Smit B Solanki1, Vineet V Mishra2*, M. Anusha3, Rohina Aggarwal4
1Assistant Professor, Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
2Professor and Director, Head of Department of Obstetrics and Gynecology, Institute of Kidney Diseases Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital and Campus, Ahmedabad, Gujarat, India.
3Sr. Resident, Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
4Professor, Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
*Corresponding Author: Vineet V Mishra, Professor and Director, Head of Department of Obstetrics and Gynecology, Institute of Kidney Diseases and Research Center & Dr. H L Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Ahmedabad, Gujarat, India.
Abstract
Complete heart block is a conduction disorder in which there is the absence of conduction of electrical impulses from atria to ventricles, which often needs the placement of a pacemaker. We present a case of successful management of full-term pregnancy with asymptomatic complete heart block without a temporary pacemaker by the combined teamwork of an obstetrician, anesthetist, and cardiologist.
Keywords: Complete Heart Block, pregnancy, pacemaker
Introduction
Complete heart block or Atrioventricular block is a conduction disorder in which there is an interruption in the conduction of the electrical signals from atria to ventricles. Entire heart block (CHB) is estimated to be 1 in 15,000 to 20,000 live births [1]. It may be congenital or acquired. The acquired type is scarce in pregnancy as this is more common after 50 years of age [2]. Hence, the Heart block seen during pregnancy is mostly of congenital variety, which is also very rare, and it is a challenging condition for obstetricians.
Case Report
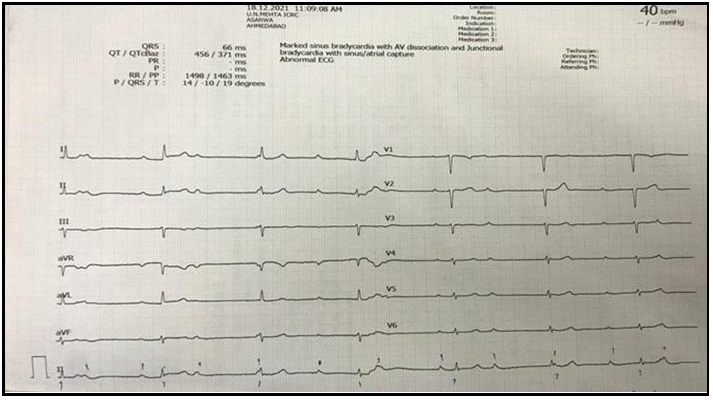
36 years old primigravida whose LMP is on 13-5-2021 and EDD on 20-2-22. During a routine antenatal visit at 6 weeks of pregnancy, her pulse rate was found to be 46 beats per minute. Hence, she underwent ECG, and 2D echo and ECG showed Mobitz type 2 AV block with narrow QRS complex with escape rhythm (Figure 1). 2D ECHO was regular with a left ventricular ejection fraction of 60 %. Holter monitoring was done, which showed complete heart block, and there was no evidence of ventricular tachycardia, supraventricular tachycardia, atrial fibrillation, or atrial flutter. The cardiologist is advised for medical management and needs a pacemaker only if the patient develops chest pain, breathlessness, or giddiness. The patient presented at 32 weeks of pregnancy, and ultrasonography was done, which showed single live intrauterine gestation in a cephalic position with a fetal weight of 2180 grams. Fetal echocardiography was done, which showed no abnormalities. At 36 weeks of pregnancy, the patient was COVID RT-PCR positive, and she was managed conservatively. At 37 weeks of pregnancy, she had labor pains, and Cervi prime gel induction was done twice 6 hours apart, and due to failure of installation, a cesarean section was done. She went through cesarean section under Epidural and Spinal anesthesia, and during cesarean section, her heart rate was 38 / min, BP 110/80 mm of hg, and her urine output was 200 ml. A male baby weighing 2500 g was delivered (Table 1).
Figure 1: ECG
Table 1: Vitals and monitoring of the patient
|
Post operative day |
Pulse |
BP |
Temperature |
Per vaginal bleeding |
Input |
Output |
|
0 |
36 |
100/60 |
98.0 |
Nab |
1500 |
1400 |
|
1 |
42 |
100/80 |
98.8 |
Nab |
1200 + Oral Liquids |
1300 |
|
2 |
38 |
110/70 |
97.8 |
Nab |
1000 + Soft Diet |
2000 |
|
3 |
40 |
120/70 |
99.0 |
Nab |
Full Diet |
4 times |
|
4 |
42 |
120/60 |
98.9 |
Nab |
Full Diet |
5 times |
|
5 |
44 |
110/70 |
98.0 |
Nab |
Full Diet |
5 times |
Emergency drugs, defibrillators, and materials necessary for temporary pacing are kept ready and available during the caesarean section.
