Maryam Haroon*
WMO at THQ hospital tehsil kot radha khishan, District Kasur.
*Corresponding Author: Maryam Haroon, WMO at THQ hospital tehsil kot radha khishan, District Kasur.
Abstract
Introduction
Joint pain and swelling with abdominal aches are the initial presentation of many Rheumatological Diseases and Metabolic disorders, such as Hemochromatosis. However, Infections, either bacterial or viral, should always be considered an important differential diagnosis.
Mycobacterium Tuberculosis is the second most common cause of Musculoskeletal Osteomyelitis, an infrequent entity accounting for 1.5 to 3 percent of all TB cases, occurring more often in young individuals and detected in later stages of the disease, predominantly affecting epiphysial and subchondral regions of bone. Occasionally, it disseminates to other body viscera and systems. We at this moment present a case of a 16- year-old girl who explained to us with joint pain along with affected joints swelling for 9 months. In addition, she had abdominal pain in the same period in association with fever and weight loss for a few months. All baseline investigations were regular except for increased ESR and CRP. Autoimmune and ENA profiles were average. Among radiological investigations, USG's abdomen and pelvis were consistent with moderate pelvic ascites and normal musculoskeletal USG in all swollen joints. CT CAP scan showed axillary Lymphadenopathy and Pelvic Ascites. MRI scan of severely inflamed right knee joint with and without contrast studies couldn't lead to a satisfactory diagnosis. SPECT/CT scan of the same joint was performed, and studies highlighted Lytic lesions on the proximal tibial bone that were AFB positive on Microbiological analysis. The histopathological evaluation further confirmed the benign but Tuberculous Nature of the lesions. The purpose of this case report is to elaborate on an atypical aspect of the clinical presentation of Musculoskeletal TB, often misdiagnosed as seronegative arthritis or malignancy. Sometimes, it is due to a lack of definite radiological findings. A delay in initiating ATT would lead to secondary dissemination to other body systems.
Case presentation
We report a case of a 16 years old Asian girl who had joint pain and swelling for a duration of 9 months along with fever and weight loss in association with abdominal pain of the same duration with no significant past medical and surgical as well as personal history except having positive contact with pulmonary TB in the family. ESR and CRP were raised. X-ray and Musculoskeletal skeletal USG of all affected joints didn't show abnormal findings. On abdominopelvic ultrasonography, moderate pelvic ascites were found (exudative, lymphocytic on diagnostic ascetic paracentesis) with no visceral enlargement or lymphadenopathy. CT CAP revealed nodal enlargement in the axillary area of one side of the body with pelvic ascites. MRI studies of actively inflamed right knee were not directed towards a reasonable diagnosis. SPECT/CT of the same joint revealed lytic lesions of proximal tibial bone; could it be malignant? After a CT-guided biopsy of suspicious lesions, specimens were sent for microbiology and histopathological examination. Finally, AFB smear staining was positive. Meanwhile, growth was detected on AFB culture as ++×. ATT started instantly, and the patient's symptoms began improving within weeks.
Conclusion
In adults with Musculoskeletal TB, Mycobacterium rarely affects joints (both small and large joints in asymmetric patterns). Sometimes, Tuberculous arthritis occurs secondary to the extension of underlying TB osteomyelitis of bones involved in joint formation. If aggressive, then earlier spread to other body systems like reticuloendothelial system, etc. Lymphadenopathy and ascites in the above case are signs of secondary dissemination of primary bone TB. However, all signs and symptoms will be settled once ATT has started.
Keywords: Tuberculous Osteomyelitis, ESR, CRP, CT CAP, SPECT/CT, Lytic lesions, AFB, Gene Xpert / MTB-RIF assay, Excisional biopsy, ATT.
