Anna Ekin, MScBr, MD1*, Jian Yang, MD1, Nada Al-Hashimi, MD1
1The Department of Family Medicine, The Brooklyn Hospital Center, Brooklyn, NY 11201
*Corresponding Author: Anna Ekin, MScBr, MD, The Department of Family Medicine, The Brooklyn Hospital Center, Brooklyn, NY 11201
Abstract
A patient from Brooklyn, New York, was diagnosed with Plasmodium falciparum malaria after traveling to Africa. Here we emphasize that malaria is still considered the leading cause of mortality and morbidity in the developing world as well as the importance for clinicians to screen for and prepare patients that travel to high-risk areas for malaria, as transmission could easily be prevented with chemoprophylaxis and counseling.
Introduction
Malaria is a disease caused by a plasmodium parasite transmitted by the Anopheles mosquito [1]. There are five subtypes of malaria: Plasmodium falciparum, Plasmodium ovale, Plasmodium malaria, Plasmodium vivax, and Plasmodium knowlesi. In the United States, only about 2,000 malaria cases are diagnosed annually [2]. Plasmodium falciparum is considered the most severe and fatal of the five subtypes. Symptoms first appear 10 to 15 days after being bitten by an infective female Anopheles mosquito. Untreated
P. falciparum malaria can progress to severe illness and death [3]. Here we present a patient who had visited Africa, had not taken or been placed on any malaria chemoprevention, and showed symptoms during her stay.
Case report
A 65-year-old female living in Brooklyn, New York, with no significant past medical history, presented to the Emergency department with fever, weakness, and poor appetite for 3 days. Social history was necessary for my one-week travel to Cameroon, Africa, and I arrived back in New York on July 3, 2022. The patient stated that she had one episode of vomiting during her stay in Africa, with occasional subjective fever. She could not tell if it was constant, intermittent, or cyclic. The madness was partially relieved with acetaminophen and lasted one week. She denied any vaccinations before travel or taking any chemoprophylaxis before, during, or after her trip. The patient said she stayed at her friend’s house and drank water from the local supply. She also confesses that she traveled with colleagues and that they presented similarly, but upon further discussion, once she was admitted to inpatient, the patient denied any friends or colleagues that traveled with her.
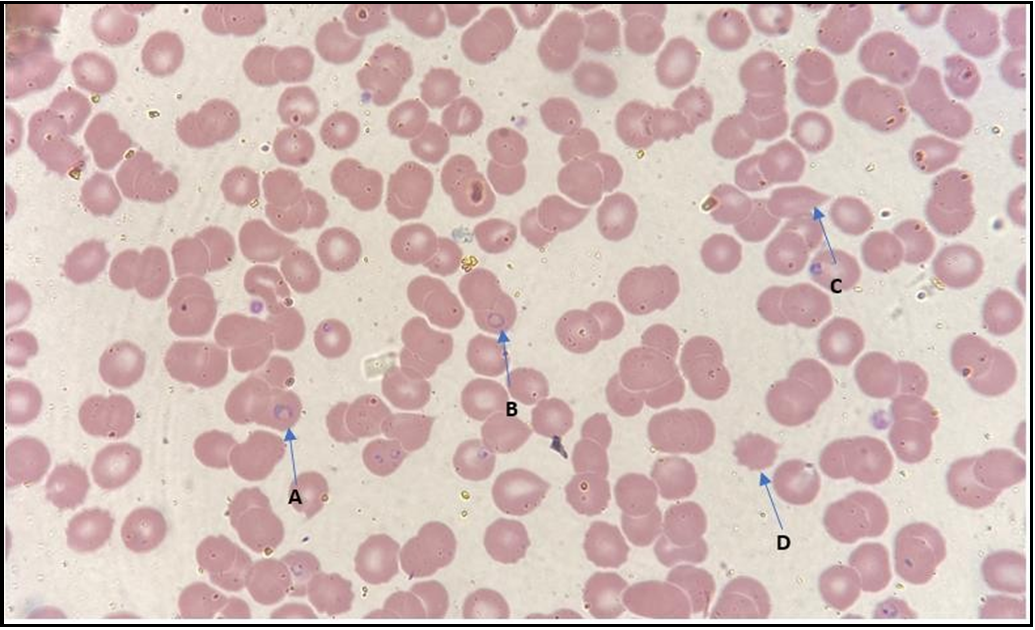
On physical exam, she appeared well-developed and not in acute distress. Vital signs are stable with a blood pressure of 100/67 mmHg, pulse rate of 97 beats/minute, and temperature of 37.7°C. Physical examination was notable for 1+ pitting edema up to the knees in bilateral lower extremities, and the rest of the physical exam was benign. Laboratory results showed a hemoglobin/hematocrit level of 11.8/35, and RBC morphology showed ovalocytes 1+, teardrop cells 1+, poikilocytosis 1+, and spherocyte 1+; thrombocyte count of 55 x 109/L, and giant platelets, a leukocyte count of 7.9 x 109 cells/L with mild lymphopenia of 18.4 %, LDH 880 U/L, creatinine/BUN of 1.9mg/dL/37mg/dL, AST of 97 U/Land ALT of 81 U/L. Peripheral blood smear showed P. falciparum-infected erythrocytes with a parasitemia index of 10.10%. (Figure 1). The right upper quadrant ultrasound was unremarkable. Chest radiograph showed mildly increased vascular markings.
