Sanjiya Arora1*, Ajay Singh2, Sandesh Dhakal3, Sachin Mahendrakumar Chaudhary4, Abdul Khalid Qadree5, Sushmita Pandey6, Kausar Bano7
1Department of Medicine, Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh, India.
2Department of Medicine, Sri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India.
3Department of Medicine, College of Medical Sciences, Bharatpur, Nepal.
4Department of Medicine, Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India.
5Department of Pathology, Caribbean Medical University, Willemstad, Curaçao. PIN code: 4797.
6Department of Medicine, Nepal Medical College, Jorpati, Kathmandu, Nepal.
7Katihar Medical College, Katihar, Bihar, India
*Corresponding Author: Sanjiya Arora, Department of Medicine, Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh, India.
Abstract
Kikuchi-Fujimoto disease (KFD), also known as histiocytic necrotizing lymphadenitis, is benign, sneaky, and uncommon. We present the case of a 29-year-old Indian male patient who presented with chills, a sore throat, joint discomfort, and an evening fever that lasted for several days. There was a slight rise in liver enzymes, an accelerated ESR, and slight leukocytosis. In the histological examination of the node, almost total preservation of its architecture was observed, with cortical and paracortical hyperplastic changes. Following the administration of NSAIDs, the patient displayed clinical remission. The prognosis for KFD is favorable, and most cases get better in a few months. However, diagnosing this rare condition is still challenging for the medical community, and histological studies are critical.
Keywords: histiocytic necrotizing lymphadenitis, lymphadenopathy, acute reactive hepatitis, hepatosplenomegaly.
Introduction
Kikuchi-Fujimoto disease (KFD), also known as benign histiocytic necrotizing lymphadenitis, is rare. Although most cases have been documented in Asia, this disease has been characterized globally since it was first identified in Japan in 1972 [1,2]. Although both genders are affected by this disease, young women with a mean age of 20 to 30 years predominate [3-5]. The most common clinical symptom is posterior cervical lymphadenopathy, which occasionally involves axillary and supraclavicular lymph nodes. Most patients experience additional symptoms such as fever, weight loss, nausea, vomiting, weakness, headache, arthralgia, night sweats, upper respiratory tract symptoms, and sore throat [6].
Though the genesis of KFD has been proposed to be associated with a heightened immune response to underlying pathogenic agents or mediated by autoimmunity, the actual cause of this illness remains unknown [1,2]. As mentioned earlier, a variety of therapeutic options have been suggested for those affected by the disorder, including administering antipyretics and non-steroidal anti-inflammatory drugs to patients exhibiting characteristic symptoms. However, some experts in the field state that treatment with corticosteroids, immunoglobulin, hydroxychloroquine, or combination therapy is the choice in those cases where symptoms become atypical and refractory to conventional treatment [7,8]. Because it is a disease with slight clinical suspicion, which can lead to the misdiagnosis of other more frequent conditions, its diagnosis continues to be challenging for the medical community, and histological studies are essential to rule out other possible causes.
Case presentation
29 years old Indian male with a history of health. 17 days before admission, he started experiencing chills, a sore throat, frontal headache, joint discomfort, general malaise, and an evening fever between 38 and 39 degrees Celsius. Notably, in addition to losing weight and getting exhausted quickly. Physical examination revealed a reddened oropharynx with enlarged tonsils, no exudates or adenopathies in the proper lateral chain of the neck, and 1.5 cm-diameter submaxillae that were not painful on palpation, had a firm, movable consistency, a smooth surface, and were not attached to deep planes. Lymph nodes with similar characteristics were identified in the left submandibular region. It was agreed to indicate laboratory testing and to decide on hospitalization.