Introduction
Evaluation of patients presenting in the medical outdoors with joint pain and swelling in association with abdominal aches would lead a clinician to take into consideration a vast list of differential diagnoses. Many Rheumatological conditions, especially seronegative arthritis, can present in this way, but the duration of symptoms from onset to progress would not be so long; on the other hand, abdominal pain (which might be due to mesenteric vasculitis) is less frequent, especially when the patient first comes across medical specialist's opinion. Metabolic derangements are consistent with the predominant hepatobiliary spectrum of symptoms with secondary involvement of the Musculoskeletal system in the form of either degenerative arthropathy or pseudogout. Other possibilities are Infections (bacterial or part of SIR's phenomenon secondary to Viral causes) and malignancy. Commonest bacterial Infections are TB (tuberculosis) and brucellosis. We present a case of 16 a 16-year-old girl who presented with a gradual onset of joint pain along with joint swelling. The pain was additive and dull in nature. Joints were affected asymmetrically, with predominant swelling of the right knee and the left index finger's DIP joint, worsening from a few weeks and not relieved with analgesics. She had a fever (high grade) and progressive weight loss in association with abdominal discomfort. Laboratory parameters showed raised serum inflammatory markers. Critical radiological investigations were done, and their findings were highlighted above and will be further explained below. Results of biopsy specimens of lytic lesions showed on SPECT/CT of the right knee were analyzed by a Microbiologist and Pathologist; AFB was found positive on smear staining. Gene Xpert/MTB-RIF assay, as well as AFB C/S, were positive. Meanwhile, anti-tuberculosis therapy started, and as a result, symptoms improved instantly.
Case presentation
A 16-year-old girl presented in the medicine outdoor department of a regional teaching hospital with complaints of joint pain and swelling for the last 9 months. Gradual onset is asymmetric, progressive instead of additive, starting from the right knee joint and then extending to the costosternal joints of the right lower rib cage and the distal interphalangeal joint of the left index finger. Initially, pain improved partially on oral analgesics, but with time, it became persistent and worsened in the last few weeks. She had a high-grade fever max. She was recorded up to 101 to 102 degrees Fahrenheit with no rigors/chills but malaise, fatigue, body aches, and progressive unintentional weight loss of about 6 kgs in the past months. There is no evidence of morning stiffness, the gelling phenomenon of joints after activity, or improvement in arthralgias with exercise, body rash, oral ulcers, hair loss, photosensitivity, frothing of urine, headache, vomiting, shaking movements of any part of the body, and altered behavior.