Figure 1: 1A. & 1B. Falciparum rings, 1C. Tear drop cell, 1D. Echinocytes
Treatment and Hospital Course
The patient was admitted inpatient for a total of 7 days. Due to the high suspicion of malaria, the patient was initially treated with Mefloquine, Doxycycline, and Ceftriaxone. The patient was transitioned to Artemether/Lumefantrine once malaria was confirmed. She was treated with IV fluids and anti-pyrectics for cyclic fevers. The patient continued to improve, and follow-up malaria smears were negative. The species of plasmodium resulted on day 7, confirming P. falciparum. The patient was discharged on Doxycycline for an additional 7 days.
Conclusion
The WHO has recently updated its malaria prevention recommendations, including three crucial malaria prevention stages. The three stages are seasonal malaria, perennial malaria, previously known as an intermittent preventive treatment in infants, and intermittent preventive treatment of malaria in pregnancy (IPTp)[4][5]. In some areas, malaria is seasonally dependent and occurs mainly during the rainy season, whereas malaria has high transmission year-round in other countries. In Cameroon, Africa, malaria prevalence depends on temperatures ranging from 24 to 26 C and rainfall rates of approximately 4 to 6 mm per day [6]. The new recommendation is less stringent on the number of doses and an expanded age range at which malaria chemoprevention can be given. The 2010 recommendations recommended three doses to be presented at the specific ages of 2, 3, and 9 months of age [4]. Lastly, malaria in pregnancy poses risks to the mother and fetus and should therefore be avoided if possible. Malaria chemoprevention is safe and effective in pregnancy. The recommendations from 2012 have changed in two ways: not limiting ITPp to only antenatal care contacts, but additionally recommending IPTp in all pregnant women in malaria-endemic areas [4].
Clinical Relevance
Patients presenting to the clinic should be screened and prompted to discuss current travel plans based on updated CDC traveler guidelines and recommendations. Clinicians should screen all patients for travel during the year, as high malaria transmission rates can occur year around in many countries. This will allow for open communication, better clinician-patient relationship, possible malaria chemoprevention before and during travel, and decreased hospital admissions.
Disclosure of Interest: The authors report no conflict of interest. Ethical review is not necessary, because this is a case report. This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Consent: As this is a case report, consent was obtained for purpose of this paper.
Author Affiliation: All authors took part in the medical management of the patient and edited the final manuscript for submission. All work was performed at The Brooklyn Hospital Center.
Reference
- CDC (2022) Malaria. Accessed September 12 2022.
- CDC. Parasites-Malaria. Accessed September 9, 2022.
- World Health Organization. Malaria. Accessed September 9, 2022.
- World Health Organization. Updated WHO recommendations for malaria chemoprevention among children and pregnant women.
- World Health Organization. (2022) Promoting Malaria Chemoprevention.
- Mbouna AD, Tompkins AM, Lenouo A, Asare EO, Yamba EI, et al. (2019) Modelled and observed mean and seasonal relationships between climate, population density and malaria indicators in Cameroon. Malaria Journal. 18(1): 359.