Table 1: Laboratory test details of the patient on admission
|
Hemoglobin |
16.2 (Normal range = 13.2-16.6 g/L |
|
Hematocrit test (Hct) |
42 (Normal range = 41-50 %) |
|
Erythrocye sedimentation rate (ESR) |
85mm/h (Normal range = 1-13mm/h) |
|
Leukogram |
10.9x109/l |
|
Polymorphonuclear leukocytes |
76 % |
|
Lymphocytes |
24 % |
|
Blood glucose |
5.5 mmol/L (Normal range = 2.8-3.9 mmol/L) |
|
Creatinine |
77 µmol/L (Normal rangr = 61.9-114.9µmol/L) |
|
Alanine aminotransferase (ALT) |
104 IU/L (Normal range = 0-44 IU/L) |
|
Aspartate aminotransferase (AST) |
94 IU/L (Normal range = 8-48 IU/L |
|
Gamma -glutamyl transpeptidase (GGT) |
40IU/L (Normal range = 0-30 IU/L) |
|
Oropharyngeal swab |
Negative |
|
Urine culture |
No bacterial growth |
|
VDRL serology |
Negative |
|
HIV serology |
Negative |
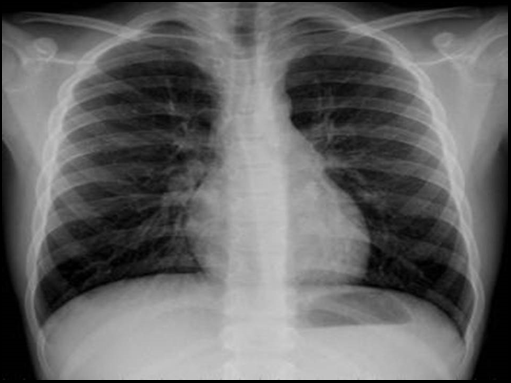
Neck ultrasonography revealed several adenopathies, the largest measuring 18 x 11 mm and being highly vascularized (Figure.1). A second adenopathy with comparable characteristics was also found in the left submandibular region, raising the possibility of an oncoproliferative process. Rest of structures without alterations. No pleuropulmonary abnormalities on the chest X-ray (Figure.2). Normal cardiothoracic index—unchanged electrocardiogram. Sinus rhythm with a steady axis (Figure 3). Acute reactive hepatitis was evident on the liver biopsy.
Lymph node biopsy is noted when the surgical specimen is examined under a microscope: 2.5 x 1.2 x 0.8 cm ovoid tissue formation with a smooth surface, congested regions, and fibroelastic consistency (Figure 4). Uniform dark-brown surface when cut. With cortical and paracortical hyperplastic alterations, its architecture was almost entirely preserved. Interfollicular, paracortical, and well-defined geographic zones were interspersed. They are composed of cells with moderate cytoplasm, transparent eosinophils, round to oval nuclei, loose chromatin, and not particularly visible nucleoli, as well as a lot of nuclear remnants without polymorphonuclear cells when observed at high magnification (Figure 5).
Immunophenotype: Membranous CD 20 positive in almost 100 % of the cells of the pathological clear area, CD 3 negative in these areas, CD 68 negative in these cells, and intense cytoplasmic positive in the histiocytic cells at the interface of the pathological area with the hyperplastic lymphoid tissue.
The case is concluded as Benign histiocytic necrotizing lymphadenitis. Non-steroidal anti-inflammatory medication therapy was initiated. The patient makes a satisfactory recovery, is released from the hospital, has outpatient follow-up, and remains asymptomatic.
Figure 1: Ultrasonography revealing adenopathies in the neck region.
Figure 2: Chest X-ray showing the absence of pleuropulmonary abnormalities.
Figure 3: Electrocardiogram with steady sinus rhythm
Figure 4: Microscopic examination of the surgical specimen revealing ovoid tissue formations.
Figure 5: Paracortex expansion, increased histiocytes and plasmacytoid dendritic cells with karyorrhectic nuclear debris.
Discussion
KFD often develops slowly and progresses in a benign, self-limiting manner. More young women of Asian descent are affected. However, some studies alert the scientific community to the prevalence in children [3,5]
Although the cause of KFD is uncertain, the condition has been linked to autoimmune disorders and viral infections [2,6]. All this favors other infectious agents such as toxoplasmosis, Brucella, Bartonella henslae, Yersinia enterolitica, viruses such as human herpes, Ebstein rod virus, parainfluenza, paramyxovirus, parvovirus B19, and cytomegalovirus; are related to this disorder. The association with systemic lupus erythematosus, Still's disease, Wegener's granulomatosis, Graves' disease, and Sjogren's disease has also been suspected [10]. Most patients have nonspecific clinical manifestations such as lymphadenopathy, fever, and less common symptoms, including night sweats, nausea, vomiting, diarrhea, stiff neck, skin manifestations, weight loss, and lymph node involvement from another location [8].
Lymph nodes, usually single or multiple, painful, preferably bilateral, can appear in any area, although more frequently in the cervical, supraclavicular, submandibular, and axillary lymph node chains. High and lingering fever can occur either before or after lymph node enlargement. Patients commonly have many diffuse arthralgias without arthritis, as well as asthenia, sweating, nausea, vomiting, diarrhea, and chills. Inflammation of the eye has been linked to it, and this inflammation might appear years after lymph nodes. Sometimes, the condition affects the skin and shows up as a rash. The time that elapses from the onset of symptoms to diagnosis varies from one to 24 months [9-11]. The physical examination is usually standard, except for the lymph node involvement mentioned. However, in a small percentage of instances, hepatosplenomegaly is present.