Also, the diffuse dull abdominal ache of an identical duration, spontaneous, remained static, improved instantly without any medication, did not radiate or shift, and had no urinary complaints or altered bowel habits. There is no history of lumps and bumps in the body, but they had disturbed sleep, decreased appetite, and amenorrhoea. At presentation, her vital signs were typical, with RBS 100 mg/dl and Sao 99 percent at room air. She was alert and conscious, with a GCS of 15/15. General and systemic examinations were regular. On Musculoskeletal system examination, her right knee joint was slightly erythematous, warm, and tender but mobile with a reduced range of movement in all planes (due to pain). The rest of the joints appeared normal. The left index finger was found to swell distally, but there was no pain in movement.
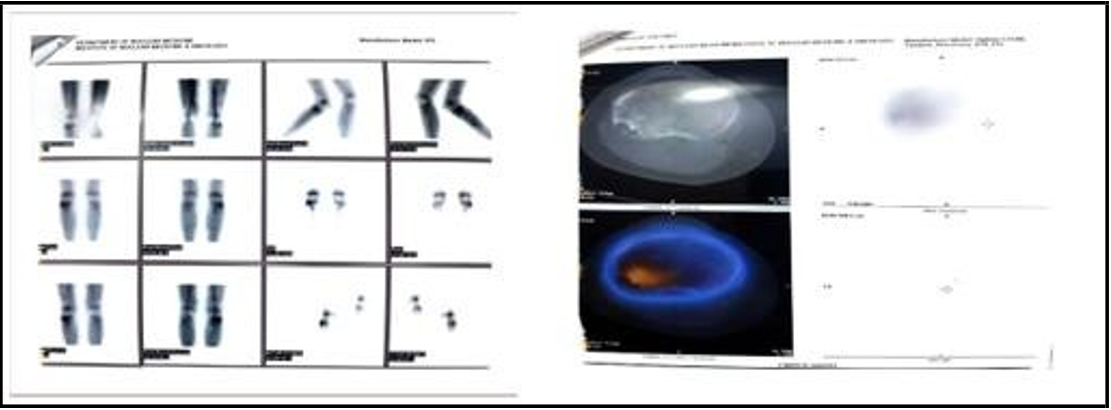
On complete blood count, Hb: 10.9, MCV: 70, WBCs: 5000, PLTs: 256000. ESR: 56mm/hr, CRP: 33.36mg/L. RFTs, LFTs, S/E, TSH, serum viral markers, LDH, serum total Protein, urine complete exam, RA factor, autoimmune, and ENA profiles were normal. Chest X-ray and affected joints X-ray were normal except for the right knee, which showed soft tissue swelling and the periosteal reaction of proximal tibial and distal femoral epiphyses. USG abdomen and pelvis showed moderate pelvic ascites (lymphocytic as 70 percent of WBCs were lymphomas, exudative with SAAG ratio of 0.9, total fluid protein approximated up to 3g/dl on diagnostic ascetic paracentesis) but no visceral enlargement or lymphadenopathy. Musculoskeletal USG of all affected joints was normal except the right knee, where it was found to have biceps femoris bursitis (1.5 cc debris collection). On further investigation, a CT CAP scan revealed right-sided axillary lymphadenopathy, the largest lymph node measuring 9cm, along with pelvic ascites. The patient and her family refused FNAC access to the axillary node.
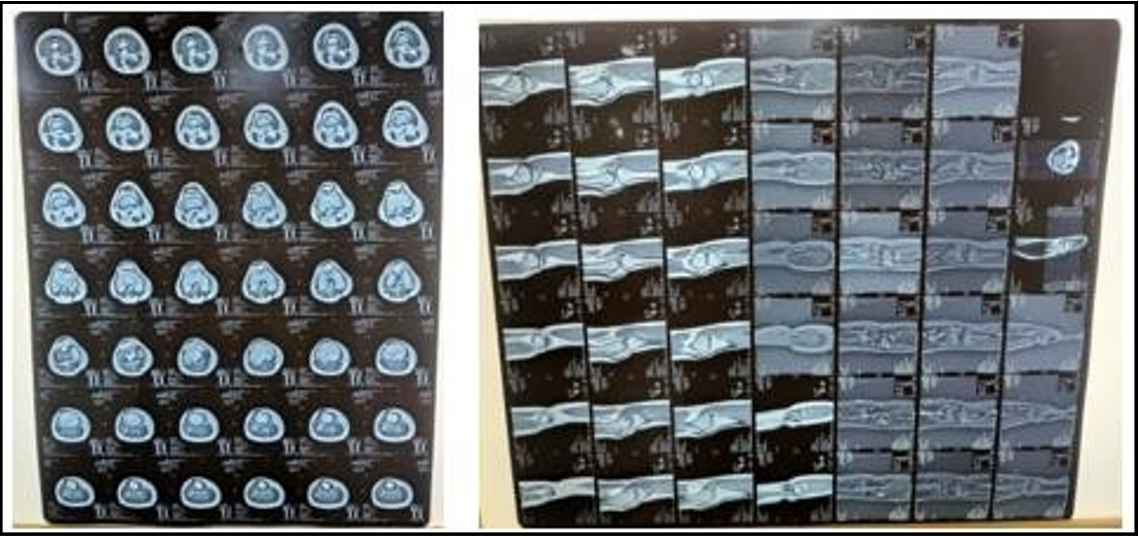
To clarify the diagnosis, an MRI scan of the right knee (with and without contrast studies) was performed. Findings were consistent with expensive tibial epiphysial lesions on T1W, heterogeneous on T2W, and hyperintense on STIR but were insufficient to lead to some authentic radiological diagnosis of peculiar lesions. To find the hidden primary or underlying focus of sepsis, a SPECT/CT scan is planned. At this time, lytic lesions in the proximal tibial bone were found with surrounding erythema. CT-guided biopsy was performed, and specimens were sent for Microbiological examination and histopathological evaluation. AFB smear staining turned out to be positive, along with positive AFB C/S. No RIF resistance on Xpert MTB-RIF assay was detected.
X-ray images of right knee joint;
Arrow head showed soft tissue swelling whereas periosteal reaction of bones epiphyses is obvious.
