Melike Ruşen Metin1 , Hasan Aydın2*
1TC.SB.Ankara Bilkent City hospital Radiology Department, Ankara-Turkey
2TC.SB.Ankara Oncology Research hospital Radiology Department, Ankara-Turkey
*Corresponding Author: Hasan Aydın, TC.SB.Ankara Oncology Research hospital Radiology Department, Ankara-Turkey
Abstract
Bone, lungs, liver, and brain were the most frequent sites of metastasis of breast cancer. In this case, we present a rectum, Gastrointestinal system(GIS) metastasis of the breast cancer which was very rare and infrequent. 61 years old female who was diagnosed and treated as invasive lobular carcinoma(ILC) T1N3M0 16 years ago, had a complaint of tenesmus for 6 months. After MRI, Colonoscopy, and histopathology yields, Rectum metastasis of ILC was confirmed. As a result, ILC metastasis of GIS and rectum should be included in the differential diagnosis of patients with prior breast cancer history and with atypic MRI findings for primary colorectal cancer.
Keywords: Tumor, cancer, metastasis, MRI
Introduction
Bone, lungs, liver, and brain were the most frequent sites of metastasis of breast cancer [1-3] Invasive ductal carcinoma was the most seen and most metastatic type of breast cancer with inflammatory carcinoma(ca.) [2-4].GIS metastasis of breast cancer, especially colon metastasis were extremely rare [1,3-5]. In this case, we present a rectum metastasis of breast cancer, ILC which was very rare and infrequent.
Case report
A 61-year-old female with a complaint of tenesmus for 6 months, was admitted to the Gastroenterology department and had a history of ILC with radical mastectomy performed 16 years ago. ILC with ring cell pleomorphic differentiation and T1N3M0 staging was confirmed histopathologically. Tamoxifen was administered for 5 years (Between 2003-8) and Zoladex for 2 years (2006-8). The tumor was 4 cm in size and revealed an extra-capsular spread.
In the colonoscopic evaluation; A mass lesion that covered the rectum peripherally, was discovered and multiple biopsies were taken. In the MRI; This mass was originated from anal verge and it was not delineated from anal sphincters and mesorectal fascia, the mass continued about 9 cm which involved the middle and distal rectal segments invaded all rectal wall and luminal structures, prolonged to the presacral and perirectal adipose tissues. It crossed over the rectovaginal diaphragm on the left anterolateral side and was very close to the posterior wall of the vagina, the mass showed intense heterogeneous contrast enhancement, low ADC levels regarding high cellularity with an infiltrative thickened rectal wall (Figure1,2).
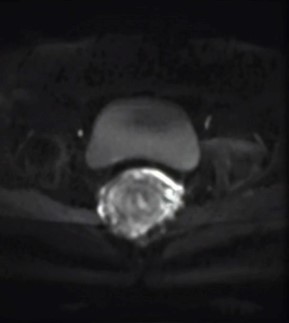
Figure 1: In the axial FS-T2W sequence; Rectal mass was slightly hyperintense with a heterogenous appereance.
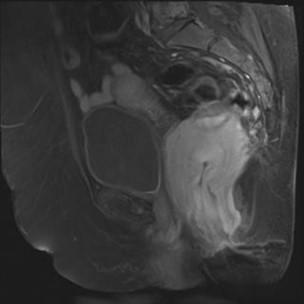
Figure 2: In the FS-T1W contrast-enhanced sequence, Mass was hyperintense with heterogeneous enhancement, invaded all rectal walls, and protruded to the perirectal fat plains No extra-mural vascular invasion was found out with a couple of lymph nodes in the pre-sacral interval, not exceeding 5 cm in size.
In the left adnexal region, a 5.5 cm well-circumscribed cyst with invisible thin Wall enhancement was seen. A lytic metastatic bone lesion was identified in the L5 vertebral corpus, PET-CT revealed high FDG-18 uptake in this lesion (SUV max.5.5) and also high uptake in the rectum(SUV max 6.0). No more hypermetabolic foci in the body, regarding malignancy, was not identified in this PET-CT.
In the histopathologic examination; Atypic cells with a hyperchromatic nucleus and infiltrative eosinophilic cytoplasm were discovered in the rectal mucosa and serosa. In the immunohistochemical essay; PanCK (+), LCA (-), CD79a (-), CDX2(-), Mammoglobin (+) and ER (+). Histomorphologic findings were consistent with metastasis of breast cancer (Figure 3).
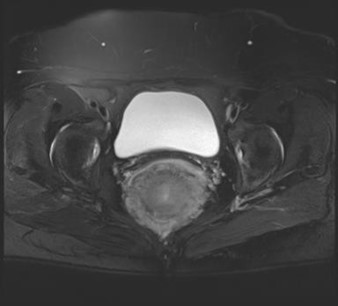
Figure 3: In the sagittal T2W sequence, Mass was iso-hyperintense and invaded mostly the posterior Wall of rectum and predicted luminal narrowing.
