Madeeha Subhan Waleed1, Waleed Sadiq2, Sanniyah Subhan3 and Uzzam Ahmed Khawaja4, *
1Ayub Medical College, Abbottabad, Pakistan.
2Staten Island University Hospital, New York, USA.
3Oakton Community College, Illinois, USA.
4Jinnah Medical and Dental College, Karachi, Pakistan.
*Corresponding Author: Khawaja UA, Jinnah Medical and Dental College, Karachi, Pakistan
Abstract
Hyper igE syndrome, Jobs syndrome, Buckley Syndrome is a syndrome with increased igE levels and multiple abscesses in the body. Acquired von willebrand disease that is non inherited and is related to other disease processes in the body like myeloprofilertive disorders, autoimmune disorders or monoclonal gammopathy of undetermined significance. We present to you a case of a two-year-old girl with hyper igE syndrome with acquired von willebrand disease.
Keywords: jobs syndrome, von willebrand, dermatitis
Introduction
Hyper igE syndrome was first discovered in the year 1966 when they discovered an association between cold abscesses in the body and dermatitis thus naming it Jobs syndrome [1]. Six years after this child with multiple cold abscesses and dermatitis were discovered by Buckley hence naming it the Buckley syndrome [2]. Acquired von willebrand disease that is non inherited and is related to other disease processes in the body like myeloprofilertive disorders, autoimmune disorders or monoclonal gammopathy of undetermined significance. About one third of the reported cases are associated with a monoclonal gammopathy of uncertain significance (MGUS) [3-5] We present to you a case of a two-year-old girl with hyper igE syndrome with acquired von willebrand disease.
Case Presentation
The patient was a two-year-old girl brought to the hospital by her mother giving a history that the child had fever for two days that was intermittent and not associated with fever and chills. She was also having recurrent epistaxis and easy bruising since a year. The patient also had multiple tender swelling on her body. There was no discharge from the swelling. The patient had one swelling on the left side of the chest right below her nipple that was approximated 6×6 cm in size. The swelling was soft fluctuant, reducible, and tender. The second one was on the right arm measuring about 2×2 cm in size and was firm nonfluctuant,tender and not tranilluminating. The third swelling was on the left forearm measuring 1×1 cm and the fourth one on the left temple. Her lymph nodes were enlarged in the axillary inguinal and cervical region. Family history was negative for this condition. The patients mother gave history that the baby has penicillin allergy. Systemic examination was normal. Routine investigations were sent. Her chest X-ray ecg and echo were normal. Von willibrand factor antigen was less than the normal range. His Complete Blood picture and immunology report are shown in Table 1 and Table 2.
Table 1: Immunology report
|
|
Patient Levels |
Normal Levels |
|
IgG levels |
11.08 |
4.5-9.16 in 1-2 years of age |
|
IgA levels |
1.70 |
0.2-1 in 1-3years of age |
|
igE levels |
991.5 |
Less than 60 in 1-5years of age |
|
IgM levels |
2.98 |
0.19-1.46 in 1-3 years of age |
Table 2: Complete Blood Picture.
|
Hemoglobin levels |
6.9g/dl |
|
White blood cell levels |
22.15 X10^9/L |
|
Red blood cells level |
4.64 X10^12/L |
|
Platelet levels |
552 X 10^9/L |
Her peripheral smear showed Microcytic, hypochromic anemia with elliptocyes. Pus culture and sensitivity showed resistant Staphylococcus aureus (MRSA), sensitive linezolid and vancomycin and amoxicillin-clavulanic acid. An abnormal bleeding t ime of greater than 22 min and partial thromboplastin time (55 sec) were found. Following the venipuncture, she had developed a swelling in the right bicep’ s region.
