevation in BUN 135 mg/dL and Cr 1.73 mg/dL compared to baseline Cr 1.10 mg/dL and slight increase in ALT 50 units/L and total bilirubin 1.5 mg/dL. Complete blood count showed a normal white blood cell count and hemoglobin and severe thrombocytopenia with a platelet count of 41 k/mL compared to a prior baseline of 90-100 k/mL.
Interventions/Investigations
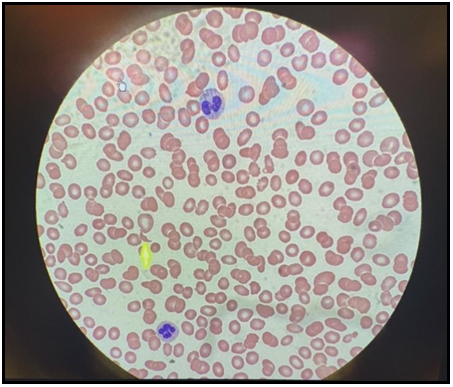
The differential diagnosis for persistent encephalopathy included disseminated herpes zoster, viral encephalitis, CVA, drug toxicity, and microangiopathic hemolytic anemia such as thrombotic thrombocytopenic purpura (TTP) or atypical hemolytic uremic syndrome (aHUS). Given the patient's elevated LDH, and decreased haptoglobin with elevated reticulocyte count, hematology was consulted but the review of the patient’s peripheral blood smear failed to reveal any clinically significant schistocytes per high power field and therefore was thought to be less likely etiology. Differential diagnosis was then turned to acyclovir-induced nephropathy and neurotoxicity for which both nephrology and infectious disease were consulted for further guidance and recommendations. Once MRI and CT head was found to be negative, the patient’s acyclovir was discontinued and he was transiently started on hemodialysis with improvement in both his mentation and thrombocytopenia during the course of his hospitalization. He did require a change in his immunosuppressive therapy from azathioprine to prednisone, as this was also thought to have contributed to his thrombocytopenia.
Figure 1: Photograph taken of patient right elbow demonstrating vesicular (blisters) lesions that are now crusted over due to shingles
Figure 2: Photograph taken of patient right foot and right ankle demonstrating petechiae due to thrombocytopenia
Figure 3: Peripheral blood smear showing one schistocyte labeled with the yellow arrow per high powered field
Discussion
Acyclovir-induced neurotoxicity is a rare complication of acyclovir therapy and is often difficult to distinguish from more common causes of encephalopathy such as encephalitis [1]. Since acyclovir is predominantly cleared by glomerular filtration and tubular secretion in the kidneys, patients with chronic kidney disease or renal impairment may be at a higher risk for this toxicity [2]. The most characteristic presenting symptoms are confusion, altered level of consciousness, hallucinations, agitation, and dysarthria and the main treatments include prompt discontinuation of antiviral and hemodialysis [3]. According to a systematic review of neurotoxicity associated with acyclovir and valacyclovir, the global mean of onset of symptoms was 3.1 days after the start of antiviral therapy, and the mean recovery time was 9.8 days [4]. Similarly, acyclovir-induced thrombocytopenia is a rare entity reported in the literature with only six published cases of acyclovir-induced immune thrombocytopenia [5,6,7,8,9,10]. Nevertheless, it was thought that this may have played a role in the pathogenesis of the patient's development of acute on chronic thrombocytopenia given to return to baseline platelet count within one to two weeks after medication cessation.
Conclusion
Our patient was being treated for zoster herpes with acyclovir 800 mg five times per day for a total of eight days before presenting with encephalopathy. He has been prescribed the correct dose based on his renal function see table 1 [11]. However, his age and history of renal transplantation made him at significant risk for acyclovir-induced thrombocytopenia [12]. There were only a handful of published cases illustrating acyclovir-induced thrombocytopenia within the literature; therefore, it is a rarely reported occurrence. The first step in treating acyclovir-induced thrombocytopenia is to discontinue the medication. In the reported cases, platelet levels increased by withholding the offending agent and without additional medication. It has been recommended in some reports to administer corticosteroids. However, its benefit has not been well established [5]. Other treatment options mentioned in the literature include platelet transfusions, intravenous IgG, and plasma exchange [5,13]. In our patient, after ruling out encephalitis as a cause for his encephalopathy and microangiopathic hemolytic anemia such as thrombotic thrombocytopenic purpura (TTP) or atypical hemolytic uremic syndrome (aHUS) as a cause for his thrombocytopenia; withdrawing the offending agent and one session of hemodialysis, improved both his thrombocytopenia and encephalopathy. Therefore, it is essential to recognize acyclovir-induced thrombocytopenia early and not confuse the diagnosis with encephalitis and worsening dementia in elderly patients. Holding the offending drug may drastically reverse the patient’s presentation.
