Vineet V Mishra1*, Smit B Solanki2, Kunur Shah3, Rohina Aggarwal4, Sumesh Choudhary4
1Professor and Director, Head of Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
2Assistant Professor, Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
3Associate Professor, Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
4Professor, Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
*Corresponding Author: Vineet V Mishra, Professor and Director, Head of Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
Abstract
Halted distal extension of the Müllerian ducts, either complete or segmental, can result in outflow tract obstruction. We hereby report a case of agenesis of the uterine isthmus and the technique to create the neo-isthmus for the outflow tract. A 20-year-old girl with cyclic pelvic pain and primary amenorrhea was found to have a separate uterine cavity and the cervix with no connecting isthmus in between uterus and cervix. The cervical-uterine anastomosis was performed via laparotomy and postoperatively she had normal painless menstruation. Thus, such cases of Müllerian duct anomaly can be corrected by primary anastomosis and establishing anatomical normality. Our ultimate objective is to restore menstruation and preserve future fertility.
Keywords: Mullerian duct, agenesis, neo-isthmus, cervical-uterine anastomosis, laparotomy
Introduction
A 20-year-old nulligravida was referred for a Müllerian anomaly, and she presented with primary amenorrhea and cyclical pelvic pain. The pelvic MRI showed agenesis of the uterine isthmus. After primary anastomosis of the uterine corpus to the cervix, she achieved normal menstruation and was pain-free. The incidence rate of genital malformation is nearing 5 % in recent times [1]. This is a very rare and compound Müllerian anomaly. The Embryological and Clinical Classification by Acién [1] and a paper discussing congenital anomalies of the uterine cervix by Rock et al. [2] address it properly. This anomaly is described as segmental type because in our case cervix was present and there was an abrupt end of the uterus which was not having any communication with the cervix.
Case Report
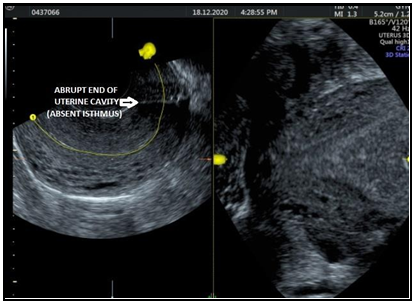
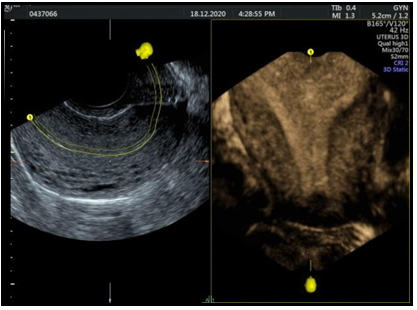
A 20 years old unmarried patient came to our hospital with primary amenorrhea and history of cyclical abdomen pain every 30 days. Diagnostic hysteroscopy revealed cervical stenosis. She was operated on for diagnostic hysteroscopy which showed a 3.5cm cervix, which was blind at the upper end and uterine cavity could not be negotiated. She was averagely built and averagely nourished. She was vitally stable. Her laboratory investigations were within normal limits. MRI was suggestive of the Possibility of non-communication between the right uterine horn with the cervix showing hematocolpus and hematometra and aplastic agenesis of the left uterine horn. Diagnostic Hyster laparoscopy was suggestive of bilateral mild hydrosalpinx and isthmic atresia. Transabdominal sonography was showing Right ovary shows 29 x29mm and 21 x 21 mm ovarian cysts; left sidehydrosalpinx showing 5.3 x 2.7 cm collection. Transvaginal sonography showed anteverted uterus, endometrial thickness 8.6mm, cervix and vagina appear to be normal, no communication between cervix and uterus (Figure 1). Right ovary was 3.6 x 3.6 cm hemorrhagic cyst, 2.3 x 1.8cm hydrosalpinx, 2.1 x 1.5cm clear cyst, 2.2 x 1.6 cm hemorrhagic cyst. The left ovary had a 5.2 x 3.1 cm tub ovarian mass and the left ovary was not separately identified from Tubo ovarian mass. 3D USG showed an abrupt end of the lower part of the uterus (Figure 2). No connection between the lower part of the uterine cavity and cervix. Examination under general anesthesia was done which showed normal urethral anatomy, hymen, cervix, and vagina. On Per vaginal examination, uterus was felt on the right side. On left side, mass was felt suggestive of hydrosalpinx or ovarian cyst.
