Yan Xu1*, Weiming Tang1, Jingjing Wang2
1Department of Clinical Laboratory, Liyang People's Hospital
2Department of Clinical Laboratory, Huashan Hospital, Fudan University
*Corresponding Author: Xu yan, Department of Clinical Laboratory, Liyang People's Hospital.
Abstract
Introduction: Fungal urinary tract infections have been on the rise in recent years, Candida is the most common. Candida urinary tract infections in symptomatic outpatients are rare. Further tests are needed to determine the type of Candida and target treatment.
Case presentation: When survey the cause of the patient's repeated fever, we found a urinary tract infection caused by Candida, and the Candida is Candida krusei (rare opportunistic pathogen). This case shows us how opportunistic bacteria cause disease.
Conclusions: It is necessary to identify the type of candida infection. The treatment of symptomatic urinary tract infections is of great significance.
Keywords: fever; Candida; fungal urinary tract infection
Introduction
Candida krusei is a relatively rare but important opportunistic pathogenic candida in clinical practice. At first, it is thought that Candida krusei is a human symbiotic bacteria with low pathogenicity and virulence. But in recent years, the clinical infection caused by it occurs frequently and is paid more and more attention. Compared to Candida albicans, Candida krusei is weak in virulence. But it has a strong adhesion, it can be attached to non-biomass surfaces, along with catheters, implants and other materials into the body, then it causes oral, urogenital and systemic infections in patients with immune dysfunction. Candida krusei can cause fatal systemic candidiasis. It is commonly seen in patients with congenital immune deficiency. It can also occur in patients receiving high doses of antibiotics or immunosuppressants [1].
Case report
A 34-year-old female outpatient presented with recurrent fever, no other discomfort, the highest temperature is 38℃. Every time a fever occurs, the routine blood test shows elevated white blood cells, consider "bacterial infections". One month ago, she developed wandering joint pain. Her temperature improved after she was given cephalosporin or levofloxacin in an external hospital. A week later, the temperature began to change again, then went to our hospital for examination: blood routine examination: normal; routine urine examination: leukocyte esterase: 1+, nitrite : negative, PH: 5.5, bacterial count: 2211.3/ml; others: erythrocyte sedimentation rate (ESR), immunoglobulin, rheumatism three tests、absolute count of lymphocyte subsets、serum amyloid A protein(SAA), these are all normal.
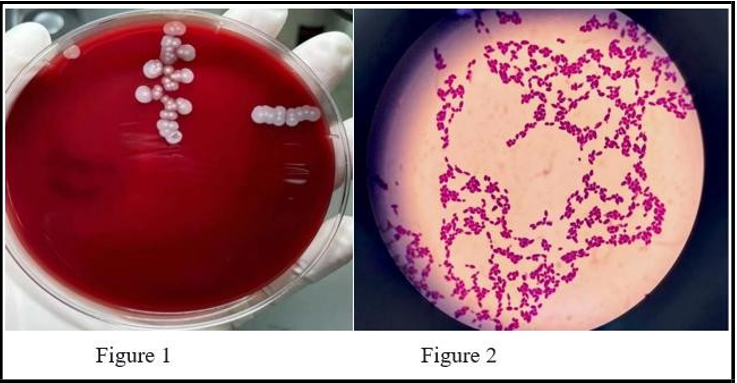
A urine culture was performed according to the results of the urine routine examination: after 48h of blood plate culture, white irregular and flat colonies were found (See Figure 1). Gram-positive, ovoid and cylindrical bacteria were detected by gram staining on colony smear (See Figure 2). According to the experience and the identification result of the time-of-flight mass spectrometer, the final determination was Candida krusei.
Discussion and conclusions
More than 95% of urinary tract infections are caused by a single bacterium. Among them, 90% of outpatients and about 50% of inpatients, the pathogen is Escherichia coli. Fungal, mycoplasma and other infections are rare, but there has been an upward trend in recent years[2]. There is currently no clinical evidence of any benefit from antifungal treatment in the absence of signs and symptoms of urinary tract infections[3]. So some scholars[4] consider that diagnosis should be made in conjunction with clinical symptoms when microorganisms are found in urine specimens. Most of the asymptomatic bacteriuria is not recommended to use antibiotic treatment.
The first midstream urine in the morning is used as far as possible to prevent contamination from causing false positives. Fungal urinary tract infection may be asymptomatic, or only pyuria, or there may be typical manifestations of urinary tract infection, and even renal failure. Candida urinary tract infection is common, Candida is an opportunistic pathogen. Only in the long-term placement of urinary catheters, the body's resistance to decline or candida overgrowth, will become pathogenic bacteria. Urine nitrites are very specific for urinary tract infections but are not always present in the setting of urinary tract infections [5].
Furthermore, not all uropathogenic bacteria produce nitrites, giving nitrates a poor sensitivity for ruling out urinary tract infections. In addition, leukocyte esterase has a high sensitivity for urinary tract infections[6]. In this case, the patient urine white blood cells were normal, nitrite was negative —— indicate a small chance of bacterial infection. The optimal PH for candida growth was 5.1 to 6.4, and the patient's urine PH was 5.5, which was favorable for candida growth. If a fungal urinary tract infection is highly suspected, it is best to inoculate Sabouraud's Agar with urinary sediment to prevent missed detection. When patients have susceptibility factors for fungal infection, such as long-term urinary catheter retention, diabetes, long-term use of antibacterial drugs or immunosuppressive drugs[7], symptoms of urinary tract infection or no urinary symptoms, but urine white blood cells and lymphocytes are mainly, and the bacterial culture is negative, special attention should be paid to whether there is a possibility of fungal infection, and it is very important to actively conduct standardized fungal culture.
Case Review
The patient underwent surgery for breast nodules and chocolate cysts and had no history of drug allergy. One month after surgery, she repeatedly developed unexplained intermittent fever accompanied by wandering arthralgia. Combined with the above factors, it is highly suspected that urinary tract infection is an infection caused by intraoperative hematogenous dissemination.
This case serves to explore the importance of accurate diagnosis in the laboratory. It can indicate the direction of clinical diagnosis and treatment so as to provide appropriate treatment for patients. The correct identification of candida species and in vitro susceptibility to the main antifungal agents are important for the success of treatment[8]. Therefore, it is very important to standardize the operation of laboratory technicians and improve the level of business.
References
- Tingying Z, Qiangqiang Z. Clinical microbiology diagnosis and diagramming, the 4th edition, 2017: 688-689.
- Timm MR, Russell SK, Hultgren SJ (2025) Urinary tract infections: pathogenesis, host susceptibility and emerging therapeutics. Nat Rev Microbiol. 23(2): 72-86.
- Dias V (2020) Candida species in the urinary tract: is it a fungal infection or not?. Future Microbiol. 15: 81-83.
- Deng R, Meng X, Li R, Wang A, Song Y (2023) Asymptomatic Candida glabrata urinary tract infection in an immunocompetent young female A case report. Medicine (Baltimore). 102(20): e33798.
- Millner R, Becknell B (2019) Urinary Tract Infections. Pediatr Clin North Am. 66(1): 1-13.
- Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management; Roberts KB. (2011) Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 128(3): 595-610.
- Timm MR, Russell SK, Hultgren SJ (2025) Urinary tract infections: pathogenesis, host susceptibility and emerging therapeutics. Nat Rev Microbiol. 23(2): 72-86.
- Sharma K, Parmanu PK, Sharma M (2024) Mechanisms of antifungal resistance and developments in alternative strategies to combat Candida albicans infection. Arch Microbiol. 206(3): 95.