Her CT scan showing abbesses as shown in Figure 1 and Figure 2
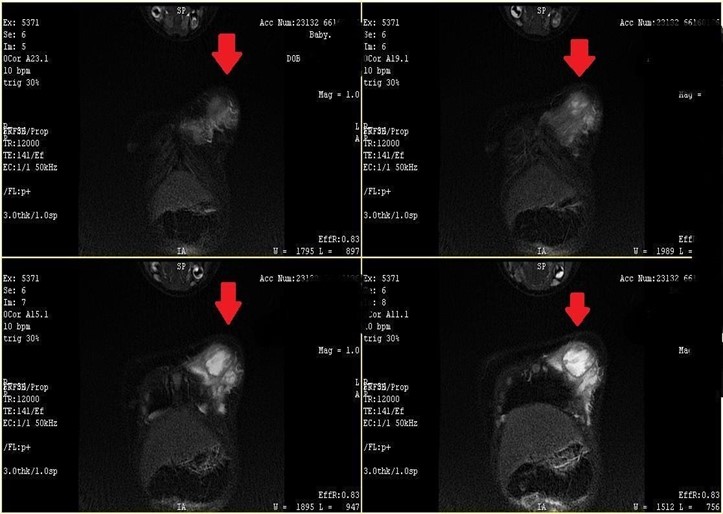
Figure. 1
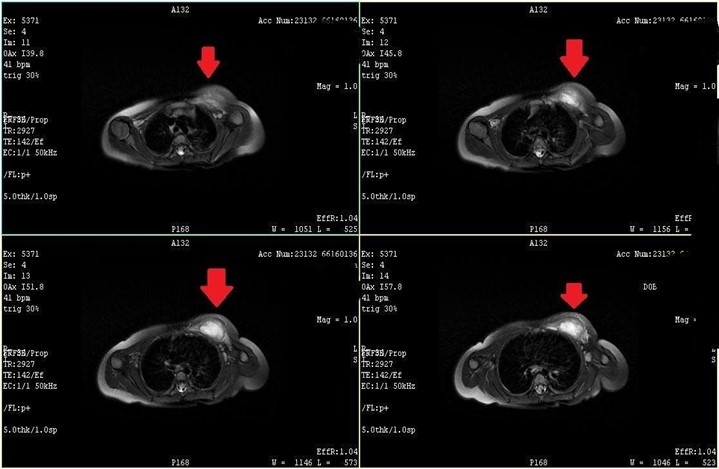
Figure. 2
Empirically amoxicillin was started along with iron supplements for her anemia and desmopressin concentrates for her von willibrand disease. The patient recovered in ten days and was discharged and was called for follow-up after a month. Her anemia had resolved.
Discussion
Hyper igE syndrome, Jobs syndrome or Buckley syndrome has increased IgE concentrations and defective neutrophil chemotaxis [6]. Hyper igE syndrome has been studies by Erlewyne-Lajeuness and Grimbacher and recently by Freeman and Holland [7, 8]. Acquired von willebrand disease is a disease that is due to another disease process and is not inherited. Acquired von willibrand syndrome is rare, with a prevalence of 0.04 % in the general population [9]. Treatment of Jobs syndrome is antistaphylococcal spectrum antibiotics such as penicillin and cephalosporins’ [10].
References
- Davis SD, Schaller J, Wedgwood RJ (1966) Job's syndrome: Recurrent, "cold" staphylococcal abscesses Lancet 1: 1013- 1015.
- Buckley RH, Wray BB, Bellmaker EZ (1972) Extreme hyperimmunoglobulinemia E and undue susceptibility to infection. Pediatrics 49(1); 59-70.
- Freeman AF, Holland SM (2009) Clinical manifestations, etiology and pathogenesis of the hyper-IgE syndromes. Pediatr Res 65(2): 32-37.
- Jakway JL (1992) Acquired von Willebrand’s disease. Hematology Oncol Clin North Am 1409-1419.
- 11.Rinder MR, Richard RE, Rinder HM (1997) Acquired von Willebrand’s disease: A concise review. Am J Hematol 54: 139-145
- Hill HR, Ochs HD, Quie PG, Clark RA, Pabst HF, et al. (1974) Defect in neutrophil granulocyte chemotaxis in Job's syndrome of recurrent "cold" staphylococcal abscesses. Lancet 304(7881): 617-619.
- Hill HR, Quie PG (1974). Raised serum IgE levels and defective neutrophil chemotaxis in three children with eczema and recurrent bacterial infections. Lancet.303(7850): 183- 197.
- Grimbacher B, Holland SM (2005) Puck JM. Hyper-IgE syndromes. Immunol Rev 203: 244-250.
- Federici AB (2006) Acquired von Willebrand syndrome: an underdiagnosed and misdiagnosed bleeding complication in patients with lymphoproliferative and myeloproliferative disorders. Semin Hematol 43(1l)
- Tanaka H, Ito R, Onodera N, Waga S (1998) Efficacy of long- term sulfamethoxazole-trimethoprim therapy in a boy with hyperimmunoglobulin E syndrome. Tohoku J Exp Med 186: 61.