Laparotomy was done under general anesthesia and no isthmus was created with malecot’s catheter for uterocervical anastomosis. The uterocervical anastomosis was done after a low transverse incision. The abdomen was opened in layers. Haemoperitonium - was drained out. Uterus was globular, bilateral round ligaments were normal. Bilateral fallopian tubes showed hematosalpinx. Bilateral ovaries showed ovarian cysts, upper segment was normal and isthmus was absent. After identifying uterovesical fold, the bladder was retracted. A vertical incision was kept on the uterus and hematometra was drained out. Dilator was passed between lower segment and bladder at proposed site of isthmus. From below, anterior lip of cervix was caught and artery forceps was introduced to peritoneal cavity. Incision was kept from the peritoneum side of the area of the proposed site of the isthmus. The anterior surface of the uterus was sutured with the upper border of the anterior lip of the cervix and the posterior surface of the uterus was sutured with the upper border of posterior lip of the cervix. Stepwise closure of abdomen was done. Postoperatively, the patient was painless. She was called for follow-up.
Figure 1: Transvaginal Sonography
Figure 2: 3D TVS
Discussion
Uterine isthmus agenesis is a rare type of Mullerian anomaly. The clinical presentation and treatment for Mullerian malformations are primarily directed to the anatomy of the defect. In the reported case, the patient was 20 years old female with amenorrhoea and cyclical abdomen pain. Patients with Mullerian malformations may be asymptomatic or may present with amenorrhoea, or cyclical pelvic pain. There is no particular etiology behind these malformations. It may be either environmental or genetic. Some of the factors causing malformation are Ionizing radiation, infections, Chemicals, immunologic disturbances, hormonal abnormalities, nutritional factors, etc. One method to label the deficit is by associating the ratio of the cervix to the uterine body – in young girls, the body of the uterus is only half as long as the cervix. But the above criteria, though, may not be relevant to a uterus with hematometra. An alternative method is to compare the development of the cervix to the developmental anomaly that is not likely to have a normal size and appearance. The size and appearance of this patient’s cervix were normal: it measured 3 cm on the basis of transvaginal sonography and sounding; and appeared normal on vaginoscopy. These explanations suggest that the isthmus is the most likely anatomical deficit. We found one case report describing a similar, but not identical, uterine anomaly: a 15-year-old girl had a 3 cm gap between uterus and cervix.[3] She presented with cyclic pelvic pain and amenorrhea. After primary anastomosis using the laparoscopic and hysteroscopic approach, menstruation started, and the individual was pain-free. Histological examination of the caudal end of the uterine body showed myometrium and endometrial glands. During second-look surgery, the site of anastomosis did not allow a probe to pass. The above case and our case differ in how the uterine body and the cervix were connected. The reported case was by a 3 cm gap: in our case, by a fibrous band. However, they have an identical embryological origin. There is a theory of the development of the female reproductive tract which shows the Wolffian ducts (as controller basics) and the female gubernaculum induce the fusing and growth of the uterus.[4] Therefore, an irregularity of any (or both) leads to different anomalies affecting the uterus, including segmentary defects. The exact cause leading to the reported malformation remains to be explained. Our technique of anastomosis maintained normal anatomy, linked two structures that may have differences in inner and outer diameters, maintained tight closure of the defect, and maintained even closure. Normal communication between the cervix and the uterus is likely to produce normal functions, including menstruation, fertility, and pregnancy. To achieve pregnancy, we mention that the patient should be monitored properly antenatally for incompetent cervix and preterm labor, and cesarean delivery. Describing this rare anomaly, a separate category should intensify consciousness and enable optimum invasive and operative correction, which can lead to symptom relief and normal reproductive function.
Conclusion
Isthmus agenesis is a very rare Mullerian anomaly that we encountered. We constructed “neoisthmus” via laparotomy approach successfully following which the patient was relieved from pain and gained normal menstruation. Thus, Mullerian anomaly can be effectively managed with surgical correction.
Acknowledgments: We are thankful to our librarian Ms. Jyotsana Suthar for her help in literature search for preparation of manuscript.
Financial support and sponsorship: Nil.
Conflicts of interest: There are no conflicts of interest.
References
- Acien P, Acien MI (2011) The history of female genital tract malformation classifications and proposal of an updated system. Hum Reprod Update. 17(5): 693-705.
- Rock JA, Roberts CP, Jones HW Jr. (2010) Congenital anomalies of the uterine cervix: lessons from 30 cases managed clinically by a common protocol. Fertil Steril. 94(5): 1858-63.
- Richards A, Phy JL, Huang JC (2018) Primary cervico-uterine anastomosis in a patient with agenesis of the uterine isthmus: A case report and review. J Obstet Gynaecol Res. 44(12): 2199- 2203.
- Acien P, Sanchez del Campo F, Mayol MJ, Acien M (2011) The female gubernaculum: Role in the embryology and development of the genital tract and in the possible genesis of malformations. Eur J Obstet Gynecol Reprod Biol. 159(2): 426-432.