Postoperative continuous monitoring of pulse rate, blood pressure, and Spo2 urine output was done. Strict input and output monitoring are done, and information is restricted to prevent fluid overload.
On postoperative day 5, a 2D echo was found normal with a Left ventricular ejection fraction of 55 %, and she was discharged on day 7 and advised on regular cardiology follow-up.
Discussion
Complete heart block (CHB) is characterized by a complete absence of atrioventricular conduction of electrical impulses in which none of the supraventricular motivations are conducted to the ventricles. Perfusing rhythm is maintained by a junctional or ventricular escape rhythm. Typically, the patient will have severe bradycardia with independent atrial and ventricular rates, i.e., AV dissociation [3].
Isolated congenital CHB is a benign condition with bradycardia and narrow QRS complex in ECG, and in patients who are asymptomatic without underlying heart disease, the feto-maternal outcome is mainly favourable [5].
There are three types of Atrioventricular blocks; they are First-degree heart block – there is a delay in the movement of electrical impulses between the atrium and ventricles through the AV node characterized by a prolonged PR interval of more than 0.2 sec on ECG, and there is no skipped or dropped beat.
Second-degree heart block – occurs when the conduction of electrical impulses from the atria to the ventricle is even more delayed compared to first-degree heart block resulting in a skipped beat. It is of two types Mobitz type 1 and type 2. Mobitz type 1 is characterized by progressive, reversible obstruction of the AV node and ECG showing progressive prolongation of the PR interval with a resulting dropped beat. Mobitz type 2 is caused by a sudden, unexpected failure of the His– Purkinje cells to conduct the electrical impulse. In the ECG, the PR interval is unchanged from beat to beat, as there is a sudden failure to perform the signal to the ventricles, resulting in a random skipped beat.
Third-degree Atrioventricular block is a complete heart block in which there is a complete AV dissociation, and there is no relationship between P waves and QRS complexes. The perfusing rhythm is maintained by junctional or ventricular escape beat [6].
Management of CHB in pregnancy depends on the type of heart block and its severity. In asymptomatic women with a response to exercise and Atropine, an increase in heart rate can be managed without a pacemaker. A permanent pacemaker should control second-degree heart block with symptoms and third-degree heart block. A pacemaker is indicated if there are symptoms like chest pain, dyspnea, syncope, palpitations, and also in patients with Q-T interval prolongation, expansive QRS complex, ventricular dysfunction, or heart failure. In a woman without a permanent pacemaker, a temporary pacemaker can be used during pregnancy in patients with Atropine resistant bradycardia and emergency conditions like labor or cesarean section. A patient who is asymptomatic with CHB in pregnancy can be managed without a pacemaker, but temporary pacing facilities and cardiologists should be made available.
Vaginal delivery is not a contraindication in CHB; cesarean is indicated only for obstetrics emergencies.
Spinal combined with epidural anesthesia is safe as it will not aggravate the risk of sudden cardiac arrest.
Perinatal outcome in patients with complete heart block is primarily favourable, and only a few have IUGR, low birth weight, and preterm labor.
Conclusion
A multidisciplinary team of obstetricians, Cardiologists, and Anesthetists should manage a complete heart block during pregnancy. All patients do not need a pacemaker. Regular antenatal monitoring of patients with ECG, 2D ECHO, and cardiologist advice, and with regular follow-up of patients, we can successfully manage a case of CHB. As this is an asymptomatic condition, in all the antenatal patients, ECG must be done, and any syncope attack must be cautiously monitored for early diagnosis and management of CHB.
Declarations
Financial support and sponsorship: Nil.
Conflicts of interest: There are no conflicts of interest.
References
- Perloff's Clinical Recognition of Congenital Heart Disease: 6th Ed. Philadelphia: Elsevier.2011.
- Baghel K, Mohsin Z, Singh S, Kumar S, Ozair M (2016) Pregnancy with complete heart block. J Obstet Gynaecol India. 66(Suppl 2): 623-25.
- Sood R, Kaur H, Mohan G, Nagpal M (2020) Maternal congenital complete heart block in pregnancy: A rare case report. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 9(8): 3502-3504.
- Kumar AU, Sripriya R, Parthasarathy S, Ganesh BA, Ravishankar M (2012) Congenital complete heart block and spinal anaesthesia for caesarean section. Indian J Anaesth. 56(1): 72-74.
- Keepanasseril A, Maurya DK, Suriya Y, Selvaraj R (2015) Complete atrioventricular block in pregnancy: report of seven pregnancies in a patient without pacemaker. BMJ Case Rep. 2015: bcr2014208618.
- Hidaka N, Chiba Y, Fukushima K, Wake N (2011) Pregnant women with complete atrioventricular block: perinatal risks and review of management. Pacing Clin Electrophysiol. 34(9): 1161- 176.