Discussion
The most common breast cancer was invasive ductal ca., but nevertheless, ILC had increasing incidence(1-3).ILC was mostly seen between 57-65 years of age [2,3,5]. The most common sites of metastasis of ILC were bones (% 65), lung (% 31.4), liver (% 26), and brain (% 8.5), at least % 33.5of all lobular ca. presented multiple organ metastasis [3,4]. The most common invaded bones were Vertebral corpus, bony pelvis, femur, and humerus [5]. In our case, a lytic sclerotic metastatic lesion was discovered at the L5 vertebral body. GIS metastasis of breast cancer was extremely rare and mostly to the stomach, small intestine, and colon [6]. GIS metastasis of ILC was higher than invasive ductal ca. (% 8-14) [1-3,7].
In research with 206 cases of GIS metastasis of breast cancer, only % 7 rectum metastasis was presented [8]. Matsuda et al. [9] reported 73 GIS metastasis of breast cancer in 2500 patients and only 24 patients had colorectal metastasis throughout those patients, regarding only % 1. In the relevant literature, GIS metastasis of ILC was defined as mass lesions like Lynitis plastic which proceeded to the diffuse and peripheral thickening of bowel Wall, shown in endoscopic and radiological imaging, some lesions might predict themselves as inflammatory bowel diseases [9-11].
In our case, different MRI findings in the rectum were found out that was not consistent with Rectum ca; A colonic mass that invaded all rectal walls with diffuse and/or concentric patterns, and to our experience, this appearance might belong to Colonic lymphoma or inflammatory bowel diseases, but however, this mass revealed restricted diffusion and low ADC levels revealed hypercellularity. GIS metastasis of breast cancer was the first diagnosis after MRI and DWI-ADC imaging results in addition to the ILC history and radical mastectomy. Lau et al[11] also presented the same results in their ILC case.
As a result; Rectum metastasis of breast cancer was extremely rare and in our case, She had a radical mastectomy 17 years ago with prior ILC diagnosis regarded rectal mass lesion which was consistent with ILC metastasis and confirmed histopathologically. Lytic and sclerotic L5 vertebral bone metastasis was also discovered after 17 years.
In conclusion, In the differential diagnosis of such mass lesions in the patients with anamnesis of breast cancer, GIS metastasis of breast cancer had to be in minds, especially in the patients without any pathognomonic MRI findings, consistent to the primary colorectal ca. In the MRI; the Typical finding of GIS metastasis of breast cancer was the invasion of all rectal walls by the mass.
Author contributions
Melike Rusen Metin: Case organisation, figure design, manuscript style, and reference listing.
Acknowledgment: The authors have no conflict of interest
Hasan Aydın: English editing and manuscript writing, figure captions design, co-author presentation and organisation of e-mails.
References
- Arrangoiz R, Papavasiliou P, Dushkin H, Farma JM (2011) Case report and literature review: metastatic lobular carcinoma of the breast an unusual presentation. Int J Surg Case Rep. 2(8): 301- 305.
- Balakrishnan B, Shaik S, Burman-Solovyeva I (2016) An Unusual Clinical Presentation of Gastrointestinal Metastasis From Invasive Lobular Carcinoma of Breast. Journal of Investigative Medicine High Impact Case Reports. 4(2): 2324709616639723.
- Chen M-T, Sun H-F, Zhao Y, Fu W-F, Yang LP, et al. (2017) Comparison of patterns and prognosis among distant metastatic breast cancer patients by age groups: a SEER population based analysis. Scientific Reports. 7: 9254
- Fisher B, Redmond C, Dimitrov NV, Bowman D, Legault-Poisson S, et al. (1989) A randomized clinical trial evaluating sequential methotrexate and fluorouracil in the treatment of patients with node-negative breast cancer who have estrogen-receptor-negative tumors. N Eng J Med. 320(8): 473-8.
- Aaron AD (1997) Treatment of metastatic adenocarcinoma of the pelvis and extremites. J Bone Joint Surg Am. 79(6): 917-932
- Winston CB, Hadar O, Teitcher JB, Caravelli JF, Sklarin NT, et al. (2000) Metastatic lobular carcinoma of the breast: patterns of spread in the chest, abdomen, and pelvis on CT. AJR Am J Roentgenol. 175(3): 795-800.
- Borst MJ, Ingold JA (1993) Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery. 114(4): 637–641.
- Ambroggi M, Stroppa EM, Mordenti P, Biasini C, Zangrandi A, et al. (2012) Metastatic breast cancer to the gastrointestinal tract: report of five cases and review of the literature. Int J Breast Cancer. 2012: 439023.
- Matsuda I, Matsubara N, Aoyama N, Hamanaka M, Yamagishi D, et al. (2012) Metastatic lobular carcinoma of the breast masquerading as a primary rectal cancer. World J Surg Oncol. 10: 231.
- Cherian N, Qureshi NA, Cairncross C, Solkar M (2017) Invasive lobular breast carcinoma metastasising to the rectum. BMJ Case Rep. 2017: bcr2016215656.
- Lau LC, Wee B, Wang S, Thian YL (2017) Metastatic breast cancer to the rectum. A case report with emphasis on MRI features. Medicine. 96(17): e6739.