Although nonspecific abnormalities are occasionally observed, such as minor neutropenia, thrombocytopenia, leukocytosis, atypical lymphocytosis, discrete changes in liver enzymes, and elevated lactic dehydrogenase enzyme and ESR, laboratory tests are typically standard. Positive viral serologies and positive autoantibodies can occur sometimes [4].
Depending on where the afflicted nodes are located, the findings have radiological similarities to salivary gland tumor pictures and branchial cysts and lymphomas. An ultrasound reveals several larger nodules and a collection of hypoechoic lymph nodes. It should be noted that pathological investigation is presently used to diagnose this condition, necessitating a biopsy of the afflicted lymph node [11]. The presence of foci or cell nodules in karyorrhexis and eosinophilic necrosis, primarily in paracortical regions, are common histological findings. Phagocytic histiocytes can be seen in these nodules, which are absent of neutrophils and have areas of hyperplasia of monocytic cells, plasmacytoid cells, immunoblasts, tiny lymphocytes, and apoptotic cells. These hyperplastic foci can be mistaken for lymphomas. Three histological subtypes of the illness have recently been identified: proliferative, necrotizing, and xanthomatous [11]. Immunohistochemical studies have shown that the immunoblastic reaction almost exclusively involves cells of the T lineage, that the evolution of the disease is accompanied by a change in the ratio of helper T lymphocytes (CD 4) and suppressor lymphocytes (CD 8), with a decrease in the latter [11]
Regardless of the cause of this disorder, the therapeutic approach is similar in all cases.
Due to their efficacy and cheapness, non-steroidal anti-inflammatory drugs are the treatment of choice [4,7]. The administration of corticosteroids and hydroxychloroquine is reserved for cases with recurrent KFD [4].
Studies suggest that KFD has a favorable prognosis and that most cases resolve within a few months [3,4].
Diagnosing this disease is still a challenge for the medical community, and histological studies are essential to rule out other possible causes of lymphadenopathy.
References
- Bolaños-Aguilar MA, Celis-Vera KD, Barragán-Garfias JA, Orrantia-Vértiz M, Duarte-Mote J (2018) Kikuchi-Fujimoto disease, manifestation together with siliconosis. Rev Med Int Mex. 34(2): 335-41.
- Castro Corredor D, de Lara Simón IM, Bellido Pastrana D (2018) Kikuchi-Fujimoto disease: evolution in outbreaks with response to antimalarials. Rev Esp Patol [Internet]. 51(1): 34-6.
- Salamat S, Chan J, Jolly K, Powell G, Harrison K, et al. (2020) Kikuchi-Fujimoto Disease and Prognostic Implications. Head Neck Pathol. 14(1): 272-275.
- Nizamuddin, Aamer U, Waheed, Farishta (2020) Arthritis as a Presenting Feature of Kikuchi-Fujimoto Disease: Time to Think Out of the Box in Patients with Arthritis. Hamdan Medical Journal. 13(1): 55-56.
- Shabana M, Warnack W (2020) An atypical neurologic complication of Kikuchi-Fujimoto Disease. Neurol Neuroimmunol Neuroinflamm. 7(3): e707.
- Perry AM, Choi SM (2018) Kikuchi-Fujimoto Disease: A Review. Arch Pathol Lab Med. 142(11): 1341-1346.
- Sharma K, Otieno F, Shah R (2020) Case Report of Kikuchi- Fujimoto Disease from Sub-Saharan Africa: An Important Mimic of Tuberculous Lymphadenitis, Case Reports in Medicine. 2020: 6.
- Raposo André D, Vicente F, Chaves J, Caldeira M, Jacinto F, et al. (2020) Kikuchi-Fujimoto Syndrome: A Rare Entity to Consider. Eur J Case Rep Intern Med. 7(7): 001456.
- Kim JE, Lee EK, Lee JM, Bae SH, Choi KH, et al. (2014) Kikuchi-Fujimoto disease mimicking malignant lymphoma with 2- [(18)F] fluoro-2-deoxy-D-glucose PET/CT in children. Korean J Pediatr. 57(5): 226-31.
- Sarfraz S, Rafique H, Ali H, Hassan SZ (2019) Case Report: Kikuchi-Fujimoto Disease: A case of supraclavicular lymphadenopathy. F1000Res. 8: 1652.
- Sukswai N, Jung HR, Amr SS, Ng SB, Sheikh SS, et al. (2020) Immunopathology of Kikuchi-Fujimoto disease: A reappraisal using novel immunohistochemistry markers. Histopathology. 77(2): 262-274.