MRI images of right knee joint
SPECT/CT SCAN of right knee joint with three D images of lytic lesions
Discussion
Joint pain as well as swelling along with abdominal pain are common complaints of patients coming to the medical outdoor department of public or private hospitals. [1] Though it seems to be simple, in reality, both are broad manifestations of many underlying diseases, rheumatological conditions, and metabolic derangements. [2] When associated with fever and weight loss, infections would be significant possibilities.[3] With advancement in Microbiological and Radiological techniques and easy access to Pathologist’s services, now it’s possible to diagnose chronic infections earlier before irreversible damage has occurred. [3]
Malignancy (primary/secondary) will always be at the bottom of the list of D/D. [4] In our society, like other resource-limited regions of the world, Tuberculosis is still endemic despite regional and national public awareness campaigns every year about modes of TB transmission while simultaneously encouraging implementation and enforcement of DOTs program for TB control around the country. In recent years, many surveillance programs have been initiated by the health sector in the countryside, ensuring adequate screening of people and patient contacts for active TB either through questionnaires or, in the case of LTBI, by a rapid, cost-effective blood test (IGRA) to minimize TB burden. Unfortunately, due to the new trend of polypharmacy, as can be appreciated in IV drug users and the increased prevalence of HIV infection in our society, MDR-TB has become a significant health problem among communities. [5]
The case presented above differs from the typical presentation of musculoskeletal tuberculous, which includes Pott’s disease (most common). Another joint presentation is tuberculous arthropathy. [5] Due to the rare but unique oligoarticular pattern of involvement, TB Osteomyelitis can be confused with autoimmune/ seronegative arthritis, especially in the context of patient age. [6] So lack of timely management of bone TB may result in dissemination of primary disease to other body systems, thus enabling patients to have a variety of symptoms including abdominal pain as an essential association. [7]
Conclusion
Though painful swollen joints and abdominal pain commonly present complaints of patients coming across Medical, Rheumatological, and ID outdoor departments, it might be rare, an atypical manifestation of Tuberculous Osteomyelitis with secondary dissemination.
Musculoskeletal TB mostly has non-discriminative findings on radiological investigations despite the indolent and a bit aggressive nature of the disease. However, if one strongly suspects that patients have tuberculous arthritis in the context of disease endemicity, ATT should be started empirically. Waiting for the results of specified investigations will increase patients' misery.
Informed Consent
Written informed consent was obtained from the patient's legal guardian for the publication of the manuscript and accompanying images. The editor-in-chief of the respected journal has a copy available for review.
Abbreviations
ESR: Estimated sedimentation rate
CRP: C-reactive Protein
ATT: Anti-Tuberculosis therapy
CT CAP: Computed tomography scan of chest abdomen and pelvis
C/S: Culture and sensitivity
ID: Infections diseases USG: Ultrasonography
SPECT/CT: Combination of Single-Proton Emission computed tomography scan with CT scan
MTB: Mycobacterium tuberculosis
RIF: Rifampicin
DD: Differential diagnosis MDR: Multi-drug resistance
DOTs: Directly observed therapy
IGRA: interferon-gamma release assay.
References
- Vohra R, Kang HS, Dogra S, Saggar RR, Sharma R (1997) Tuberculous osteomyelitis. J Bone Joint Surg Br. 79(4): 562-6.
- Till SH, Snaith ML (1999) Assessment, investigation, and management of acute monoarthritis. J Accid Emerg Med. 16(5): 355-61.
- Yap J (2023) Tuberculous arthropathy: Radiopaedia.
- Wallace R, Cohen AS (1976) Tuberculous arthritis: A report of two cases with review of biopsy and synovial fluid findings. The American Journal of Medicine. 61(2): 277-282.
- UF Health (2023) Tuberculous arthritis.
- Santos HC, Henriques AR, Branco JC, Machado P, Canhão H, et al. (2023) In a community-based setting spondyloarthritis patients report higher levels of physical disability than chronic low back pain patients-results from EpiReuma. pt. ARP rheumatology. 2: 97-110
- Weissman BN (2009) In: Imaging of Arthritis and Metabolic Bone Disease.