Table 1. Acyclovir Dose Adjustments for Kidney Impairment [11]
|
CrCl |
Dose |
Dose |
Dose |
|
>50 mL/minute/1.73 m2 |
If the usual dose is 400 PO mg every 12 hours |
If the usual dose is 200 PO mg 5 times daily |
If the usual dose is 800 PO mg 5 times daily |
|
25 to 50 mL/minute/1.73 m2 |
No dosage adjustment necessary. |
No dosage adjustment necessary. |
No dosage adjustment necessary. |
|
10 to <25 mL/minute/1.73 m2 |
No dosage adjustment necessary. |
No dosage adjustment necessary. |
No dosage adjustment necessary. |
|
<10 mL/minute/1.73 m2 (not on dialysis) |
200 mg every 12 hours |
200 mg every 12 hours |
200 mg every 12 hours or 400 mg every 12 hours (severe infections) |
11 Zovirax (acyclovir) [prescribing information]. Research Triangle Park, NC: GlaxoSmithKline; January 2019
Authors Contribution:
All authors participated in drafting the case report and provided critical revisions for important intellectual content. All authors agree to be accountable for all aspects of the work and are confident in the integrity of co-authors' contributions.
Disclosures/Conflicts of Interest:
The authors do not have any disclosures/conflicts of interest.
References
- Chong BH (1991) Drug-induced immune thrombocytopenia. Platelets. 2(4): 173–181.
- King DH (1988) History, pharmacokinetics, and pharmacology of acyclovir. J Am Acad Dermatol. 18(1 Pt 2): 176–179.
- Yarlagadda SG, Perazella MA (2008) Drug-induced crystal nephropathy: an update. Expert Opin Drug Saf. 7(2): 147–158.
- Brandariz-Nuñez D, Correas-Sanahuja M, Maya-Gallego S, Martín Herranz I (2021) Neurotoxicity associated with acyclovir and valacyclovir: A systematic review of cases. J Clin Pharm Ther. 46(4): 918-926.
- Aster RH, Curtis BR, McFarland JG, Bougie DW (2009) Drug- induced immune thrombocytopenia: Pathogenesis, diagnosis, and management. J Thromb Haemost. 7(6): 911–918.
- Visentin GP, Liu CY (2007) Drug-induced thrombocytopenia. Hematol Oncol Clin North Am. 21(4): 685–696, vi.
- Aster R. Drug-induced thrombocytopenia. In: Michelson A, ed. Platelets. New York: Academic Press, 2006: 887-902
- Van Den Bemt PM, Meyboom RH, Egberts AC (2004) Drup- induced immune thrombocytopenia. Drug Saf. 27(15): 1243-52.
- Kaufman DW, Kelly JP, Johannes CB, Sandler A, Harmon D, et al. (1993) Acute thrombocytopenia purpura in relation to the use of drugs. Blood. 82(9): 2714-2718.
- Aster RH, George JN. Drug-induced thrombocytopenia. In: Mcrae K, ed. Thrombocytopenia. New York: Marcel Dekker Inc, 2006: 145-77
- Zovirax (acyclovir) [prescribing information]. Research Triangle Park, NC: GlaxoSmithKline; January 2019
- Sadjadi SA, Regmi S, Chau T. (2018) Acyclovir neurotoxicity in a peritoneal dialysis patient: report of a case and review of the pharmacokinetics of acyclovir. Am J Case Rep; 19: 1459–1462.
- Pourrat O. Treatment of drug-related diseases by plasma exchanges. (1994) Annales de Medecine Interne.;145(5):357-360